Journal of
eISSN: 2373-4426


Research Article Volume 10 Issue 1
1Bahir Dar University, College of Medicine and Health science, Ethiopia
2Wollo University, College of Medicine and Health science, Ethiopia
Correspondence: Yibeltal Asmamaw Yitayew, Wollo University, College of Medicine and Health science, Ethiopia
Received: January 23, 2020 | Published: February 27, 2020
Citation: Gessesse FG, Yitayew YA. Epidemiology of burn injury among children’s attended felege hiwot referral hospital in bahir dar town, amhara regional state, Ethiopia, 2017. J Pediatr Neonatal Care. 2020;10(1):21-27. DOI: 10.15406/jpnc.2020.10.00408
Background: Burn injury is a major global public health problem accompanied by a high risk of mortality and morbidity. Sufficient knowledge in the epidemiological pattern is necessary to prevent burn injury, but in many developing countries, including Ethiopia, the epidemiological patterns of burn injuries given low attention.
Methods: The institutional-based retrospective cross-sectional study design was conducted from March-April 2017. A total of 102 burn patients were selected in a simple random sampling method. Data were collected retrospectively from patients’ medical records using a data extraction tool among children’s attended Felege Hiwot referral hospital with burn injury from 2011 to 2016. Data were cleaned, coded, and entered in Epi-data version 3.1, then exported to Statistical Package for Social Sciences version 21 for analysis.
Result: The overall prevalence of burn injury among children was 0.46%. In all age groups, the prevalence of burn injury was higher among females. Scald burn injuries account for 42.2%, and 41.61% of burn injuries involved multiple body parts. The majority of children (75.5%) presented with second-degree burns, and the mean TBSA (total body surface area) burned was 12.56 ±8.91. The majority of patients (77.5%) seek health care within <24 hours, 35.3% of patients received prehospital care after burn injury, and 33.3% of patients recovered with significant scarring and disfigurement.
Conclusion and recommendations: The majority of the burn injuries occurred at home, and pre-hospital interventions were mostly harmful practices. Therefore adequate health education should be delivered to the society regarding appropriate pre-hospital interventions and a safe home environment.
Keyword: burn injuries, epidemiology, children, bahirdar, Ethiopia
LMIC, low and middle income countries; LOS, length of stay; TBSA, total body surface area; WHO, world health organization
A burn is a skin and tissue damage caused by agents like fire, scald, electricity, sunlight, and chemical or nuclear radiation.1 Scald burn is the most common type, and home constituted the commonest place of occurrence of burn injury.2,3 Burn can be assessed using the estimate of the depth, and total body surface area burned(TBSA).4 Additionally, burns are classified as superficial, partial, and full-thickness, depending on the depth of injury to the skin.5 Furthermore, it can vary from mild to severe, depending on the total body surface area burned (TBSA), depth, and location of the burn.6 Burn injury is a major global public health problem accompanied by a high risk of mortality and morbidity.7,8 Globally, nearly 96,000 children under the age of 20 were fatally injured as a result of a fire-related burn. Of this, the majority of burn injuries occur in low- and middle-income countries (LMIC).8 The World Health Organization (WHO) estimates that the annual death due to burns is over 310,000, and LMIC accounts for 95% of all annual burn deaths.9 These injuries were rated as the second most common cause of accidental death among African children younger than 5 years of age. In sub-Saharan Africa, it is estimated that between 18,000 and 30,000 children under the age of 18 died annually as a result of burn-related injuries.10
Burns in children differ in multiple aspects from adults and may result in a more sever devastating injuries.6 These injuries include, acute life-threatening complications (Fluid loss, airway obstruction, renal failure, Super-infection) and chronic complications (significant disfigurement, disability and Psychological trauma).7,11 Additionally, Burns account for the greatest length of stay (LOS) of all pediatric hospital admission injuries and the management of pediatric burns remains complicated, challenging and extremely costly even in well-equipped and modern burn units.12,13
The epidemiological patterns of burns vary significantly based on age, sex, economic status, local customs, social, and environmental circumstances.14–22 The epidemiology of burn injuries in developing countries is different from that in the developed world.23 Unfortunately, many developing countries with a significant incidence of burns do not have adequate data for epidemiological analysis.17 Sufficient knowledge about burn injury and its pattern is necessary for the prevention. Research in the epidemiology of burn injury in many developed and high-income countries made a great contribution for the primary and secondary prevention of fires and burns. However, in many developing countries, including Ethiopia, the primary focus is on communicable diseases and the epidemiological patterns of burn injuries given low attention.24 So, this study aimed to assess the epidemiology of burn injury among children’s attended Felege Hiwot referral hospital from 2011 to 2016.
Study design, area and period
The institution-based retrospective cross-sectional study design was conducted in the Felege Hiwot referral hospital from March 25 to April 25, 2017. Felege Hiwot referral hospital is found at Bahir Dar, the capital city of Amhara regional state, which is 565 km away from Addis Ababa, Ethiopia. In 2016, the total population of the town was 750,991. Bahir Dar town is one of the twelve cities that was conferred the UNESCO learning cities award in 2015.25 The town has two governmental hospitals, one private hospital, and three higher clinics. Felge Hiwot referral hospital has a total of 400 beds, and in this hospital, there was no pediatric burn unit.
Sources population
All patients less than 18 years of age sustained burn injury and visited Felege Hiwot hospital for medical care from October 2011- September 2016.
Study population
Randomly selected patients less than 18 years of age sustained burn injury and attended Felege Hiwot hospital for medical care from October 2011- September 2016.
Exclusion Criteria
Incomplete card or cards with illegible hand writing.
Sample size determination and procedure
The sample size was determined using a single population proportion formula, with the assumption of 6.4% (p = 0.064) prevalence of burn injury among children which is taken from the study conducted in Yekatit 12 hospital, Addis Ababa with a 95% confidence level and 5% margin of error.
ni = (Z ɑ /2)2 × p (1– p)/W2
ni = (1.96)2× (0.064) × (0.936)/ (0.05)2 = 92
Where:
ni = initial sample size
ɑ = confidence interval
p = prevalence of burn injury among children
W = margin of error
By considering a 15% data incompleteness rate, the final sample size was calculated to be 108. A total of 325 children attended Felege Hiwot referral hospital from October 2011- September 2016 with burn injury, and a systematic random sampling technique (k=3) was used to select the study participants.
Data were collected from the patient’s medical record using a pre-tested data extraction check-list, which was adopted and modified from previous research conducted in Addis Ababa.26 The medical diagnosis and MRN number of children who had burn injury in the last five years (October 2011 to September 2016) were obtained from the pediatric patient registry log book. The selected children’s chart was accessed using a unique MRN number, and clinical data were obtained from medical files of patients.
Before data collection, a pre-test was conducted in 5% of the final sample size in the Felege Hiwot referral hospital, and adjustments were made based on the finding. One day training and clear orientation were provided to data collectors and supervisors on the process of data collection. During the data collection time, close supervision and monitoring were made by the supervisor to ensure the quality of the data. Finally, the collected data were checked, cleaned, and compiled daily by the principal investigator.
The data were checked for completeness, consistency, and accuracy, then entered into EPI info version 3.1 and exported to SPSS version 21 for data analysis. Frequency, proportion, means, and SD was used to describe the variables and frequency tables chart and graphs were used to present the findings.
Age group: Toddler = [1-3] years
Preschool = [4-6] years
School age= [7-13] years
Pubertal= [14-18) years
Children<18 years
Conservative management: burn patient’s treatment options which include, fluid administration, wound care, administration of antibiotics, analgesics, and tetanus toxoid only or in combination.
Outcome of burn injury: The consequences of burn injury at the end of the treatment mentioned in the patient's card (complete recovery, and recovery with scar or disfigurement, etc.).
Appropriate pre-hospital intervention: Applying cold water or gentian violet in the injured part before getting medical care.
In appropriate pre-hospital intervention: Applying traditional medicine (herbs), oil, egg, and ice in the injured part before getting medical care.
Prevalence of burn injury among children’s
In the five years retrospective study (October 2011 - September 2016), a total of 70,652 patients aged less than 18 years had visited Felege Hiwot referral hospital both in the inpatient (11,775) and outpatient (58,877) departments. Of which 325 (0.46%) patients had sustained a burn injury. Among patients sustained a burn injury, 80(24.6%) were managed on an outpatient basis, and the remaining were admitted in the pediatric ward. Among selected 102 patients, 80(78.4%) were managed on an inpatient basis, and the rest were managed on the outpatient department.
Socio-demographic characteristics of participants
A total of 102 children with burn injuries were included in the study, with a 94.4% data completeness rate. The mean age was 9.56±5.49 years, and 34(33.3%) children were aged from 7-13 years. The majority of them were females (64, 62.7%), and fifty-two (51%) of the total study subjects were from the urban area (Table 1).
Variables |
Category |
Frequency |
Percent (%) |
Age |
1-3 years |
23 |
(22.5%) |
4-6 years |
12 |
(11.8%) |
|
7-13 years |
34 |
(33.3%) |
|
14-18 years |
33 |
(32.4%) |
|
Sex |
Male |
38 |
37.3% |
Female |
64 |
62.7% |
|
Address |
Urban |
52 |
51% |
Rural |
50 |
49% |
Table 1 Socio-demographic characteristics of participants at Felege Hiwot referral hospital, Bahir Dar town, Ethiopia, 2017(n=102).
Clinical characteristics of children’s with burn
Scald burns account for 42.2% of all causes, and 42.2% of burns involve multiple body parts. The majority (75.5%) of burn injuries were second-degree burns, and 56.9% burns were <10% in extent. Similarly, 84.3% of children’s with burn had no pre-existing medical condition, and 75.5% of them had no clinical presentation at the time of admission (Table 2).
Variables |
Category |
Frequency |
Percent (%) |
Cause of burn |
Scald |
43 |
42.2% |
Flame |
41 |
40.2% |
|
Electric |
13 |
12.7% |
|
Chemical |
5 |
4.9% |
|
Anatomic location of burn injury |
upper extremity |
22 |
21.6% |
lower extremity |
26 |
25.5% |
|
anterior trunk |
5 |
4.9% |
|
posterior trunk |
2 |
2% |
|
face and neck |
4 |
3.9% |
|
multiple body part |
43 |
42.2% |
|
Depth of burn |
First degree |
16 |
15.7% |
Second degree |
77 |
75.5% |
|
Third degree |
9 |
8.8% |
|
Extent of burn |
<10% |
58 |
56.9% |
10-20% |
32 |
31.4% |
|
>20% |
12 |
11.8% |
|
Pre-existing medical condition |
Yes |
16 |
15.7% |
No |
86 |
84.3% |
|
Clinical presentation at the time of admission |
Yes |
25 |
24.5% |
No |
77 |
75.5% |
Table 2 Clinical characteristics of burn injury among children’s at Felege Hiwot referral hospital, Bahirdar town, Ethiopia, 2017(102).
Among 16(15.7%) children having pre-existing medical conditions, 8(50%) had epilepsy, 5(31.25%) had HIV/AIDS, 2(12.5%) had malnutrition and 1(6.25%) had anemia. Concerning clinical presentation at the time of evaluation, 10(9.8%) patients presented with loss of consciousness, 4(3.9%) patients presented with airway compromise, 2(1.9%) patients with shock and 9(8.8%) patients presented with either of post-burn contracture, diarrhea and vomiting, and skin discoloration.
Scald burns predominated in toddlers (1-3years) (87%), and the flame was the predominant cause of burn among pubertal age (14-18 years)(66.7%). Of all scald burn injuries, 30.2% of them were due to hot milk, and the remaining were due to hot tea 23.2%, hot soup/food 18.6%, hot water 18.6%, and hot oil 9.3%. Moreover, among the total 102 burns injuries, 99.1% were accidental, while the remaining was intentional (Figures 1-3).
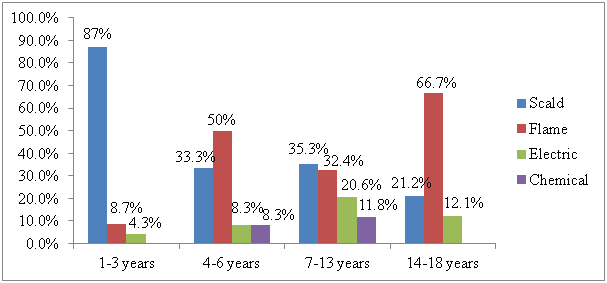
Figure 1 Age distribution of type of burn injuries among children’s at Felege Hiwot referral hospital, Bahirdar town, Ethiopia, 2017(102).
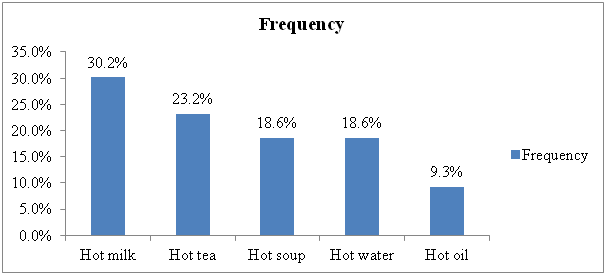
Figure 2 Causes of scald burn injuries among children’s at Felege Hiwot referral hospital, Bahirdar town, Ethiopia, 2017(102).
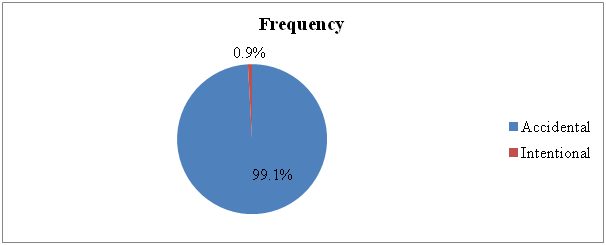
Figure 3 Mechanism of occurrence of burn injury among children’s at Felege Hiwot referral hospital, Bahirdar town, Ethiopia, 2017(102).
Time related characteristics of burn injury
Duration of time before getting medical attention and length of hospital stay
Most of the patients (77.5%) seek health care within <24 hours, and the mean length of hospital stay was 14.14 days±14.82 (median: 7; range: 1-66 days) (Figure 4). Eighty-nine (87.3%) cases discharged within 30 days of hospital stay, and the remaining (12.7%) cases discharged after 30 days.
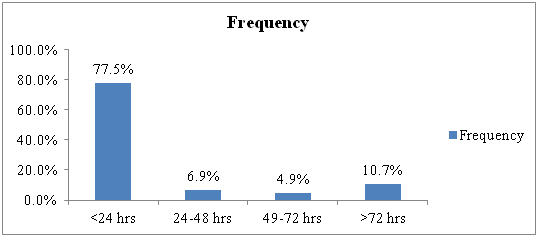
Figure 4 Duration of time before getting medical attention after burn injury among children’s at Felege Hiwot referral hospital, Bahirdar town, Ethiopia, 2017(102).
Management related characteristics
Pre hospital intervention and hospital Management
Among 102 patients, first aid was provided only for 35.3% of patients immediately after the occurrence of burn injury. The most common (63.8%) first aid measures given for these burn patients represent harmful practices, and the rest 36.2% received pre-hospital intervention considered to be appropriate like cold water irrigation (Figure 5). Conservative treatment was successful in 89.7% of cases which includes, 78.4% wound cleaning and dressing, 60.8% antibiotics, 41.1% tetanus toxoid, 32.3% fluid replacement,13.7% analgesics, and 2.9% physiotherapies. A total of 15 surgical interventions were carried out for 11 children, including 7 patients contracture release, 5 patients underwent debridement, and 3 patients underwent grafting procedures.
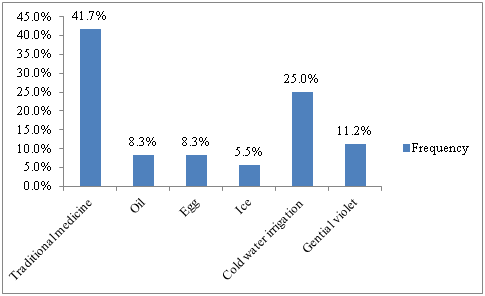
Figure 5 Pre-hospital intervention after burn injury among children’s at Felege Hiwot referral hospital, Bahirdar town, Ethiopia, 2017(102).
Clinical outcome of burn injury
Most of the burn patients (58.8%) healed without complication, 33.3% of patients recovered with significant scarring and disfigurement at the end of treatment and 7.8% patients were discharged with a summary of discharge saying ‘Discharged against medical advice’ hence, their outcome was unknown in the study period. The majority of children’s with TBSA burned >20% healed with scar and disfigurement (Figure 6).
In this study, the prevalence of pediatric burn injuries was found to be 0.46%, which is lower than the findings of the study conducted at Yekatit 12 hospital (6.4%).26 The higher prevalence in Yekatit 12 hospital could be explained by the fact that the study was conducted in a burn center where burn cases are expectedly high. The majority of burn patients were females (62.7%). A similar finding from America (54%) and Tanzania (50.4%) reported that female burn cases were higher than male burn cases.27,28 The main reason why female burn cases were higher may be possibly due to increased exposure of females to household activities such as cooking and baking. Moreover, the majority of pediatric burn injuries in this study occurred at home (96.1%), and this finding was comparable with other studies in Pakistan29 and Peru30 in which 91.5% and 77.5% burn cases occurred at home respectively. This could be probably due to children’s tendency to spend most of their time with their mothers at home or in the kitchen.
The most frequent cause of burn injuries in this study was scald. This finding is in agreement with the finding in Kenya,9 Brazil,20 and Tanzania27 in which scald burn was reported high compared to other causes of burn injury. This might be due to children’s attitude in playing (stay) at home or in the kitchen with their mother or guardians where drinks and liquid foods are being prepared. The findings of this study showed Scald burns occurred more in toddlers compared to their elders. This finding is consistent with the study in Peru, which reported that toddlers were more affected by scald burn.30 This could be because, in this age group, children start to investigate their environment and learn walking by grabbing different equipment and vulnerable to injury when they are left unattended near hot fluids. The majority of the study participants (77.5%) in this study presented to the emergency department within 24 hours of injury. This finding is greater than the study conducted in Nigeria, where only 56.7%of burn injuries were presented to the emergency department within 24 hours of injury.31 This could be explained by the probable difference in public awareness regarding health-seeking behavior. The mean TBSA burnt in this study (12.56%±8.91) was lower than reported in Istanbul, Turkey (16.6% ±12.57), and Lagos, Nigeria (29.67 ±21.98) (16, 32). However, this finding was higher than the mean TBSA shown from Kenya (6.5% ±8.1) and Pakistan (9.37 ±9.61).9,29 This discrepancy may be due to the differences in causes of burn injury and the respective duration of contact with the burning agent. In this study, the mean length of hospital stay was 14.14 ±14.83days. The finding was lower than a study conducted in Lagos State University Teaching Hospital which was 18.61±24.18 days.32 On the other hand, a study from Iran showed a much lower mean hospital stay than this study which was 7.5±3.2 days.15 The discrepancy could be attributed to the differences in the extent of wounds as well as patient health conditions. Extensive wounds, for instance, require more time to heal (needs cleaning and dressing for a number of days).
Extremities were the most frequently affected anatomical sites (47.1%) of burn patients in this study. In agreement with this finding, a study conducted in Addis Ababa also found that burns involving the extremities were most frequent (51.2%).19 This might be attributed to how a burn injury occurs to a child. Usually, hot substances spill on the children’s extremities while playing.
The pre-hospital intervention was given to 35.3% of the study subjects. A lower finding was reported from Tanzania, in which only 6.7% of pediatric burn victims got pre-hospital interventions.22 On the contrary, a study from Yekatit 12 hospital showed that 77% of burn cases had received the pre-hospital intervention, which is much higher than this finding.26 However, only 36.1% of burn patients in this study and 17.3% burn patients from a study in Yekatit 12 Hospital had received first aid measures, which are considered appropriate such as cold water irrigation and application of gentian violet. This discrepancy may be attributed to the difference in public awareness and knowledge about first aid procedures for burns from one country to another and from place to place within the country. In this study, conservative treatment was successful in 89.7% of burn cases. This finding was higher than a study from Turkey, in which 57.6% of burn cases were managed conservatively.16 This might be due to the difference in TBSA burnt. The mean TBSA burnt in Turkey’s study was higher than this study, and this difference will affect treatment options. This study revealed that 58.8% of patients healed completely, and this finding is lower than a finding from Iran in which 77.9% of burned patients healed without squalle.21 This discrepancy might be due to the difference of pre-existing medical condition, extent, and depth of burn injury, and quality of care.
Since this research was a retrospective study, including other characteristics that could only be assessed by observation or history-taking was not possible.
The prevalence of burn injury among children in the study area was low. The majority of the burn injuries were partial thickness burn and occurred at home. Extremities were the most frequently affected body parts, and pre-hospital interventions following burn injury were mostly harmful practices. Therefore, adequate health education should be delivered to the society regarding appropriate pre-hospital interventions following burn injury. Additionally, health education should be delivered to parents and caretakers regarding the safe home environment.
None.
The authors declare there are no conflicts of interest.
None.

©2020 Gessesse, et al. This is an open access article distributed under the terms of the, which permits unrestricted use, distribution, and build upon your work non-commercially.