Journal of
eISSN: 2373-4426


Proceeding Volume 2 Issue 6
Al Noor Hospital, UAE
Correspondence: Emad Azer, Al Noor Hospital, UAE, Tel 972000000000
Received: July 17, 2015 | Published: September 9, 2015
Citation: Azer E (2015) Post Delivery Antibiotics. J Pediatr Neonatal Care 2(6): 00101. DOI: 10.15406/jpnc.2015.02.00101
The need to know which babies need antibiotics after delivery and which are not is the main goal of this lecture
Definition
It is a clinical syndrome of systemic illness accompanied by bactremia occurring in 1st month of life.
Incidence
Range from 1-8/thousand & reaches 13-27/thousand for B.W < 1.5kg. The mortality rate is 13-25% & higher rates are seen in premature.
Patients meeting any of the following criteria Should receive intrapartum prophylaxis:
If patient meets none of stated criteria, intrapartum prophylaxis for GBS is NOT indicated. This includes the Following circumstances
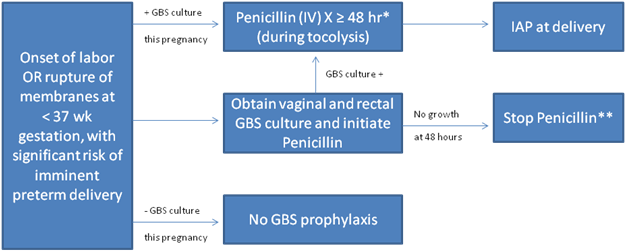
* Penicillin should be continued for a total of at least 48 hours, unless delivery occurs sooner. For women who are GBS culture positive, antibiotic.
** If delivery has not occurred within 4 wk, a vaginal and rectal GBS screening culture should be repeated, and the patient should be managed as mention, based on the result of the repeat culture.
* Penicillin should be continued for a total of at least 48 hours, unless delivery occurs sooner. For women who are GBS culture positive, antibiotic.
** If delivery has not occurred within 4 wk, a vaginal and rectal GBS screening culture should be repeated, and the patient should be managed as mention, based on the result of the repeat culture.
The initial diagnosis of sepsis is a clinical one & we should start treatment before results of culture are available. Clinical sign & symptoms are non specific and D.D is broad including RDS, metabolic diseases, Blood diseases, CNS diseases, Cardiac disease s& other infection eg. Torch.
Sign and Symptoms include
Target audience
Pediatrics, Obstetrics, GP and other related health care professionals.
Before Prescribing Antibiotics to the newborn we have to ask ourselves some Questions
Are there any maternal risk factors for sepsis: This include: African Race, Malnutrition, Maternal GBS colonization, history of STD, Age < 20 years, low socioeconomic status, asymptomatic bacteraemia and previous history of GBS infection.
Are there intrapartum risk factors for sepsis: This include: Prom>18h, chorioamnionitis (fetal tachycardia, uterine tenderness, purulent amniotic fluid, unexplained maternal temp.>38) maternal fever, Perinatal asphyxia (AP at 5 min<6) DDL.
Are there neonatal risk factors for sepsis: This include: Male sex, twin birth, prematurity, LBW and Galactosemia.
When Membranes Ruptured: Prom>18h~ à high risk.
Fetal condition: Fetal tachycardia>160 also intrauterine monitoring for prolonged time
à high risk of GBS infection.
Did the mother has cerclage for cervical incompetence: This ↑ high risk of sepsis
Are there any sign of sepsis: Signs of Neonatal Sepsis include Apnea, bradycardia, temp instability (high & low) Feeding intolerance, tachypnea jaundice, cyanosis, poor peripheral perfusion, hypo Glycemia, lethargy, poor sucking, high gastric aspirate and irritability. Also tachycardia, shock, vomiting, rash, abdominal distension, seizures and hepatomegaly.
Did the mother have epidural: It ↑ intrapartum fever and the needs for investigations and treatment but not risk of infection.
Did the mother tested for GBS and received Antibiotics?: D.D We classify neonates for those with ↑ risk of sepsis and those with low risk of sepsis.
Cardiac
GIT
Metabolic
Respiratory
Mostly we know which patient who needs sepsis work up and antibiotics but there are certain situations we will discuss it now.
Start Antibiotics
When to discontinue antibiotics
None.
The authors declare that there are no conflicts of interest.
None.

©2015 Azer. This is an open access article distributed under the terms of the, which permits unrestricted use, distribution, and build upon your work non-commercially.