Journal of
eISSN: 2373-4426


Research Article Volume 13 Issue 3
Department of Bioengineering, Imperial College London, United Kingdom
Correspondence: Professor Hippolite O. Amadi, Bioengineering department, Imperial College London, South Kensington Campus SW7 2AZ, United Kingdom, Tel +44 7984175083
Received: September 04, 2023 | Published: September 19, 2023
Citation: Amadi HO. Empowering the LMIC hinterlands with compatible technologies for neonatal care – the resilience of a research group. J Pediatr Neonatal Care. 2023;13(3):174-179. DOI: 10.15406/jpnc.2023.13.00512
Background: High neonatal mortality rate (NMR) in low- and middle-income countries (LMIC) might not be resolved until rural healthcare facilities are empowered with sustainable frugal technologies and procedures. Needed technologies may not rely on cutting-edge systems of the high-income countries (HIC), which require much funding and well-established public infrastructure to thrive. Rather, tailored non-conventional designs that are compatible with the deficiencies at low-income settings must take center stage.
Study design: A multistage strategy was designed to identify and resolve the technology and knowledge gaps responsible for high NMR and rural community deficiencies militating against neonatal interventions within the primary healthcare settings in Nigeria.
Methods: We concluded many scientific investigations and developed interventions over 25 years period to resolve the various factors militating against neonatal survival in Nigeria. Unconventional ideas relying on solar powered systems and easily available local materials were developed, trialed, and commissioned at various times across 31 tertiary hospitals spanning all regions of Nigeria. Stand-alone studies or solutions-creation, amidst discouraging situations, were individually completed, peer-reviewed, and journal-published. The full package of technologies was finally assembled to launch a community empowerment strategy – the Neonatal Rescue Scheme – to generate integrated proof of concept.
Finding: The number of early neonatal deaths and overall NMR drastically reduced at participating centers.
Conclusions: This Rescue-Scheme strategy could revolutionize neonatal healthcare in low-income countries and drastically reduce Nigeria’s corporate NMR if properly adopted.
Clinical evidence: Recent studies of the Scheme and various combinations of its neonatal technologies have demonstrated significant clinical evidence of NMR-reduction, e.g., overall NMR fell from 90/’00 to 4/’00 as published by Amina-center Minna Nigeria 2023; early mortality fell from 81% to 0% - University of Abuja Teaching Hospital Nigeria 2017, etc.
Keywords: neonatal rescue scheme, neonatal mortality, frugal technology, solar systems, LMIC
Previous publications of the World Health Organization (WHO) in collaboration with many international GlobalHealth agencies contain vast number of revealing facts about the never-ending high neonatal mortality rate (NMR) in Nigeria.1–3 The various causes of death could be argued to be well researched, however, the country-specific solutions to these were far from being discovered and strategized. Therefore, NMR continued to soar irrespective of numerous funded programs using conventional neonatal care technologies over the last two decades. The Nigerian situation is compounded by factors such as social-cultural, climatic, and infrastructural inadequacies, and knowledge gaps.
Low- and Middle-income Countries (LMICs) in Africa, such as Nigeria, have challenges of unsustainable basic infrastructure. This does not allow for competitive, independent, and progressive healthcare systems. There is high dependence on unsustainable importation of needed technologies, and challenges of adverse climatic impacts on neonatal health seem overwhelming. These have contributed to the prevailing high NMR in Nigeria, for example. Effective neonatal care requires sustainable and affordable technologies, which currently remain elusive to these LMICs. This research article is focusing on, and referencing, our extensive neonatal work experience across all regions of Nigeria, spanning over a quarter century. This reveals that the country is full of intelligent basic skilled nurses and doctors who could help to lower mortality if the necessary technologies were available. The problem was that technology requirements to save the neonates had remained unaffordable and insufficient in most Nigerian centers, creating no immediate hope for mortality reduction. This situation needed to change, but in a successful manner. However, the country’s high poverty rate and 100% dependency on technology-importation has further put any sustainable solution beyond her reach. A possible solution that could alter this negative trend must be radical, affordable, and indigenously driven and self-sustaining. Therefore, the search for this comprehensive solution inspired the long-term efforts being addressed.
This presentation highlights the components of our Neonatal Rescue Scheme (NRS) and its recent frugal devices and ideas that could potentially revolutionize neonatal healthcare in Nigerian and other LMICs. These are radical ideas within the contexts of rural healthcare transformation, empowering dwellers in remote locations of the LMICs with extraordinary knowledge to push their own boundaries of neonatal survival. The rural health centers in the hinterlands of Nigeria are limited in skills and technologies to handle neonatal devastating conditions such as extreme prematurity requiring incubator care, respiratory distress syndrome requiring non-invasive respiratory support machines with the use of oxygen delivery techniques, threats of hyper-bilirubinemia and kernicterus syndrome disorder (KSD) requiring early phototherapy treatment, amongst other conditions. Many neonates in the interior villages die of these conditions because they are unable to successfully make the journeys to the centers in the urbanized cities where there could be expertise but without guarantee for survival. Therefore, many of them die without being known or counted. Our NRS was conceptualized in the attempt to change all these with technologies that empower the rural community.
A long-term research project was necessary. The actualization of this project required high dedication and consistency towards scientific investigation of various stand-alone research questions, covering various social, climate and health issues that adversely impact neonatal survival. A properly harnessed insight from the research investigations could be applied to design and develop appropriately tailored solutions that could mitigate the researched militating factors.
The knowledge of neonatal anatomy, physiology and standard intervention technologies were explored and harnessed. Other mortality impacting factors were studied and applied, including regional climate changes, poor national infrastructure, practitioners’ knowledge gaps, and societal behavioral patterns. Frugal, compatible, and sustainable devices and procedures were strategically developed and improved upon over 20 years, beginning from 1996, supported with concerted training of practicing professionals who trialed and applied our emerging technologies at tertiary hospitals across the entire regions of Nigeria. The GlobalHealth drive of the UN’s Millennium Development Goal Target No.4 (MDG4) was leveraged upon as justification to initiate a corporate collaboration with motivated Chief Medical Directors (CMD) at Nigerian referral hospitals, mediated through the comradeship of the Committee of chief executives of tertiary hospitals (CCETH) of Nigeria in 2007.
Facility participation comprising institutions across the entire regions of Nigeria rapidly grew, albeit in discrete capacities based on the varying choices of the respective CMDs. This was frustrating as the bad choices of many CMDs were not necessarily for neonatal interests, but selfishly ill-motivated. However, participation grew and dwindled at various times based on the level of emphases to remain focused by the changing leaderships at CCETH. Hence, collaborative efforts were maximized during the tenure of every willing incumbent CMD, before the possible emergence of a passionless successor-in-office, who could frustrate the progress of the work, or terminate the collaboration, often due to selfish reasons (Figure 1).
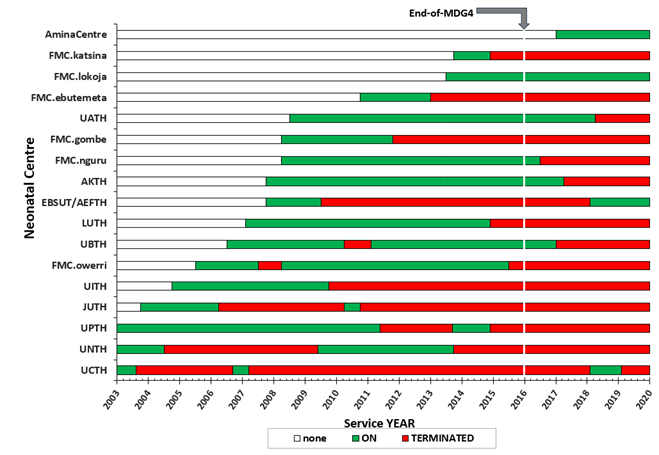
Figure 1 Nigerian tertiary hospitals’ inconsistencies until end-of-MDG4 and beyond.
[Only the top 16 collaborated Teaching Hospitals (TH) and Federal Medical Centers (FMC) has been plotted].
The nationwide outreach across participating tertiary hospitals was maintained despite the dwindling numbers of collaborating institutions at various times until the end of 2015, when MDG4 ended. Basic science studies, syntheses of interventions, technology, and protocol developments, were strategically tailored towards possible practices in the hardest-to-reach places and remote villages of the country. Therefore, efforts were made to develop systems that could rely on low-voltage power that could be harnessed from the sun. Some of these comprised recycled incubators, resuscitaires, phototherapy machines, the politeheartCPAP machine, patient monitors, the politeoxygen-blend system, and the polite-light-bank system, etc. Intuitive simple‑to‑apply thermoneutral control protocols were developed and introduced – such as the hippolite initial setpoint algorithm (HISA) and hippolite handy approach (HHA), and various nursery building correction features to mitigate the climate and to enhance neonatal safety in other ramifications. Training modules and certificate courses were developed and applied to enhance the knowledge of basic nursing and clinical officers, who are typically found in the rural health centers, on simplified neonatal care protocols using the developed devices and procedures. The transferred knowledge and devices empowered and enhanced the confidence of the rural dweller practitioners on the management of the cases for which they, by default, would normally initiate unsuccessful referrals to bigger urban city hospitals. Nurses and doctors in all the participating tertiary hospitals were encouraged to attend the courses, empowering them to utilize the gained knowledge at their respective centers, but at the same time, supporting our team as the knowledge was transferred to rurally located facilities, further into the hinterlands.
Comparative analyses of average outcomes from the few consistent hospitals in our collaboration as against the other non-participating tertiary hospitals were often assessed via the Proceedings of annual conferences of the Paediatrics Association of Nigerian (PANCONF), notably the January 2016 edition in Port Harcourt city, just following the end of MDG4. At the 2016-PANCONF, abstracts on neonatal mortality‑related topics were published from hospitals that were well-distributed across the country. The topics and geographical locations of the contributing facilities were unplanned and unintended; however, a significantly representative number of reviewed abstracts organically presented enough leeway for a national end-of-MDG4 comparative analyses.4–10 The information was exploited to analyze the comparative impact of the national programs as against the results from our participating tertiary centers (Figure 2).
Many opportunities for useful studies emerged through the CCETH guidance and collaboration. A handful of willing academics across Nigeria and a small group of personal support staff identified with this author’s passion to save the neonates and yielded to his leadership. Hence, he developed a few low-cost, rural village compatible devices that could ensure affordability of essential technologies - incubators, CPAP machine applications, minor assistive breathing devices, and extended reach of oxygen delivery systems, many applying low voltage inputs that could be harnessed from the sun in remote places of the country. The trialed applications, which demonstrated drastic reduction of neonatal mortalities at usage centers, include: the recycled incubator technology (RIT) of Amadi et al. (2010),11 discovery and creation of the antidote to evening fever syndrome (EFS),12 the Handy Approach (HHA)13 and Initial Setpoint Algorithm (HISA),14 the politeheartCPAP machine,15 the politeoxygen splitter system (PSS),16 the polite-light-bank (PLB),17 the mathematical model for the quantification of neonatal thermal-shock and cold-stress,18 and other applications, which are currently in use across neonatal centers in Nigeria.
These are affordable technologies, many of which are reliant on sunlight-harnessed and converted energy for operation, with which Nigerian centers like the Niger-State’s Amina-center in Minna has applied in lowering the regional neonatal mortality rate from 90% to 4% within six years of operation. The combination of these technologies and the training provided for the nurses and the local practitioners have provided a strong intervention confidence which they applied to adequately cater for the needy neonates simultaneously within their rural location, hence revolutionizing the once precarious situations. The Minna mortality reduction shows that the LMICs can be empowered for a self-sustaining and independent healthcare, pushing their own boundaries of development and resilience. The end-of-MDG4 comparative outcomes between the few consistent collaborating hospitals and the corporate Nigerian facilities as drawn from the 2016 abstracts of the Paediatrics Association of Nigeria conference showed that our collaborating centers surpassed the MDG4 target for mortality reduction, which was set at 67%, whereas there was insignificant progress by corporate Nigeria (Figure 2).
The roadmap from initial recognition of this Nigerian need in 1996 to the trialing of the Neonatal Rescue Scheme (NRS) is captured in the itemized narrative of Table 1,19–29 highlighting the various semi-independent researched devices and procedures, which came together to form the constituent elements of the NRS.
|
Research events |
Related publications |
|
|
1. |
Roadmap to the NRS began in 1996. Nigeria high NMR was presented during a meeting at University of Calabar Nigeria |
|
|
2. |
High NMR at facilities blamed on no functional incubators. Hence, the Reprogramming Technique was developed and applied; later modernized & upgraded to Recycling Incubator Technology (RIT) in 2003. Functional incubators became affordable.19 Facilities such as LUTH, UBTH, FMC Owerri, could own and maintain as much as 40 functional thermoneutral systems via RIT by 2014 |
Solution: Amadi et al., 2007, Annal of Trop Paediatr |
|
3. |
Average national NMR at facilities assessed & quantified at 254/’000 presenting neonates11 |
Amadi et al., 2010, Int J Pediatr – six-year RIT impact |
|
WHO 2008 DHS of U5 mortality brought further insight – lack of incubators was not the sole gap, there was knowledge gap + others, Vital information revealed, such as: Neonates = 48% U5MR; >75% NM = premature+VLBW. Nearly 80% mortality occurs during 1st 7 days of life (F7D) What’s going on during F7D? |
Lawn & Kerber, 2006, editors, Opportunities for Africa’s Newborns: practical data. STC UNICEF WHO USAID UNICEF, WHO et al., 2010 &2012, Levels & trends in child mortality report MCA, WHO et al., 2014, Maternal and Perinatal Health Profile of Nigeria, Africa Region |
|
|
4. |
Strategy was necessary to explore and solve other contributing gaps other than affordable incubators |
|
|
Amadi, Mokuolu, & Obasa, 2012, J Neonatal Nurs; solutions: Amadi et al., 2014, Int J Pediatr |
||
|
b. Poor thermoneutral control techniques leading to habitual thermal distress13,14,18 |
Amadi et al., 2015, Paediatr Int Child Health Solutions: the HHA, Amadi, 2012, Tropical Medicine IntechOpen; the HISA, Amadi et al., 2017, J Pediatr Neonatal Care |
|
|
c. Poorly challenged respiratory distress syndrome (RDS)15,16,20,21,22 |
Amadi, Abubakar AG, Abubakar AL, Yusuf, & Usman, 2019, Hypothesis iatrogenic severe hypothermia, EC Paediatr Solution: Amadi et al., 2019, politeheartCPAP machine, Paediatr Int Child Health; Amadi, 2023, politeoxygen-splitter-system, J Pediatr Neonatal Care; Amadi, Obu, & Onwe-Ogah, 2023, politeO2blend, J Pediatr Neonatal Care |
|
|
d. Poorly challenged neonatal jaundice – studied & amplified TBI intervention via the Firefly (MTTS Asia Vietnam)23,24 |
Solution: Amadi et al., 2020, total body irradiation, Paediatr Int Child Health; Onwe, Ezeanosike, Obu, Daniyan, & Amadi, 2019, economic cost savings, J Pediatr Neonatal Care; Amadi et al ... solar-powering phototherapy devices at LMICs – in trialing |
|
|
Solutions: the PBS, in Amadi et al., 2014, Challenges & frugal remedies, Int J Pediatr; Amadi & Kawuwa,2018, in Neonatal Care, IntechOpen; The PLB facility lighting, Amadi & Abubakar, GJMR-K 2023 |
||
|
Interventions: elective certificate course modules on paediatrics intervention techniques, in Amadi et al, Challenges & frugal remedies, Int J Pediatr 2014; Amadi & Kawuwa,2018, in: reducing early mortality, IntechOpen |
||
|
intervention: advocacy for 10% re-shovel limit, in Amadi et al., 2014 Challenges & frugal remedies, Int J Pediatr; Amadi & Kawuwa,2018, in: reducing early mortality, IntechOpen |
||
|
h. Dysfunctional facility building patterns27 |
intervention: Features of frugal, safe & functional neonatal building – studied, implemented, and trialing, Amadi, Kawuwa, Abubakar, & Obaro, 2023: in Best Practices in Neonatal Care and Safety, IntechOpen |
|
|
5. |
The assemblage of researched strategies as integrated package of a regional intervention system that could ensure semi-independence of full neonatal care in hardest-to-reach locations28 |
Amadi, Kawuwa, Abubakar, Adesina, & Olateju, 2022, Neonatal Rescue Scheme: a community integrated concept, J Pediatr Neonatal Care |
|
6. |
Proof of concept of NRS (end-game results) |
|
|
a. Minna Regional cluster: NMR fell 90% to 4% 29 |
Amadi, Abubakar AL, Abdullahi, & Abubakar AG, 2023, J Neonatal Nurs |
|
|
b. CWCH Neoroom >95% rating17 |
Amadi & Abubakar, 2023, polite-light-bank, Global J Med Res |
|
|
|
c. Yobe statewide NRS rollout |
Comprising six regional clusters – project in progress |
Table 1 Roadmap to NRS
This 25 years research journey and development of our frugal neonatal technologies were marred by various competing and well-funded global health ideas within Nigeria – from our analogue Incubator Reprogramming Technique of 1996 to the unveiling of our Neonatal Rescue Scheme (NRS) of 2022.19,28 Many tertiary hospitals were motivated into adopting our ideas of simple technologies that could be sustainably self-funded by the institutions. Hence, these institutions collaborated as we established our research units at each hospital’s facility, encouraging them to own the very projects and be proud of this. Significant progress was made at various times amongst the collaborating hospitals. However, the attention of many of the hospitals soon got diverted by other foreign-funded programs which offered the opportunity to save or make money, but not necessarily better neonatal survival. Therefore, the national collaborative outreach was characterized by inconsistent numbers of participating healthcare facilities, essentially driven by either the commitment or lack of passion of the incumbent chief medical director (CMD) of the respective collaborating hospitals. This dynamic was clearly portrayed in the inconsistency of Nigeria’s corporate neonatal mortality outcomes, from 2007 through 2020, as this suggested to inversely follow the changing national spread of the total number of hospitals collaborating in our activities throughout (Figure 3).
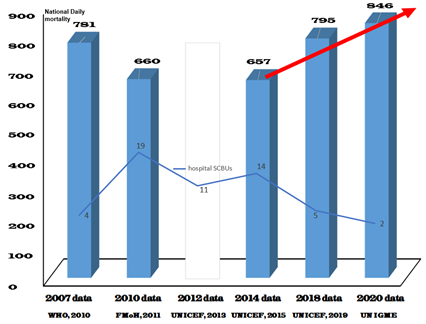
Figure 3 Nigeria average daily neonatal mortality, 2007–2020.
(Information extracted from the various publications of the World Health Organization (WHO), Federal Ministry of Health (FMoH) of Nigeria, UNICEF and UNIGME).
The committee of chief executives of tertiary hospitals (CCETH) of Nigeria, who corporately identified with this outreach in 2007, had at various times intensified or abandoned the emphases for member institutions to stay committed in the collaboration. The leadership changes at CCETH also influenced these emphases leading to a decrease or increase in the number of participating member institutions at various times. At one time, there were up to 18 tertiary hospitals in active participation before leadership changes led to some terminations, for example, between 2010 and 2012. However, later encouragements by the new leadership of the CCETH led to new sign-ups other than those who were previously enrolled. In all, up to 31 Nigerian tertiary hospitals participated in either a test-run or full collaboration at various times, each lasting up to one year or more. Therefore, the national demographic health surveys following the years of a passionate CCETH leader reflected a relatively reduced mortality, and vice versa (Figure 3). We can, therefore, conclude that the collaboration and sustained usage of our frugal technologies in various volumes across the entire country determined how well Nigeria’s corporate performance emerged in the last 25 years.
The collaboration with CCETH died-off owing to lack of leadership interest in 2016 and all active drives ended across the nation, except at three neonatal centers (SCBUs) where the program continued, howbeit, in skeletal form, namely: Alex-Ekwueme Federal Teaching Hospital Abakaliki, Federal Medical Centre Lokoja and the Amina Centre of General Hospital Minna. Figure 3 also demonstrates the negative impact of the total withdrawal of our active drive, leading to the termination of our national program, as Nigeria’s corporate overall NMR has since continued to soar till date.
The assemblage of these frugal technologies into NRS clusters, made up of the hub-centers and neorooms, is a success story that has demonstrated a possible route out of Nigeria’s continuing high neonatal mortality rate.28 Hence, the NRS application has lowered neonatal mortality from 90% to 4% within 6 years of its operation in Niger State whilst the NMR in corporate Nigeria continued to soar.29 The practicing senior nursing officers (SNO) at the Federal Medical Centre Owerri, who participated in the recent review of their NRS-inspired new facility, after one year of usage, independently came out with similar reports of a revolutionary high success rate of practice, as was captured in the book, “Best practices in neonatal care & safety”.27
The few ambitious efforts to scale up the NRS have been hampered by the lack of passion of the successors-in-office to the Chief Medical Directors who initially signed-up the collaboration at their hospitals. Therefore, lack of consistency and continuation of this drive has led to the loss of many lives. Typically, the Yobe State government initiated a drive to roll out a statewide NRS program for trialing in 2016 and commenced with the construction of the hub-center facilities at five regional clusters. However, the project suffered much neglect, without the expected rollout after 2019 when a new state government, who lacked the passion, came into office.
There also seems to be a lack of interest of foreign donor agencies to support the local communities and States who have genuinely embarked on this project but lacked extra funding for good progress. This is regrettable as genuine external assistance could easily boost the morale of many communities or healthcare facilities in their self-help initiatives of managing and sustaining the NRS within their locality to continue to save the precious lives of dying neonates.
This study was supported by Neonatal Concerns for Africa (www.neonatalconcerns.org) organized and managed by Hippolite Amadi in collaboration with the Department of Bioengineering at Imperial College London. The medical missions of Professor H Amadi in Nigeria were morally and prayerfully supported by the Hornchurch Baptist Church, Essex England, United Kingdom (https://www.hornchurchbaptist.org.uk). I acknowledge all technical support and assistance received from Mr Chuks Ugbome, Mr Jude Chima Nzerem and Mr Jerry Okoye. We thank all the doctors and nurses who participated in the various research investigations that were necessary to achieve these results over the last 25 years. I wish to specifically mention some outstanding colleagues and leaders of CCETH whose passion and love for the neonates helped to propel my efforts: posthumously – Jonathan C Azubuike and Isa Dutse; and the rest – Sulema A Kuranga, Peter Alabi, Uriah S Etawo, Akin A Osibogun, Bello M Kawuwa, Emmanuel E Ekanem, Olugbenga A Mokuolu, and Amina L Abubakar.
This research received no specific grant at any time from any funding agency in the public, commercial, or not-for-profit sectors.
The author declares that there are no conflicts of interest regarding the publication of this paper.

©2023 Amadi. This is an open access article distributed under the terms of the, which permits unrestricted use, distribution, and build upon your work non-commercially.