Journal of
eISSN: 2373-4426


Clinical Case Volume 15 Issue 1
1Neonatal Intensive Care Unit, UROS Clinic, Colombia
2Pediatric Service, UROS Clinic, Colombia
Correspondence: Dr. Saul Hernando Vallejo Chaves, Pediatrician, Universidad Surcolombiana, Breastfeeding Consultant, Clinical Researcher, Vice President of the Ethics and Research Committee, UROS Clinic, Neiva, Huila, Colombia, Tel +573105568460, Fax +573105568460
Received: February 10, 2025 | Published: February 27, 2025
Citation: Hernando VCS, Sandra ST, Omaira GM, et al. Median cervical cleft: A rare disease: Case report in a newborn. J Pediatr Neonatal Care. 2025;15(1):61-63. DOI: 10.15406/jpnc.2025.15.00585
Congenital midline cervical cleft is a rare condition, with an incidence of less than 2% among congenital malformations. Its etiology is related to defects in the fusion of the first branchial arches. The clinical findings of a fibrous cord with skin involvement in the midline cervical region allow for an early and accurate diagnosis in most cases without requiring further studies. It was fully described by Ombreadanne in 1946. Although it can be followed in the first day of life and the diagnosis is typically made on the basis of the clinical presentation of the action of the lesion at birth, the cleft may not appear very striking in a newborn. When observed at birth, the characteristic features are a defect in the ventral area of the neck with a subcutaneous fibrous cord and a nipple-like projection at the top and a sinus or fistulous tract at the lower end of the defect. The defect is located between the mental areas superiorly to the suprasternal notch, inferiorly with variable length and width. Most cases are sporadic and it is more common in Caucasian girls.
Keywords: congenital anomaly, branchial arch, middle cervical cleft, newborn, UROS clinic
Full-term newborn, 38 weeks gestational age, 4 days old, born vaginally without complications, spontaneous neonatal adaptation, Apgar 8-9-10, Silverman Anderson 0 points, no respiratory distress, anthropometry weight 3,385 g height 50 cm, head perimeter 34.5 chest perimeter 33 abdominal perimeter 33, female sex, blood classification mother or positive newborn or positive, There was no family history of congenital defects and both parents were also healthy. On examination, a vertical mucous surface was observed in the midline on the anterior part of the neck extending from below the mental process of the mandible to the supra sternal area without skin cover. The defect was 3 cm vertically long and 0.5 cm wide. A nipple-like projection was observed at the top of the defect and there was a sinus at the bottom of the defect above the manubrium, so the patient was transferred to the neonatal intensive care unit at Clínica UROS for comprehensive management. The newborn remained in stable condition, thermodynamically compensated with cardiorespiratory sufficiency, with adequate respiratory pattern and saturations, without requiring supplemental oxygen. From a hemodynamic point of view, there was adequate distal perfusion with good urinary output. An echocardiogram was requested as a complementary study due to midline defects, reporting good left ventricular systolic and diastolic function, physiological tricuspid and pulmonary insufficiency, 3.3 mm oval fossa, 8 mm Tapse, without vegetations or ductus. From a gastrointestinal point of view, there was adequate suction and oral tolerance, with no difficulty sucking. Physical examination showed a cleft in the anterior midline of the neck, with no discharge, no infection, no induration. A thyroglossal cyst was ruled out. Further studies were required and a neck ultrasound was performed to exclude an association with other neck abnormalities. Echocardiography and abdominal ultrasound were normal and no other midline defect was found. After being assessed by pediatric surgery, the newborn was referred with a congenital neck injury, a midline cleft, a rare condition with no indication for emergency surgery, but with an indication for early treatment in life to avoid complications. Assessed by maxillofacial surgery considered a 3 cm vertical erythematous outline of possible closure of the central fissure in zone VI of the neck who maintains a search and suction reflex without complications, for which reason an outpatient control was indicated in 1 month by head and neck surgery. Pediatric neurology presents a 3 cm vertical erythematous outline, possible closure of the central fissure in zone VI of the neck, non-productive, non-transfixing, no secretions or bleeding, active, reactive, complete Moro ++, search reflex, palmar plantar prehesion ++ adequately mobilizes the 4 extremities. Due to findings on physical examination and high risk of neural tube malformation, a simple MRI of the cervical, thoracic and lumbosacral spine was indicated, which were performed without alterations. The otorhinolaryngological evaluation confirmed the diagnosis of isolated middle cervical cleft. A clinical follow-up was planned, which will be performed at 6 months of age. Surgical treatment with a Z-plasty will be planned before school age to allow for better extension of the neck and to ensure a functional and aesthetic result. Due to adequate clinical evolution, it is decided to discharge the patient in the company of his parents. Outpatient follow-up will be provided by an outpatient clinic. (Figures 1–3)

Figure 2 Clinical features of congenital middle cervical cleft (CMCC) in our patient. The nipple-shaped upper skin tag, the red, oozing band of atrophic skin from the level below the hyoid bone to the suprasternal notch, and the caudally located sinus tract are evident.
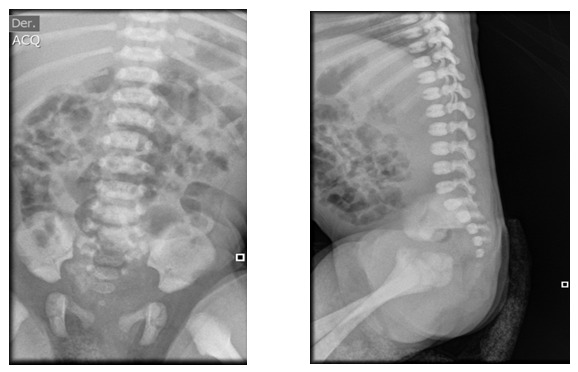
Figure 3 Lumbar spine x-ray technique: AP and lateral projection. Findings: There is no evidence of soft tissue alteration. The lumbar lordosis is preserved and the load-bearing spine is not displaced. The vertebral bodies have normal morphology, height and density according to the patient's age. The intersomatic spaces have normal width. The pedicles, spinous and transverse processes have normal morphology and density. The sacrum and coccyx have a normal anatomical position.
CMCC, with around 100 cases reported in the literature, is a rare congenital anomaly of the anterior neck region.1,2 It can extend in the midline from the mandible to the manubrium and the length and width of the lesion may differ from one child to another. Although the anomaly is mainly observed in females,3 which was reported in our first case in the Southern Colombian region.
The anomaly presents a linear vertical zone of thin, erythematous mucosa at birth. There is often a nipple-like projection at the top and a sinus or fistula at the lower end. Sometimes there is also a fibrous band beneath the mucosal defect. If left untreated in newborns, the midline cord begins to act as an anchor as the baby grows. Therefore, surgical excision has both cosmetic and functional benefits.
Several studies have suggested that there is a predominance of CMCC in the Caucasian population, mainly in women, with a F:M ratio of 2:1.4,5 Reviewing the current literature, we found that this is the first case report in a female newborn in the southern Colombian region, which is why it is of great importance to follow up the patient and subsequently perform the surgical management which was proposed by the pediatric surgery group around 12 months of life.
Several theories are suggested for the pathogenesis of this condition: presence of amniotic bands, vascular abnormalities that would cause areas of ischemia with necrosis and subsequent scarring, remnants of the thyroglossal duct, compression of the cervical region by the pericardium in early stages of embryonic development and incomplete fusion of the distal branchial arches in the midline.6
Cervical midline clefts are lesions that can cause functional disorders with limitation of cervical extension and psychological disorders due to their aesthetic implications. Their treatment is surgical.7,8 It is recommended to perform resection of the lesion, including the fibrous tissue, reaching the deep pretracheal plane to avoid recurrences. To close the defect, the advancement of lateral skin flaps and lengthening of the shortened area is suggested. A straight closure is not always advisable because it can cause retraction and subsequent shortening, although in this case it was performed without difficulty and without leaving sequelae.9
CMCC may be associated with other anomalies such as thyroglossal duct cyst,10,11 ectopic bronchogenic cyst, cleft lower lip, tongue and jaw, cleft sternum, and cardiac ectopia with intracardiac anomalies.12
To date, we have not found any reports of this condition in our setting. As in most patients, the clinical findings allowed for early diagnosis, in addition to differentiation from other congenital conditions such as fistulas and branchial sinuses. Clinical experience has shown that over time it can scar and form a rigid structure that leads to a neck contracture with limited mobility, functional compromise and sometimes torticollis. It has been observed that early treatment guarantees better results and a lower risk of recurrence and complications. There is little controversy regarding the treatment of choice for this condition; different authors agree on complete surgical excision and the performance of zetaplasties to prevent anterior neck contraction and achieve acceptable cosmetic results.7
Diagnosis is made by clinical examination of the lesion at birth and treatment is surgical excision. Although there is no agreement on the appropriate age for treatment of CMCC, we recommend early intervention due to the disfiguring appearance of the lesion. Furthermore, if not treated in time, the lesion behaves like a scar and, by becoming a cervical cord in the midline, acts as a tether. This in turn will cause limitation in neck extension as the child grows. Furthermore, Ercocen et al suggested that early intervention prevents the disfiguring appearance of the malformation and also prevents later limitation of neck movement.8
The treatment of midline cleft is based on surgical resection of the lesion, in order to avoid complications such as cervical contracture and secondary aesthetic deformities. Most authors suggest the correction of this entity especially in the first two years of life to prevent such complications. The surgical technique is based on complete resection of the skin defect and subcutaneous fibrous cord with a subsequent closure based on a Z-plasty technique to improve healing and camouflage of the surgical site.13,14
Finally, our purpose was to evaluate the clinical characteristics, histopathological features and treatment modalities that we could offer to our newborns, this being the first reported case.
Congenital cervical anomalies are a heterogeneous group of diseases that can occur from birth to adulthood. In order to achieve optimal management of this type of lesions and thus avoid possible complications derived from them, it is of utmost importance that both pediatricians and pediatric surgeons know the embryological origin, as well as the main clinical manifestations of each of the different pathological entities that can occur in the cervical region. In order to make a correct differential diagnosis of this set of malformations, complementary imaging studies are usually necessary. These will help us to classify the lesion and to know the most important anatomical relationships of the same in order to design an adequate therapeutic strategy that, in most cases, will include its surgical removal.
Congenital midline cervical cleft is one of the rarest congenital anomalies of the neck and, although it has well-defined features, is often not recognized at birth. CMCC should be considered when evaluating a child with a cervical midline lesion and differentiated from other more common neck anomalies. Early recognition at birth and a structured diagnostic evaluation are necessary to ensure a favorable outcome. CMCC requires clinical and surgical follow-up that should be planned after birth.
Mid-cervical cleft represents a rare congenital defect with 205 cases reported in the literature. It has rarely been associated with other anomalies. Surgical excision is simple, reconstruction with multiple Z-plasties produces good aesthetic results, while improving neck mobility and avoiding long-term mandibular defects.13 It is a rare pathology, but it should be known due to the possible complications it may cause.15
It is important for pediatricians, neonatologists, and pediatric surgeons to recognize this rare congenital anomaly. Although the exact timing of surgery for CMCC is not clearly stated, intervention as early as possible is recommended as the outcome of the operation will be excellent.
The patient was assessed by pediatric surgery and an initial wait-and-see approach was decided. Curative surgical treatment will be scheduled around one year of age.
Thus, congenital midline cleft, despite being a rare congenital malformation, is an entity that requires a high degree of clinical suspicion when evaluating patients with midline neck defects, given that the clinical findings in almost all cases are sufficient to make an adequate diagnosis, without having to resort to expensive diagnostic aids and thus allow intervention at an early age that prevents the appearance of sequelae or major aesthetic defects that complicate its subsequent correction.16
Surgical management is the cornerstone of treatment based on resection and correction by Z-plasty. Performing it at an early age minimizes the possibility of functional and aesthetic sequelae.
Neck injuries are very common in Pediatrics. Knowledge of all of them is important to establish an adequate diagnosis. Among these conditions, the middle cervical cleft is one of the least frequent. In this condition, a timely diagnosis and treatment improves the post-operative evolution and prevents deforming sequelae.
These patients require long-term follow-up to verify the effect of growth on the remaining scar, and the eventual need for any other procedure.
The medical history was kept strictly confidential; the use of the data was only for academic purposes.
None.
None.
The authors declare that they have no financial interests or personal relationships that could have influenced this work.

©2025 Hernando, et al. This is an open access article distributed under the terms of the, which permits unrestricted use, distribution, and build upon your work non-commercially.