Journal of
eISSN: 2373-4426


Research Article Volume 7 Issue 4
Pediatric Surgery University, All India Institute of Medical Sciences, India
Correspondence: Kashish Khanna, Senior Research Associate, Pediatric Surgery University, All India Institute of Medical Sciences, New Delhi-110029, India, Tel 91-9811866150
Received: January 01, 1971 | Published: December 15, 2017
Citation: Khanna K, Khanna V, Kour H (2017) Megacystis Megacolon Intestinal Hypoperistalsis Syndrome: A Rare Entity! J Pediatr Neonatal Care 7(4): 00297. DOI: 10.15406/jpnc.2017.07.00297
Megacystis microcolon intestinal hypoperistalsis syndrome is a well established clinical entity; a variant of intestinal neuronal disease spectrum. However, megacystis associated with megacolon and intestinal hypoperistalsis is generally unheard of. We report a case of 7‒day‒old baby boy who presented to us with massive abdominal distension, bilious vomiting and non passage of stools since birth. The radiological features were suggestive of neonatal intestinal obstruction. The child was managed for 25 days before he was gradually diagnosed as a case of megacystis associated with megacolon and intestinal hypoperistalsis. The interesting course of his presentation, exploration, re‒exploraton and diagnosis has been discussed in detail. The literature was reviewed for similar cases. Megacystis‒megacolon‒intestinal hypoperistalsis syndrome, commoner in male infants, presents similar to variants of Hirschsprung’s disease. Intestinal biopsies show normal ganglion cells; establishing nutrition (enteral or parentral) and intermittent catheterization remains the cornerstone of its management. Survival though dismal; multi‒visceral transplantation holds potential for improvement.
Keywords:Megacystis, Megacolon, Intestinal hypoperistalsis, Intestinal neonatal obstruction, Intestinal neuronal disease, Microcolon
MMIHS, Megacystis‒Microcolon‒Intestinal‒Hypoperistalsis syndrome; MMH, Megacystis Megacolon Intestinal Hypoperistalsis; TPN, Total Parentral Nutrition; HD, Hirschsprung’s Disease; IND, Intestinal Neuronal dysplasia
Megacystis microcolon intestinal hypoperistalsis syndrome (MMIHS) is now a well established entity.1,2 Also known as Berdon syndrome.1], it is characterized by massive abdominal distension caused by a largely dilated non obstructed urinary bladder, microcolon and decreased or absent intestinal peristalsis. Isolated cases of congenital megacystis.3,4] and microcolon without megacystis.5] have also been reported as have cases of idiopathic megacolon.6 Megacolon alone as a variant of Hirschsprung’s disease (HD) has presented in various forms.7 We report an interesting case of a neonate that turned out to be magacystis associated with megacolon and intestinal hypoperistalsis; a less heard entity.8‒10
History and examination findings
A 7‒day‒old baby boy delivered normally to a 29‒year‒old multipara female, was admitted with the complaints of non passage of meconium since birth, increasing abdominal distension for 4 days and a history of bilious vomiting at birth. At presentation the child’s general condition was poor. He was dehydrated with a heart rate=130/min and a delayed capillary refill time. His abdomen was grossly distended with overlying shiny skin and prominent visible veins. On rectal stimulation by an infant feeding tube, meconium staining was noted. An erect X‒ Ray of the abdomen showed multiple air‒fluid levels (Figure 1). The child received supportive care, oxygen by hood, intravenous fluids and antibiotics. Naso‒gastric (NG) tube decompression yielded bilious aspirate. On urinary catherization, 430ml of clear urine was aspirated at a single time. Child was stabilized and taken up for exploration in view of neonatal intestinal obstruction.
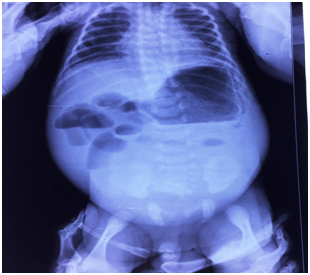
Figure 1 X‒ray abdomen erect of a 7 day baby boy showing multiple dilated loops with air‒fluid levels suggestive of intestinal obstruction.
Exploratory laparotomy
On exploration, the peritoneal cavity was filled with bile and meconium. There were 2 perforations in the transverse colon; 1x1.5cm and 1.5x2cm in size about an inch apart on the ante‒mesenteric border (Figure 2). The descending colon and sigmoid colon were healthy, patent and of dilated caliber than normal intestinal colon. A thorough peritoneal lavage followed by resection of unhealthy perforated bowel segment was performed. A right transverse colostomy and a distal mucus fistula near the splenic flexure were fashioned. Of note was a huge flabby distended bladder reaching up till the epigastric region (Figure 3). Multiple biopsies were sent; rectal biopsy from the peritoneal reflection, resected colon specimen, proximal and distal stomal biopsies. Peritoneal drains were placed.
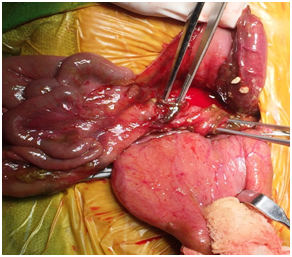
Figure 2 Bladder retracted anteriorly, dilated transverse colon with 2 perforations (forceps inserted) about an inch apart.
Postoperative course
Postoperatively, the baby was kept stable on intravenous fluids and antibiotics were started according to culture reports. The stoma did not function till the 9th postoperative day despite adequate gut stimulation (proximal and distal stomal washes, gavage feeds, rectal washes, prokinetics including metclopramide and erythromycin). The child was maintained on total parentral nutrition (TPN) since repeated attempts on establishing oral feeds were rendered unsuccessful and the child vomited oral feeds. The postoperative X‒ Ray abdomen showed an enlarged gastric shadow suggestive of persistent gastric dilatation and absence of distal gas (Figure 4).
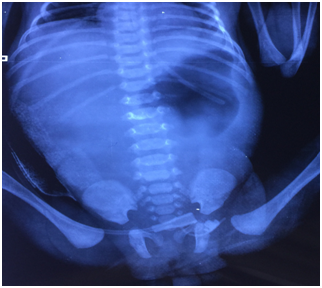
Figure 4 X‒ray abdomen (post operative day 9) showing large gastric shadow with no distal gas suggestive of decreased or absent motility.
Histopathology
The histopathology reported presence of normal ganglion cells with normal Acetyl cholinesterase staining seen in all sent specimens.
Re‒exploration
The child was taken up for re‒exploration with the aim of establishing a route for entral feeds. A pre‒gangrenous necrotic patch was noticed near the greater curvature of stomach. The rest of the bowel was however healthy. The patch was excised, sent for biopsy and a gastrostomy made. The stoma was revised.
Further hospital course
The child was restarted on supportive treatment including TPN and antifungals were added. Gastrostomy feeds were started on the 4th postoperative day. The stoma did not start functioning despite all efforts and gut stimulation. The second histopatholgy again reported the presence of normal ganglion cells in the intestinal specimen and chronic inflammatory changes and necrosis in the gastric biopsy. The child’s parents discontinued further treatment after a hospital stay of 26 days and left against medical advice.
The typical presentation of bilious vomiting, massive abdominal distension, non passage of meconium since birth, meconium staining of catheter on rectal stimulation and X‒Ray findings of neonatal intestinal obstruction are akin to neonatal HD. Allied disorders of HD describe such conditions that clinically resemble HD despite the presence of normal ganglion cells in terminal rectum.11 Also known as Pseudo HD.12,13], these can be distinguished from HD based on the histipathological findings.13 Puri et al..7 ,14] called this group as variants of HD that included 4 disorders:intestinal neuronal dysplasia(IND); isolated hypoganglionosis; internal anal sphincter achalasia; and MMIHS.14 Our case presented with the typical clinical features suggestive of neonatal intestinal obstruction. The initial X‒ray abdomen did not show the presence of pneumoperitoneum. However a decision to explore was taken and a serial pre‒operative X‒Ray abdomen could not be obtained after stabilization.
Megacystis‒Megacolon‒Hypoperistalis (MMH) is probably a variant of the MMIHS. Berdon et al..1] described MMIHS in 5 newborn girls in 1976. In a review on MMIHS conducted on 227 cases reported from 1976 to 2011.2], a clear preponderance for female infants was found (female‒70.6%; male‒29.4%). However the association of megacolon with megacystis in MMH has been previously reported in a male infant.8] like in our case.
Unlike MMIHS that is characterized by massive abdominal distension caused by a large, dilated, non‒obstructed bladder; microcolon with malrotation; and decreased or absent intestinal peristalsis.15], MMH is associated with megacolon with or without malrotation.10
Many surgical interventions that included gastrostomy, jejunostomy, ileostomy, cecostomy, segmental resection of jejunum and ileum, adhesiolysis and internal sphincter myectomy, and vesicostomy have been reported in 115 patients of MMIHS.2 Despite these surgeries, the reported survival rate was 19.7% that too with partial or TPN support.2 Even in cases of MMH, despite all attempts at oral or entral nutrition, the case reported by Akel et al..8] survived for 14 months due to TPN support. Prato et al..10] reported a similar case of a 2‒year‒old girl who presented with signs of bowel obstruction and was evaluated to have a megacolon (diffuse IND) with megacystis. She managed to survive till 8‒years of age with the aid of various repeated surgical procedures which also included total colectomy. Our case was managed on similar lines with supportive care, TPN, repeated exploration and multiple attempts at establishing oral or entral feeds with all kinds of elemental formula preparations and prokinetic drugs. The dysfunctional/adynamic bladder was managed by intermittent catheterization.
In MMIHS, intestinal biopsy shows normal ganglion cells and a normal pattern of Acetyl cholinesterase staining.16 Similar to this in MMH multiple biopsies from the ileum, rectosigmoid, and appendix had presence of normal ganglia without any neuronal dysplasia or a myopathy.8 Histochemical staining showed normal acetyl cholinesterase and neuron‒specific enolase.8 In our case also multiple biopsies from the stomach, resected colon, stomal site and the rectum showed the presence of normal ganglion cells.
Survival in cases of MMH is dismal. However hope for an improved outcome lies in multi‒visceral transplantation for this condition; as has been reported for MMIHS.17 The bladder function may still require intermittent catherization. Till then, maintaining nutrition by enteral or parentral route is the key to survival. Multiple repeated surgical interventions may not reap better results.
Megacystis may be associated with megacolon and intestinal hypoperistalsis. More commonly seen in male infants, its presentation may be similar to HD. Intestinal biopsies may show normal ganglion cells and histochemical staining pattern. Management should concentrate on establishing parentral or enteral nutrition. Clean intermittent catheterization is mandatory to decompress the dysfunctional bladder. Survival is dismal but can be improved by maintaining nutrition till multi‒organ transplantation is planned.
Proper consent for management of patient and publication of patient related material was taken from the parents at the time of hospital stay by the authors.
None.
Nil.
The efforts of the parents and attendants of the patient are highly appreciated. The efforts and cooperation of the doctors and staff of the department of Pediatric Surgery at Vardhaman Mahavir Medical College and Safdarjang hospital, New Delhi during the management of the case is acknowledged.

©2017 Khanna, et al. This is an open access article distributed under the terms of the, which permits unrestricted use, distribution, and build upon your work non-commercially.