Journal of
eISSN: 2373-4426


Research Article Volume 10 Issue 3
Department of Paediatrics, Indira Gandhi Government Medical College, India
Correspondence: Shamama Subuhi Mohammed Zubair, Department of Paediatrics, Indira Gandhi Government Medical College, Nagpur, 103,C wing, Aman Pride Appartment,Katol Road, Nagpur -440013, India
Received: February 09, 2020 | Published: June 29, 2020
Citation: Zubair SSM. Outcome of neonatal thrombocytopenia in tertiary care NICU. J Pediatr Neonatal Care. 2020;10(3):92-96. DOI: 10.15406/jpnc.2020.10.00418
Thrombocytopenia is one of the commonest haematological disorders in the neonatal period, affecting up to a third of those admitted to neonatal intensive care units. It is well recognized that many fetomaternal and neonatal conditions are associated with thrombocytopenia. The majority of episodes of neonatal thrombocytopenia are relatively mild, self-limiting and of short duration but it may cause severe morbidity & mortality due to severe complication like IVH. Methods & material: 140 Newborn admitted in tertiary care NICU were selected to find out outcome and etiology of neonatal thrombocytopenia. Detail maternal history and neonatal physical examination done and Neonates were followed for outcome, relevant investigation done according to cases. Result: Out of 140 neonates 63 neonates had thrombocytopenia (45%).42.8% neonates were premature out of which 63.3% had thrombocytopenia. Other neonatal risk factor for thrombocytopenia are sepsis 38 (74.5%), SGA/IUGR 28(80%) and NEC 9(100%). Maternal risk factor for thrombocytopenia are eclampsia81.8% and infection during pregnancy 72.72%. 95.5 % of all study population were discharged.4.5 % cases of whole study population didn’t survive. 4.54% of mild, 9.09% of moderate and 60 % of severe thrombocytopenic babies didn’t survive. Conclusion: Bleeding manifestations i.e. mucosal, cutaneous and intracranial bleed were significantly associated with severe thrombocytopenia. 60% of mortality was found in severe thrombocytopenic group. Thus, severe thrombocytopenia was found to be a predictor of poor outcome in sick neonates of NICU.
Keywords: neonatal thrombocytopenia, maternal eclampsia, prematurity, sepsis, outcome
IUGR, intra uterine growth retardation; SGA, small for gestational age; NEC, necrotising enterocolitis; PIH, pregnancy induced hypertension; IVH, intra ventricular haemorrhage
Thrombocytopenia is one of the commonest haematological disorders in the neonatal period, affecting up to a third of those admitted to neonatal intensive care units. Most cases of thrombocytopenia in babies admitted to NICUs are discovered incidently. The majority of episodes of neonatal thrombocytopenia are relatively mild, self-limiting and of short duration but some times It can cause mortality & morbidity due to severe complication like IVH. The incidence varies greatly depending upon population studied from <1% in healthy term babies to around one third of neonates admitted to NICU.1 Thrombocytopenia is defined as platelet count <1.5 lakh/cmm regardless of gestational age. Degrees of thrombocytopenia can be further subdivided into mild (platelet count 100,000 to 150,000/µl), moderate (platelet count 50,000 to 99,000/µl) and severe (platelet count <50,000/µl).2 Prematurity, sepsis, hypoxia, intrauterine growth retardation, and disseminated intravascular coagulation & maternal eclamsia play an important role in the etiology of NT. Hence we aim to study the profile of neonatal thrombocytopenia in our NICU so that we can know morbidity pattern of neonatal thrombocytopenia.
This is prospective observational study, hospital based study carried out in department of Paediatrics in Indira Gandhi Govt medical College & hospital, during period of January 2018 to June 2019 after acceptance from institutional ethical committee. In this study, a sample of 140 of all the newborns admitted in NICU during this time period except for the ones admitted for observation were selected. Prior written Informed Consent was obtained from the parents or available relatives of each neonate. All maternal aspects like maternal age, parity, prenatal events like leaking/bleeding > 18 hrs, maternal illness like PIH, eclampsia, hospital admission, maternal drug intake like aspirin, antiplatelet drugs, bad obstetric history, Rh-isoimmunization, mode of delivery suggesting thrombocytopenia was noted down. In all enrolled newborns detailed history regarding presenting symptoms and physical examination of each neonate was done, neccesary investigation were done accordingly and followed up for outcome. Gestational age was calculated by New Ballard score.
INVESTIGATIONS: CBC (Hb, TLC, DLC, Platelet count, absolute neutrophil count) C- reactive proteins (CRP). Micro-Erythrocyte sedimentation rate (m-ESR), Blood culture and sensitivity, X-ray chest, USG abdomen, LP, Urine routine done if needed.
Definitions of importent terms:
Study protocol
This is observational prospective study carried out in 140 neonates. Following are the results
Out of 140 neonates 63 neonates had thrombocytopenia, hence prevalence of thrombocytopenia was 45 % (Tables 1&2) (Figures 1&2).
Material Risk Factor |
Number |
Thrombocytopenia |
No Thrombocytopenia |
P value |
Elderly Primigravida |
12 |
6 |
6 |
0.71 |
Chronic Illness Drug Prgnancy |
21 |
8 |
13 |
0.49 |
Infection during Pregnancy |
11 |
8 |
3 |
0.015 |
PIH |
39 |
19 |
20 |
0.588 |
ECLAMPSIA |
11 |
9 |
2 |
0.02 |
GDM |
2 |
1 |
1 |
0.99 |
APH |
12 |
6 |
6 |
0.71 |
Auto Immune Disease |
2 |
1 |
1 |
0.99 |
Table 1 association between maternal risk factors and thrombocytopenia.
Fetal Risk Factor |
Thrombocytopenia |
No Thrombocytopenia |
P value |
SGA/IUGR (35) |
28(80%) |
7(72%) |
0.00 |
Preterm (60) |
38(63.33%) |
22(36.44%) |
0.0001 |
Birth Asphxia (13) |
8(61.53%) |
5(39.47%) |
0.2 |
Respiratory Distress Syndrome (10) |
6(60%) |
4(40%) |
0.32 |
Meconium Aspiration Syndrome (12) |
6(50%) |
6(50%) |
0.71 |
Sepsis(51) |
38(74.5%) |
11(25.5%) |
0.00 |
NEC (9) |
9(100%) |
0 |
0.001 |
Table 2 Association between neonatal risk factors and thrombocytopenia

Figure 1 Among all maternal risk factors, eclampsia was common risk factor for thrombocytopenia 81.81%.( p value = 0.02 ) followed by history of infections during pregnancy 72.72 %. It was statistically significant. (p value = 0.015 ).
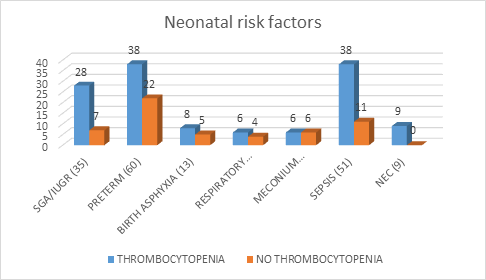
Figure 2 Amongst neonatal risk factor IUGR (p value 0.00), prematurity (p value 0.0001), sepsis (p value 0.00) and NEC (p value 0.001) were statistically significant for thrombocytopenia.
Severity of neonatal thrombocytopenia
Out of 140 neonates, Mild thrombocytopenia was observed in 46(32.85%) neonates, moderate thrombocytopenia in 12(8.57%) & severe thrombocytopenia in 5(3.57%) (Table 3). Amongst cases of severe thrombocytopenia, 60 % had intraventricular haemorrhage and 100 % neonates has GI bleeding. It was statistically significant (p value- < 0.00). Those presenting with bleeding manifestions i.e. GI bleed (8), of which 5 neoates had severe thrombocytopenia i.e.100 %. It was statistically significant (p value-0.000). Out of 140 neonates 135 (96.4 %) neonates were discharged. 5 (3.7%) neonates were died, of which 1 (2.1%) of mild, 1 (8.3%) of moderate and 3(60%) were having severe thrombocytopenia. The mortality in babies with severe thrombocytopenia was high (p value =0.03) which was statisticaly significant.
Neonatal thrombocytopenia |
GI bleed |
Intraventricular haemorrhage |
Discharge |
Death |
Normal(77) |
2 |
0 |
77 |
0 |
Mild(46) |
1 |
0 |
45 |
1 |
Moderate(12) |
2 |
0 |
11 |
1 |
Severe(5) |
5 |
3 |
2 |
3 |
Total(63) |
10 |
3 |
135 |
5 |
Table 3 Neonatal thrombocytopenia and it’s complications & outcome according to severity
This study is done on 140 neonates in a tertiary care NICU. The prevalence of neonatal thrombocytopenia was 45.0 %. Sonam nadyal et al.,3 the prevalence of neonatal thrombocytopenia was 63.8%. Among all maternal risk factors, PIH was seen to be more commonly associated with thrombocytopenia.. All babies who had maternal risk factor as eclampsia had thrombocytopenia which was statisticaly significant (81.81% ) followed by history of infections during pregnancy which was 72.72 %. Keerthi tripathi et al.,4 showed that PIH was the commonest maternal risk factor. 27(13.5%) babies had PIH as the maternal risk factor and it was associated with severe thrombocytopenia. Most common causes of thrombocytopenia in neonates was of prematurity (63.3%) and sepsis (74.5%) followed by IUGR (80%), NEC (100%). Eslami Z et al.,5 recorded neonatal sepsis and intra uterine growth retardation as important causes of thrombocytopenia. Sonam Nandyal et al.,3 showed leading causes neonatal thrombocytopenia include prematurity, sepsis, respiratory distress syndrome, birth asphyxia, meconium aspiration syndrome, hyperbilirubinemia and intra-uterine growth retardation.
In present study, mild thrombocytopenia was observed in 32.85 % neonates, moderate thrombocytopenia in 8.57 % & severe thrombocytopenia in 3.57 %. Khalessi et al.,6 found 43.5% had mild thrombocytopenia, 25.8% had moderate thrombocytopenia, and 24.1% had severe thrombocytopenia. Jeremiah et al.,7 observed that amongst thrombocytopenic neonates 39.4% were mild, 12.1% moderate and 1.5% severe. Amongst neonates of severe thrombocytopenia, 60 % had intraventricular haemorrhag. Von Lindern JS et al.,8 found that 12% of babies with neonatal thrombocytopenia developed IVH. Beiner et al.,9 showed strong correlation between neonatal thrombocytopenia and IVH. Amongst babies presenting with bleeding manifestions i.e. GI bleed (7), mucosal bleed (5), malena (4), and petechiae (5) had severe thrombocytopenia i.e.100 %. Similar results were found in other studies. Khalesssi et al.,6 showed 6.5% had gastrointestinal bleeding. Patil et al.,10 showed that mucosal bleeding was significantly associated with thrombocytopenia. In this study out of 140 neonates the mortality was in 5(3.7%) of which 3 babies were having severe thrombocytopenia. Patil reported that mortality rate was very high 37%, among the severely thrombocytopenic neonates. Bonifacio L et al.,11 observed that the mortality rate was 16.7%, 32.4% and 45.8% in neonates with mild, moderate and severe thrombocytopenia, respectively. In our study, 95.5 % of all study population showed improvement.4.5 % cases of whole study population couldn’t survive. All non thrombocytopenic cases improved.4.54% of mild, 9.09% of moderate and 60 % of severe thrombocytopenic babies died. Patil et al.,10 showed that mortality rate was very high, 37%, among the severely thrombocytopenic neonates while it was only 3.72% and 3.92% respectively in the mild to moderate and no thrombocytopenia groups.
Neonatal thrombocytopenia is one among most common hematological abnormality encountered in NICU. The prevalence of neonatal thrombocytopenia was 45%. The most common etiology associated with thrombocytopenia were sepsis and prematurity followed by IUGR and NEC. Amongs the maternal factor eclampsia was significantly associated with neonatal thrombocytopenia. Clinical signs and symptoms associated with neonatal thrombocytopenia especially severe thrombocytopenia were gastrointestinal and mucocutaneous bleeding, petechiae, malena and IVH. Bleeding manifestations i.e. mucosal, cutaneous and intracranial bleed were significantly associated with severe thrombocytopenia. 60% of mortality was found in severe thrombocytopenic group. Thus, severe thrombocytopenia was found to be a predictor of poor outcome in sick neonates of NICU. The most significant conclusion of study was severe thrombocytopenia can be used as a prognostic indicator in sick neonates.
None.
The authors declare there are no conflicts of interest.
None.

©2020 Zubair, et al. This is an open access article distributed under the terms of the, which permits unrestricted use, distribution, and build upon your work non-commercially.