Journal of
eISSN: 2373-4426


Review Article Volume 11 Issue 4
1Hawassa university comprehensive specialized hospital, Ethiopia
2Department of Nursing, College of medicine and health sciences, Wachamo University, Ethiopia
3Department of Nursing, College of medicine and health sciences, Kotebe Metropolitan University, Ethiopia
4School of nursing, College of medicine and health sciences, Hawassa University, Ethiopia
Correspondence: Tomas Yeheyis, School of Nursing, College of Medicine and Health Science, Hawassa University, Ethiopia
Received: July 29, 2021 | Published: December 29, 2021
Citation: Wuletaw G, Birhanu B, Admasu S, et al. Predictors of breastfeeding practice, evidence from mothers of children less than two years of age in southern Ethiopia. J Pediatr Neonatal Care. 2021;11(4):58-64. DOI: 10.15406/jpnc.2021.11.00445
Background: The World Health Organization recognizes that continuous and on-demand breast feeding until two years of age and beyond is essential for health, growth and development of young children, and protection against infectious diseases. In Ethiopia, breastfeeding is promoted by providing information on benefits during ante-natal care and by supporting mothers during post-natal visits.
Objective: To assess the current breast feeding practices and associated factors among mothers of children less than two years of age in Areka town, southern Ethiopia.
Methods: A community-based cross-sectional study was conducted among 286 randomly selected mother-child pairs living in Sothern, Ethiopia, Areka town community. A structured questionnaire was used to collect data on maternal characteristics and assess breast feeding practice. Descriptive summaries were done to present pertinent findings. Multivariate logistic regression analysis was done to establish statistical associations between dependent and independent variables with p <0.05.
Results: From the total of 274 mother- child pairs participated in the study,132 (48.2%) have good breast feeding practice of breast feeding and 142(51.2%) mothers have poor practice of breast feeding. Mothers of age less than 35 practiced appropriate breastfeeding were less likely than mothers with age greater than 35 years. Like wise mothers who are none governmental employed have good breast feeding practice compared to government employees.
Conclusion: The finding in the study showed that magnitude of good breast feeding practice in the study area is lower than the national level. In this study maternal age and maternal occupation have been found to be predictors of breast feeding practice.
Keywords: Breast feeding, knowledge, practice
AMU, Arba Minch University; HSDP, Health Services Development Program; NGO, Non-Governmental Organization; SNNPR, Southern Nation Nationality and People Region; UNICEF, United Nations Children Fund; USA, United States of America; WHO, World Health Organization
Breastfeeding, initiated within the first hour of birth, provided exclusively for six months, and continued up to two years or beyond with the provision of safe and appropriate complementary foods, is one of the most powerful practices for promoting child survival and wellbeing. Improving breastfeeding rates around the world could save the lives of more than 820,000 children under age 5 every year. In addition, it is estimated that improving breastfeeding rates could prevent an additional 20,000 maternal deaths from breast cancer. Observing the statistics in low- and middle-income countries, just 4 per cent, or 1 in 25 babies, are never breastfed.1
Despite extensive evidence that non-breastfeeding is associated with increased mortality and serious morbidity and other long-term adverse health outcomes, efforts at different national levels to increase exclusive breastfeeding and rates of continued breastfeeding have, in general, had only a modest effect.2
On average, infants younger than six months who are not breastfed are 3-4 times more likely to die than those who received any breastmilk. Nearly half of all diarrhea episodes and one-third of all respiratory infections would be prevented by breastfeeding. Protection against hospital admissions due to these diseases is even greater – 72 percent and 57 percent, respectively. Increasing rates of breastfeeding worldwide is a fundamental driver in achieving Sustainable Development Goals by 2030. Breastfeeding plays a significant role in improving nutrition education, and maternal and child health and survival. Longer breastfeeding duration was associated with a 13 percent reduction in the likelihood of overweight and/or obesity prevalence and a 35 percent reduction in type-2 diabetes incidence. Breastfeeding is one of the top interventions for reducing under-5 mortality. To achieve its full impact, breastfeeding should continue up to the age of two years as its protective effect extends well into the second year of life. In children aged 6-23 months, breastfeeding was associated with a 50 percent reduction in deaths.3-5
The Ministry of Health of Ethiopia has also tried to enhance the practice of optimal breast feeding practice by developing training manuals and implementation guidelines on breastfeeding; and incorporated it to the primary health care in line with the health extension program but still the practice is far from the global recommendations.6-19
Demographic and health survey of Ethiopia conducted in 2019 showed that despite WHO recommendations, exclusive breast feeding practice is 59% decreasing as age increases. On the other hand, breast feeding practice until 2 years of age is 76%.20-25
Therefore, this study was conducted to find out breastfeeding mothers adherence to global recommendations on optimal breastfeeding practices and to assess optimal breastfeeding knowledge and practice of mothers who have less than two years of age children as well as factors associated with this in Araka town, South Ethiopia.
Study setting, design, period
The study is conducted in Araka town, which is found 300 km from Addis Ababa the country capital. The town has a general population of more than 60,000. A Community based cross-sectional study design has been employed from April 1 to May, 30, 2018.
Sample size determination
The sample size was estimated using a single population proportion formula assuming prevalence for breastfeeding practice 77% from a study conducted in Jimma, South west Ethiopia,26 with 95% confidence interval (CI) and marginal error (d) of 5%.
After considering 5% non- response rate, the final sample size n= 286.
Sampling procedure and data collection
Simple random sampling technique was used in sampling the study subjects. Out of the total 4 kebeles in the town, 1of them was selected by lottery method. To get the individual sample units (subjects) at household level from the randomly selected Keble, the number of households children less than two years were identified from health extension workers. After that, we entered those house numbers into the computer and generated the required sample size. If there were mothers with more than one child aged less than 2 years in one household, the oldest child will be selected for the study. If mothers had twin children aged less than 2 years, one child was selected by the lottery method. However, in the absence of eligible respondents in a given household, a substitution will be made by an individual in the next household.27-34
Interviewer administered a structured questionnaire by reviewing different researches was used to collect data on maternal socio-demographic characteristics, breast feeding practice, duration, frequency, and related areas. Good practice of breast feeding was asserted when the mother responded more than satisfactory to 10 of the 12 questions used to assess breast feeding practice.35-43
Data processing & analysis
After the data was collected, questionnaires were reviewed and organized by investigators. The data were entered after defining variables and analyzed using SPSS v. 24.0 statistical software. Binary and then multivariate logistic regression was used to decrease the effect of confounding factors. Statistical significance was declared with p-value less than 0.05 for multivariable and 0.25 for bivariate logistic regression. Finally, the result is presented using tables, texts, and other pictorial representations.
Data quality control
The questionnaire was translated to local language and the responses were retranslated to English for consistency. A pretest was done on 5% of the sample and the result was used to correct the wording, spelling, and approach of the questionnaire. Training was given for data collectors on the content of the questionnaire and observational checklist for two consecutive days. After data collection, internal consistency was checked by cross-checking the collected data on every day basis.
Ethical consideration
Ethical clearance was obtained from Arbaminch University, College of Medicine and Health Sciences, Department of Nursing. Permission was obtained from Areka woreda administrative office and informed consent was obtained from individual respondent. The respondents have been told know that they have the right to be involved or not in the study, and that non involvement will not affect the clinical care they might receive.
Socio demographic characteristics of the respondents
Out of the 286 questionnaires that were run, 274 questionnaires were completed making a response rate of 96%. Out of the total respondents in the study 43.4% of mothers were in age group 20-25 years,78.1% of the respondents were married, 45.6.0%,attended secondary and preparatory school, 49.6% were Protestant by religion and 54.7% house wives. From total of 274, 100(36.5%) children were in age group of 6-1 and nearly half 138(50.4%) were male (Table 1).
|
Variable |
|
Frequency |
Percent (%) |
|
age of mother |
15-19 |
21 |
7.7% |
|
20-24 |
100 |
36.5% |
|
|
25-29 |
119 |
43.4% |
|
|
30-34 |
25 |
9.1% |
|
|
>=35 |
9 |
3.3% |
|
|
age of child in month |
0-5 |
92 |
33.6% |
|
6-11 |
100 |
36.5% |
|
|
12-17 |
54 |
19.7% |
|
|
18-24 |
28 |
10.2% |
|
|
sex of child |
Male |
138 |
50.4% |
|
Female |
136 |
49.6% |
|
|
Religion |
Protestant |
136 |
49.6% |
|
Orthodox |
97 |
35.4% |
|
|
Muslim |
12 |
4.4% |
|
|
Catholic |
25 |
9.1% |
|
|
Other |
4 |
1.5% |
|
|
Total |
274 |
100.0% |
|
|
Ethinicity |
Wolayita |
227 |
82.8% |
|
Hadiya |
16 |
5.8% |
|
|
Kamibata |
13 |
4.7% |
|
|
Gamo |
12 |
4.4% |
|
|
Others |
6 |
2.2% |
|
|
Total |
274 |
100.0% |
|
|
Educational |
not attended formal education |
13 |
4.7% |
|
primary school |
104 |
38.8% |
|
|
secondary and preparatory school |
125 |
45.6% |
|
|
College and above |
32 |
11.7% |
|
|
Total |
274 |
100.0% |
|
|
Marital status |
Married |
241 |
78.1% |
|
Divorced |
38 |
13.9% |
|
|
Widowed |
18 |
6.6% |
|
|
Single |
4 |
1.5% |
|
|
Total |
274 |
100.0% |
|
|
occupation |
gov'tal employ |
17 |
6.2% |
|
non gov'tal employ |
18 |
6.6% |
|
|
Merchant |
64 |
23.4% |
|
|
house wives |
150 |
54.7% |
|
|
Student |
25 |
9.1% |
|
|
Total |
274 |
100.0% |
Table 1 Socio-demographic characteristics of mothers of children aged less than 2 years in Areka town, SNNPR Ethiopia, 2018
Maternal and child health service utilization
From the respondents participated in the study, 263(96%) had three or less number of children and 271(98.9%) mothers had ANC follow-up during their last pregnancy. Among those mothers who had ANC follow-up 255(94.1%) mothers had at least two follow-up sessions during the period of pregnancy. Majority of 270 (98.5%) of mothers gave birth to the indexed children in a health institution assisted by a health workers and 273(99.6%) of the paired children in the study had taken vaccination fully or partially (Table 2).
|
Variable |
Frequency Percent(%) |
|
Parity |
<3 263 96.0% >4 11 4.0% |
|
number of children in the house |
<3 263 96.0% >4 11 4.0% |
|
ANC follow up |
Yes 271 98.9% No 3 1.1% |
|
number of ANC follow up |
>2 255 94.1% <2 16 5.9.% |
|
PNC visit |
Yes 272 99.3% No 2 0.7 % |
|
BF counseling before or after child birth |
Yes 271 98.9% No 3 1.1% |
|
place of child birth |
Home 4 1.5% Health institution 270 98.5% |
|
Birth attendant |
Health worker 270 98.5% Untrained birth attendant 4 1.5% |
|
Baby vaccinated |
Yes 273 99.6% No 1 0.4% |
|
|
|
|
Full vaccinated |
Yes 124 45.3% No 150 54.7% |
|
|
Table 2 Health service utilization of mothers and children participated in the study in Areka town, 2018
Breast feeding practice
Breast feeding practices including initiation, exclusive breast feeding on-demand breast feeding frequency, duration, current breast feeding status, positioning, and related practices were assessed. To set the status of general breast feeding practice, those responded to optimal practices on 10 of the questions were labeled as having good practice, while for those less than that, labeled as “poor practice. Based on this assumption, around 133(48.2%) of the mothers have good practice of breastfeeding (Figure 1).
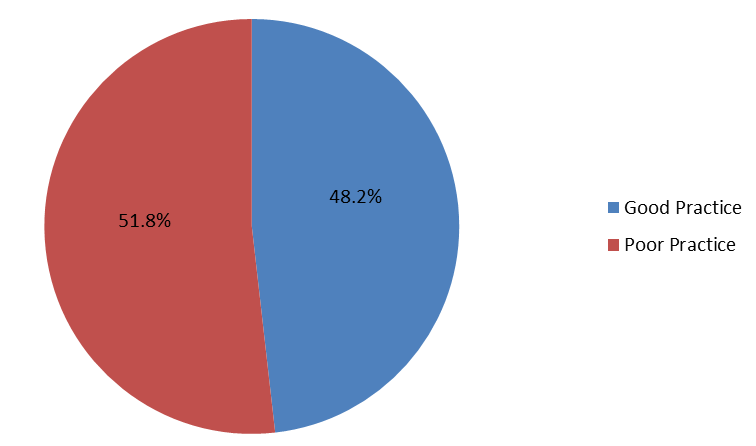
Figure 1 Breast feeding practice among mothers of children aged less than two years, southern Ethiopia, 2018.
Factors associated with the practice of breast feeding
In the bivariate analysis, maternal educational status, maternal employment, religion, maternal age, parity, and received health education were found to be associated with the practice of breastfeeding with a P value of 0.2 or less. When each independent variable was adjusted for other variables, occupation of the mother and age of the mother were found to be statistically significantly associated with breastfeeding practice at a 95% confidence level and a p - value of 0.05. Multivariate logistic regression analysis showed mothers of age20-24 (AOR 0.51 [95% CI 0.25 .510] and mothers of age 30-34 (AOR 0.58 [95% CI 0.28, .69] practiced appropriate breastfeeding less likely than mothers with age > 35years. On the other hand, the odds of good breast feeding practice for non government employees was 15 folds (AOR 15.805[2.664, 93.763] as compared to students (Table 3).
|
Variable |
|
Good practice |
Poor practice |
COR |
95% CI |
AOR |
95%CI |
||
|
lower |
upper |
lower |
upper |
||||||
|
Age of |
15-19 |
15(11.4%) |
6(4.2%) |
1.250 |
0.233 |
6.69 |
.757 |
.089 |
5.804 |
|
20-24 |
47(35.6%) |
53(37.3%) |
0.443 |
0.105 |
1.87 |
.051 |
.025 |
.510 |
|
|
25-29 |
53(40.2%) |
66(46.5%) |
0.402 |
0.096 |
1.68 |
.064 |
.028 |
1.105 |
|
|
30-34 |
11(8.3%) |
14(9.9%) |
0.393 |
0.080 |
1.93 |
.058 |
.020 |
.69 * |
|
|
>35 |
6(4.5%) |
3(2.1%) |
1 |
|
|
1 |
|
|
|
|
Religion |
Protestant |
60(45.5%) |
76(53.5%) |
1 |
|
|
1 |
|
|
|
Orthodox |
52(39.4%) |
45(31.7%) |
1.464 |
0.867 |
2.470 |
1.231 |
.675 |
2.245 |
|
|
Muslim |
5(3.8%) |
7(4.9%) |
0.905 |
0.273 |
2.993 |
1.466 |
.395 |
5.438 |
|
|
Catholic |
13(9.8%) |
12(8.5%) |
1.372 |
0.584 |
3.225 |
.901 |
.327 |
2.485 |
|
|
Other |
2(1.5%) |
2(1.4%) |
1.267 |
0.177 |
9.257 |
1.012 |
.128 |
8.011 |
|
|
Education |
Not attended formal education |
6(4.5%) |
7(4.9%) |
1 |
|
|
1 |
|
|
|
Primary |
51(38.6%) |
53(37.3%) |
1.123 |
0.353 |
3.568 |
11.488 |
1.219 |
108.256 |
|
|
Secondary and preparatory |
53(40.2%) |
72(50.7%) |
0.859 |
0.273 |
2.703 |
10.596 |
1.132 |
99.149 |
|
|
Higher education |
22(16.7%) |
10(7%) |
2.567 |
0.684 |
9.628 |
12.865 |
1.137 |
145.578 |
|
|
occupation |
Government employ |
12(9.1%) |
5(3.5%) |
7.600 |
1.894 |
30.499 |
9.274 |
1.531 |
56.175 |
|
Non-government employ |
7(5.3%) |
11(7.7%) |
2.015 |
0.539 |
7.538 |
15.805 |
2.664 |
93.763 * |
|
|
Merchant |
38(28.8%) |
26(18.3%) |
4.628 |
1.628 |
13.155 |
10.998 |
2.747 |
44.035 |
|
|
House wife |
69(52.3%) |
81(57%) |
2.698 |
1.020 |
7.133 |
5.181 |
1.402 |
19.149 |
|
|
Student |
6(4.5%) |
19(13.4%) |
1 |
|
|
1 |
|
|
|
|
Health education |
Satisfactory |
113(85.6%) |
112(78.9%) |
0.628 |
0.334 |
1.180 |
.480 |
.220 |
1.050 |
|
Un-Satisfactory 19(14.4%) 30(21.1%) 1 1 |
|||||||||
Table 3 Factors associated with breastfeeding practice among mothers of children less than two years, Areka town, Southern Ethiopia, 2018
This study assessed breastfeeding practices, knowledge, and factors associated with breastfeeding in mothers who have less than two years children in the community of Areka SNNPR, Ethiopia. Findings of the study showed that less than half (48.2%) of mothers have good practices on breast feeding. This result is higher than study in Jimma 28% (22).This might be due to currently in Ethiopia both urban and rural HEWs were trained by the help of NGO as well as governmental organization on area particularly optimal breastfeeding practices and how to increase maternal knowledge towards benefit of breast feeding were included like breastfeeding during maternal and child sickness and frequency of eating food during lactation.
On the contrary, the finding in this study(48.2%) is less than the national breast feeding practice level until 2 years of age which is 76%. This might be because the study is done in one of the rural areas in the country where health information dissemination is not adequate. Beyond that, the national figure is an average of findings from different corners of the country but may not address each kebele in the country.
Mothers of age 20-24 (AOR 0.51 [95% CI 0.25, 1.010] and mothers of age 30-34 (AOR 0.58 [95% CI 0.28, 1.105] practiced appropriate breastfeeding less likely than that of mothers with age>35. This may be due to as those mothers with age >35 are more experienced probably multi gravida and mothers at age group from 20-24 and 30-34 are youngsters will less experience and beyond that most of mothers in this age group are busy either by work or social interation and myths in the community regarding continued breast feeding. Hence, this might have contributed to decreased breast feeding practice.
Likewise, maternal occupation was significantly associated with breastfeeding practice. Mothers who are none governmental employed are 15 times more likely to have good breast feeding practice AOR 15.805(2.664, 93.763) as compared to students. Employment of the mother may be expected to enhance accessibility of the household to income, which may in turn have a positive effect on the nutritional status of the child. This may be expected because such income is more likely to be controlled by the mother and used to improve children’s nutritional status. However, it may also be argued that employment of the mother may have a negative effect on children’s nutritional status by reducing both infants’ access to breastfeeding and time spent on childcare due to long hours spent at work and classes’ and the absence of day care stations at work and school for those mothers. Some empirical studies show that the mothers of the most malnourished children work outside their home.
The findings in the study showed that the magnitude of good breast feeding practice in the study area is lower than the national level. In this study, maternal age and maternal occupation have been found to be predictors of breast feeding practice. This study indicates the need for child day care centers at work places. In addition it shows that primi gravida mothers and those below the age of 35 needs a special attention regarding practicing breast feeding optimally.
The authors are grateful for the data collectors and study participants. There was no funding source for the study. Expenses are covered by the authors.
Ethics approval and consent to participant
The study protocol was ethically approved by the Ethical Review Board (IRB) of Arbaminch University, College of medicine and Health Sciences. Official letter was written to Areka woreda Administrative office. The study posed a low or no risk to the study participants. The study did not involve any invasive procedures. Moreover, the confidentiality of information was guaranteed by using code numbers rather than personal identifiers and by keeping the data locked.
Not applicable.
The datasets used and/or analyzed during the current study is available upon request from the corresponding author and Co- authors.
The authors declare that they have no competing interests.
There is no source of funding for this research. All costs were covered by the authors.
SA, GW and BB conceived and designed the study and analyzed the data. ZS and TY assisted with the design conception, advising and reviewing the manuscript. FE, AB, BW, GK and DH prepared the manuscript.

©2021 Wuletaw, et al. This is an open access article distributed under the terms of the, which permits unrestricted use, distribution, and build upon your work non-commercially.