Journal of
eISSN: 2373-4426


Research Article Volume 14 Issue 2
Mother and Children Department, University of Parakou, Regional Teaching Hospital of Borgou-Alibori, Benin
Correspondence: Noudamadjo Alphonse, Mother and Children Department, University of Parakou, Regional Teaching Hospital of Borgou-Alibori, 03 PO Box 369 Parakou, Borgou, Benin, Tel (+229) 90 049007/ (+229) 94794149
Received: April 11, 2024 | Published: May 7, 2024
Citation: Noudamadjo A, Agbeille MF, Voduhè MV, et al. Frequency and immediate neonatal prognosis of low birth weight neonates in Parakou (Benin) in 2018. J Pediatr Neonatal Care. 2024;14(2):109-112. DOI: 10.15406/jpnc.2024.14.00550
Introduction: Infant and child mortality remains high in Benin and is sustained by neonatal mortality which has stagnated for decades. Low birth weight (LBW) is recognized to be an important risk factor for neonatal death worldwide and serves as an indicator of perinatal death.
Objective: The objective is to establish the relationship between LBW and immediate neonatal prognosis in the city of Parakou (Benin).
Patients and methods: This was a cross-sectional study with a descriptive and analytical aim. A prospective collection of data on neonates born from pregnancies with a gestational age of at least 22 weeks of amenorrhea was carried out. It was conducted in three health structures drawn randomly from ten structures in the city of Parakou from May 15 to July 14, 2018. The study included all live neonates. The recruitment of neonates was subject to an oral informed consent of their mothers. We excluded from this study any malformed neonate, any neonate who died in utero and any neonate born from a multiple pregnancy. The data collected were processed and analyzed using Epi Data 3.1, Microsoft Excel 2007 and Epi Info version 7.1.5.0 software. Statistical inferences (Chi-Square test, Person test, Yates correction, Ficher's exact test and their confidence intervals) were used to check the level of association between LBW and morbid situations and then immediate mortality. The research protocol was submitted to the local ethics committee of the University of Parakou and obtained its approval under the reference 0121/CLERB-UP/P/SP/R/SA of May 5, 2018.
Results: The frequency of LBW was 16.9%. LBW was associated with poor adaptation to extrauterine life (p=0.000), neonatal resuscitation (p=0.000) and early neonatal mortality (p=0.000). Birth weight in neonates with LBW was inversely related to the risk of death within 24 hours of life.
Conclusion: One in six neonates had LBW in the city of Parakou in 2018. LBW at birth was a state at risk of neonatal resuscitation and early death. Reducing neonatal mortality requires preventing low birth weight.
Keywords: low birth weight, immediate neonatal prognosis, Benin
Low Birth Weight (LBW) is defined as any live birth of a child weighing less than 2500 grams (g) regardless of its gestational age (GA).1 It is a major public health problem in both developing and developed countries.2 Furthermore, LBW has long been used as an indicator of perinatal health because of its link with the survival, health status and subsequent development of the neonate.2
The global prevalence of LBW is 16%, greater in third world countries (up to 17.3%) than in developed countries (7.2%).2 In Benin, on average 13% of women give birth to a LBW neonate and this prevalence reaches 17.4% in the department of Borgou.3
According to WHO, LBW is not only a predictive condition of perinatal death but recent studies have shown that it also increases the risk of non-communicable diseases in adulthood.4 Furthermore, these LBW neonates are 20 times more likely to die than normal weight neonates.2 In the world and in Benin, the leading cause of hospitalization and death in neonatal units is represented by LBW neonates.2,4,5 It is in this context that the present work was initiated. The objective was to establish the relationship between LBW and immediate neonatal prognosis in the city of Parakou.
This was a cross-sectional study with descriptive and analytical aims. A prospective data collection was carried out in three public health centers in the city of Parakou (the Regional Teaching Hospital of Borgou-Alibori (CHUD-B/A), Kpebie Health Center and Zongo Health Center), drawn at random from the ten functional centers. It covered a period of 2 months from May 15 to July 14, 2018. The study included all live neonates with a gestational age of 22 weeks and above. The recruitment of neonates was subject to an oral informed consent of their mothers. We excluded from this study any malformed neonate, any neonate who died in utero and any neonate born from a multiple pregnancy. The minimum sample size was 317 and was calculated using Schwartz Formula, N= (1.96²pq) / i² with a prevalence p of 17.4%.3 The risk of error agreed (i) was 4% and q=1-p.
The variables studied were: gestational age (divided into 4 classes: [22-28[WA; [28-32[WA; [32-37[WA; and ≥37 WA), birth weight (divided into 3 classes: <1000 grams, 1000-1499 grams and 1500-2499 grams), the Apgar score at the end of the fifth minute (divided into 2 classes: <7 and ≥7), resuscitation at birth (yes and no), vital status at 24 hours of life (grouped into living neonates and deceased neonates). The data were collected from the medical records of neonates in the neonatology department of CHUD/BA and in the maternity wards covered by the study. All at risk neonates identified in the maternity wards were referred to the unit of neonatology.
A double data entry was made in the French version of Epi Data 3.1 software. The analysis was carried out in Epi Info software version 7.1.5.0.
Statistical inferences (Chi-Square test, Person test, Yates correction and Ficher exact test) were used as necessary to assess the distribution of the problem in the population studied. The difference was considered statistically significant for p <0.05. The mean and median were used for the distribution of quantitative variables. The Odds Ratio (OR) was used as a measure of association. The research protocol was submitted to the local ethics committee of the University of Parakou and obtained its approval under the reference 0121/CLERB-UP/P/SP/R/SA of May 5, 2018.
At the end of the study period, 524 neonates were identified and 8 were not included due to parental refusal. 60 were excluded including twins (39), malformation (12) and stillbirth (09). The number of neonates retained was 456.
The frequency of LBW during the study period in the three maternity wards varied from 12.3% to 20.1% without a significant difference. The overall frequency was 16.9% (77 out of 456) 95% CI = [13.63-20.72] (Table 1).
|
|
Total (N) |
LBW |
p-value |
|
|
n (<2500 g) |
% |
|||
|
CHUD /BA |
239 |
48 |
20.1 |
0.139 |
|
Zongo Health Center |
79 |
12 |
15.2 |
|
|
Kpebie Health Center |
138 |
17 |
12.3 |
|
|
Total |
456 |
77 |
16.9 |
|
Table 1 Frequency of LBW in public health centers in the city of Parakou, 2018
The average gestational age of LBW neonates was 36.7 ± 3.4 weeks of amenorrhea (WA) with the extremes of 24 WA and 40 WA. More than half of LBW neonates were at term (50.6%). The distribution of neonates included according to gestational age is presented in Figure 1.
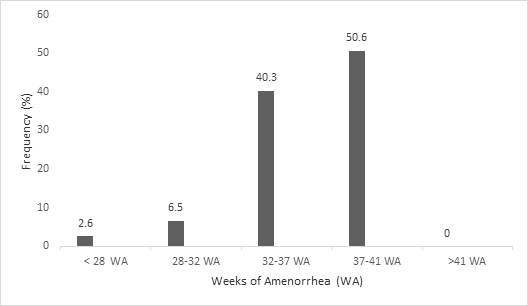
Figure 1 Distribution of low birth weight neonates according to gestational age in public health centers in the city of Parakou, 2018.
The average weight of LBW neonates was 2063.6 ± 364.4g with the extremes of 700g and 2450g. The study showed 2.6% of extremely low birth weight and 6.5% of very low birth weight (Figure 2).
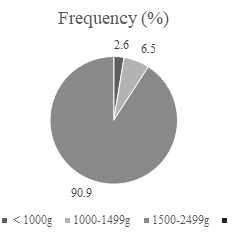
Figure 2 Distribution of low birth weight neonates according to weight group in public health centers in the city of Parakou, 2018.
Tables 2 and 3 present the relationship between LBW and immediate neonatal morbidity on the one hand, then LBW and immediate neonatal mortality on the other hand. The Apgar score at the fifth minute was less than 7 in 73.7% of LBW with a statistically significant difference (p=0.000) and an OR of 5.11 [3.59-7.27], meaning that LBW presented a 5.11 times risk of being born with a poor adaptation to extrauterine life than the others. Concerning the notion of resuscitation at birth, it included 58.0% of LBW. There was a significant difference (p=0.000). The risk of being resuscitated at birth was 4.91 times in LBW neonates compared to normal weight neonates (OR=4.91 [3.44-6.99]). Regarding immediate neonatal death (within 24 hours of life), it concerned 12.0% of LBWs with a significant difference p=0.000). The LBW neonates had a risk of 9.84 of dying in the immediate neonatal period than normal weight neonates (OR = 9.84 [3.46-27.99]).
|
|
Total (N) |
Birth weight |
Crude OR [95% CI] |
p-value |
|
|
n (<2500 g) |
% |
||||
|
APGAR score (5th minute) |
|||||
|
<7 |
19 |
14 |
73.9 |
5.1 [3.59-7.27] |
0 |
|
≥7 |
437 |
63 |
14.4 |
1 |
- |
|
Resuscitation |
|||||
|
Yes |
50 |
29 |
58 |
4.9 [3.44-6.99] |
0 |
|
No |
406 |
48 |
11.8 |
1 |
- |
Table 2 Immediate neonatal prognosis of low birth weight neonates in public health centers in the city of Parakou, 2018
|
|
Neonatal outcome |
Total |
OR [95%CI] |
p-value |
|||
|
Deceased (n=10) |
Alive (n=67) |
||||||
|
n |
% |
N |
% |
||||
|
LBW |
10 |
13 |
67 |
87 |
77 |
9.8 |
0 |
|
Normal weight |
5 |
1.3 |
374 |
98.9 |
379 |
1 |
|
Table 3 Relationship between vital status at 24 hours of life and low birth weight in public health centers in the city of Parakou, 2018
Table 4 illustrates the influence of birth weight and gestational age of LBW neonates on immediate neonatal mortality. Neonates with extremely low birth weight (< 1000 grams) had a significantly higher death rate (100%) than others (p<0.001). The lower the birth weight, the higher the mortality. The mortality rate decreased as the birth weight approached 2500 grams. The same is true for gestational age without a significant difference.
|
|
Neonatal outcome |
Total (n=77) |
OR [95% CI] |
p-value |
|||
|
Deceased (n=10) |
Alive (n=67) |
||||||
|
n |
% |
N |
% |
||||
|
Gestational age |
|||||||
|
<28 WA |
1 |
50 |
1 |
50 |
2 |
6.5 [1.12-37.84] |
0.187 |
|
28-32 WA |
1 |
20 |
4 |
80 |
5 |
2.6 [0.33-20.46] |
0.394 |
|
32-37 WA |
5 |
16.1 |
26 |
83.9 |
31 |
2.1 [0.54-8.09] |
0.452 |
|
≥37 WA |
3 |
6.7 |
36 |
92.3 |
39 |
1 |
|
|
Birth weight |
|||||||
|
<1000 grams |
2 |
100 |
0 |
0 |
2 |
11.7 [5.43-25.07] |
0.0035 |
|
1000-1499 grams |
2 |
40 |
3 |
60 |
5 |
4.7 [1.25-17.44] |
0.0278 |
|
1500-2499 grams |
6 |
8.6 |
64 |
91.4 |
70 |
1 |
|
Table 4 Risk factors for mortality among low birth weight neonates in public health centers in the city of Parakou, 2018
During this study, measures were taken to minimize selection and information bias by carrying out a random selection of three health centers among the ten centers in the city of Parakou and ensuring that the data are collected in the same way. However, the univariate analysis carried out to establish the relationship between LBW and immediate neonatal prognosis is not sufficient to reduce the risk of confounding bias. Furthermore, the low number of deaths and more generally of the subjects included in the study is likely to reduce the power of the relationship established between LBW and immediate neonatal mortality, hence the need to consider a study focusing on larger sample sizes and using multivariate analysis to test potential associations.
This study reported an average frequency of 16.9% of LBW neonates in the three public maternity hospitals in Parakou. The frequency of LBW neonates in this study is close to that reported by the Demographic and Health Survey (DHS) IV in the department of Borgou (17.3%) but higher than the national prevalence of LBW in our country (13%).3 The extent of this situation in our country and especially in the department of Borgou could be explained on the one hand by a lack of knowledge of the risk factors of LBW and on the other hand, by the socio-cultural constraints which could constitute an obstacle to the adherence of mothers to information on maternal and neonatal health. It is important to carry out a community study on the risk factors of LBW.
In Sub-Saharan Africa, some authors have reported higher proportions. Chiabi et al in Cameroon had observed a frequency of 20.79% at the maternity hospital of Yaounde6 and Bayo et al in Uganda reported a hospital frequency of 25.5%.7 In Asia, Misra et al in India8 and Baghianimoghadam et al in Iran9 reported a frequency of 26.28% in Jalandha hospital and 20.1% in Urmia city, respectively.
Compared to developed countries, the frequency observed in the study was double that of developed countries.10 This supports the hypothesis of the real public health problem that LBW constitutes in developing countries.
In the present work, hypotrophy was predominant in LBW neonates. Padonou et al11 in Benin in 2014 made the same observation. The predominance of hypotrophy compared to prematurity is classically observed in developing countries where more than three quarters of low birth weight neonates suffer from hypotrophy. This could be explained by the high frequency of malnutrition in both macronutrients and micronutrients among pregnant women. Our results differ from those of Siza et al,12 carried out in a referral hospital in northern Tanzania which showed a predominance of prematurity of around 90.87% among LBW neonates.
Neonates whose birth weight was between 1500g and 2499g were the most represented (91.0%). Beddek et al13 in Algeria and Letaief et al14 in Tunisia made the same observation.
In this study, low birth weight neonates resuscitated at birth were 4.91 times more likely to die than those not resuscitated. This observation was made by Ouédraogo-Yugbaré et al15 in Burkina Faso.
Regarding the Apgar score, the study showed that a poor Apgar score (<7) was a poor prognostic factor for neonatal mortality in LBW neonates. Indeed, LBW neonates with an APGAR score less than 7 at the fifth minute had 5.11 times the risk of dying than others with a statistically significant difference (p <0.001). Our results corroborate those of Chiabi et al6 in Cameroon and Ouédraogo-Yugbaré et al15 in Burkina Faso.
This high mortality in the event of a poor Apgar score or resuscitation at birth could be explained by the immaturity of most of the functions and systems of LBW premature babies and the increased risk of hypoxia in utero in those at term. As the transfer of these neonates from a first level maternity ward to a neonatology unit was not medicalized, they are exposed to hypothermia and an increased risk of mortality.
In this study, mortality was 100%, 40.0% and 8.6% in neonates weighing less than or equal to 1000 g, between 1000 and 1500 g, then between 1500 and 2500 g ( p <0.001), respectively. The mortality rate was inversely proportional to birth weight with a statistically significant difference. Birth weight therefore constitutes a determining factor in the immediate neonatal prognosis of LBW. According to our results, gestational age was not identified as a prognostic factor for mortality of LBW neonates within 24 hours of life. Ilunga et al16 in Congo, on the other hand, noted that neonatal mortality decreased significantly in inverse relation to gestational age, that is to say, the greater the gestational age, the lower the neonatal mortality.
At the end of the study, one in six neonates had a low birth weight. LBW was statistically significantly associated with the risk of poor adaptation to extrauterine life and death within 24 hours of life. Furthermore, independently of gestational age, birth weight was inversely proportional to the risk of death of LBW neonates within 24 hours of life. Reducing immediate neonatal mortality requires controlling LBW risk factors, which must be the subject of subsequent studies involving larger numbers.
None.
None.
The authors declare that there are no conflicts of interest.

©2024 Noudamadjo, et al. This is an open access article distributed under the terms of the, which permits unrestricted use, distribution, and build upon your work non-commercially.