Journal of
eISSN: 2373-4426


Research Article Volume 8 Issue 6
1Rainbow children’s hospital, India
2Department of Paediatrics, GMC, India
Correspondence: Dr. Aakash Pandita, Department of Paediatrics, GMC, Jammu, India
Received: November 30, 2018 | Published: December 21, 2018
Citation: Gupta V, Panigrahy N, Venkatlakshmi A, et al. Diagnostic ability of bedside lung Ultrasound in neonates with respiratory distress. J Pediatr Neonatal Care. 2018;8(6):308-312. DOI: 10.15406/jpnc.2018.08.00364
Background: Lung Ultrasound (LUS) has recently become an important method for diagnostic examination and monitoring of lung disease. Many lung diseases, such as respiratory distress syndrome, transient tachypnea of the newborn, pneumonia, atelectasis and pneumothorax were diagnosed by chest X-ray, but can now easily be diagnosed with lung ultrasound. Lung ultrasound has many advantages over X-ray and CT scan including accuracy, reliability, low-cost and simplicity, as well as the fact that ultrasound incurs no risk of radiation damage. Preliminary data has shown a good sensitivity and specificity of LUS in the diagnosis of respiratory distress syndrome (RDS) and transient tachypnea of the newborn (TTN).
Objective: The aim of this study was to evaluate role of lung ultrasound in neonates with respiratory distress within 6 hours of life and to calculate the sensitivity, specificity, and negative (NPV) and positive predictive value (PPV) of LUS for RDS and TTN, using an external reader blinded to the clinical condition.
Design and Methods: Neonate with gestational age between 28 weeks and 42 weeks who were admitted with respiratory distress had a chest x ray and LUS within first 6 hours of life. Reading of chest X ray for immediate management was done by treating neonatologist by using chest x ray and clinical criteria. Images were uploaded and sent to the external reader, who made the ultrasound diagnosis according to the appearance of the images. Sensitivity, specificity, PPV, and NPV were calculated considering the final clinical diagnosis as the gold standard. The clinical criteria for diagnosing TTN was early respiratory distress (tachypnea and increased work of breathing) with x-ray chest showing a well inflated or hyper inflated lung fields and the condition improved within first 24 to 96 hours after birth. The Clinical criteria for diagnosing RDS was respiratory distress (RD) typically presenting within the first several hours of life, often immediately after delivery. Clinically, these preterm infants have marked respiratory distress with tachypnea, nasal flaring, grunting, and subcostal, intercostal, and/or suprasternal retractions. Furthermore x-ray chest was suggestive of RDS with feature of low lung volume, reticulogranular pattern, ground glass appearance and/or air bronchograms.
Results: Seventy seven neonates were studied (mean gestational age: 32.9±2.5 weeks, mean birth weight: 1,813±625.9g). Forty nine infants had a final diagnosis of RDS and 24 of TTN. LUS showed a sensitivity of 87.7% and specificity of 89.2%, with a PPV of 93.4% and a NPV of 80.6% for RDS, and a sensitivity of 91.6% and specificity of 90.5% with a PPV of 81.4% and a NPV of 96% for TTN.
Conclusion: LUS is a reliable method to diagnose RDS and TTN in newborns with respiratory distress .It showed high sensitivity and specificity in diagnosing RDS and TTN.
Respiratory distress accounts for almost 40% of admissions to Neonatal intensive care unit.1 The respiratory distress syndrome (RDS) and transient tachypnea of Newborn (TTN) are the most common cause of respiratory distress in the preterm and term neonates respectively.2 Chest X-rays are the cornerstone for the diagnosis of respiratory distress (RD). However, distinguishing RDS and TTN may be difficult during the first 24h after birth. Besides, x-rays are not safe for a newborn who is still undergoing maturation. Chest radiography is still the investigation of choice to evaluate the cause of RD in the neonates. However radiography findings are not always diagnostic, it has been shown to be inaccurate in many situations.3 In addition, chest X-ray itself has a wide intra- and inter-observer variability and requires expensive equipment. The adverse effects of irradiation are higher among the Neonates and may be more pronounced in preterms.4 The potential weakness of bedside radiography is explainable by its principle: three dimensions are reduced to two. A CT scan could resolve many of these issues but involves transporting potentially unstable patients out of the department, larger radiation doses (typically 200 times that of a CXR), and the use of contrast makes it unsuitable for routine use in neonates. To circumvent these limitations, ultrasound lung may be a useful tool for the differential diagnosis of RD in newborns. The aim of this study was to determine the diagnostic accuracy of LUS in the evaluation of RDS and TTN in comparison to clinical and chest X ray diagnosis
Study design
All Neonates between 28 weeks and 42 weeks of gestation admitted with RD in the NICU within first 6 hours of life were enrolled after obtaining an informed consent by parents. Both ultrasound chest and CXR were done at admission. CXR was obtained in AP view and was digitalized. Reading of x-ray for immediate management was done by the treating neonatologist but the final interpretation of CXR was done by the radiologist who was blinded to the patient details. Furthermore, to prevent any inter observer variation chest ultrasound was done by the principal investigator. An approval was obtained from the institutional ethical committee for the said study.
Inclusion criteria: All Neonates between 28 weeks and 42 weeks of gestation admitted with RD in the NICU within first 6 hours of life. Respiratory distress was defined as presence of any two of the following: respiratory rate >60 breaths/min, intercostal/subcostal retractions, FiO2 requirement >0.21 and nasal flaring.
Exclusion criteria: Neonates with major congenital anomalies. Outborn admitted within 6 hrs of life but intubated & received surfactant. Consent could not be obtained.
LUS Procedure: A linear probe of 9-12 MHz was used to do the ultrasound of the chest and the sequence of views were anterior chest in vertical and transverse views, mid-axillary vertical and transverse views. Anterolateral parts of the chest wall were examined with the patient in the supine position, whereas posterior parts were examined with the patient in the lateral position. Transthoracic and trans abdominal approaches were also be used for examination. The transthoracic USG approach included examination in supine and both lateral decubitus positions of the anterior (between the sternum and the anterior axillary line), lateral (between the anterior and posterior axillary lines), and posterior (between the posterior axillary line and the spine) lung areas in caudo-cranial direction. The transabdominal USG included the transhepatic and Trans splenic approach in supine position to examine either lung bases ultrasound is performed in the supine, prone, or decubitus position. Images were obtained in the transverse, longitudinal, and inclined transverse or inclined longitudinal planes to maximize visualization of the lung fields.
Ultrasound diagnosis
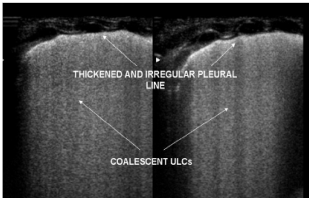
In a typical lung the pleura shows up as a normal echogenic line moving persistently amid breath.5 ‘A lines’, are equidistant lines parallel to straight solid pleural lines, and are reverberation artefacts (Figure 1). B-lines occur when sound waves pass through the pleural line encountering a mixture of air and water as in pulmonary oedema (Figure 2). These are discrete laser-like vertical hyper echoic lines that arise from the pleural line, extend to the bottom of the screen without fading, and move synchronously with lung sliding. The pleural line slides from side to side with respiration and represents movement of the pleural surface with the respiratory cycle. This sign is known as sliding sign, a normal lung feature.6-8 Due to the presence of fluid in normal neonatal lung, B-lines can be found in first few days in normal neonates too.9 In TTN, there are very compact B lines in the inferior pulmonary fields and not so compact B lines in the superior lung field giving a characteristic double lung point sign. Coexistence of lung consolidation, abnormal pleural line (thickness of >0.5mm or blurred), bilateral white lung and disappearance of A lines are constant ultrasonography features of RDS with a specificity and sensitivity of 100%. The most important indicator of RDS is consolidation and the extent and scope of consolidation varies with severity of RDS. Consolidation in moderate RDS is sub pleural and focal in nature whereas consolidation in severe RDS is more widespread and deep.10,11 (Figure 3, 4).

Clinical diagnosis
An analysis of RDS was made if the clinical course and the CXR appearance were concordant. X-ay features suggestive of RDS included diffuse atelectasis, 'ground glass' appearance of the lung fields, low volume lung and air bronchograms.
TTN was considered if there were x-ray findings of hyperinflation, prominent fissure ,perihilar cuffing and the oxygen requirement subsided in 48-72 hours.
Statistical analysis
The results are expressed as mean and standard deviation for continuous variables. The categorical variables are expressed as % frequency distribution. Student t test was applied for continuous variables and proportion test for categorical variables. Fisher’s exact test is used wherever the sample size was low. A value of p <0.05 is considered as significant with two sided tails. The analysis was carried out using the statistical package for social sciences (SPSS 20th version).
During study period total 1157 patient got admitted out of which 537 had respiratory distress. Patient who fulfill the inclusion criteria were 244 but not able to enrolled 167 patient due to principal investigator was not available onsite.
The gestational age of the subjects ranged from 28 to 39 weeks (32.9 weeks, mean 2.5± SD). The mean birth weight was 1813.8 g, 625.9±SD.
Seventy seven patients were enrolled in the study: 7 (10%) were term and 70 (90.9%) were preterm and late preterm.43 (55.8%) were males and 34 (44.1%) were females.
Forty nine infants were diagnosed with RDS and 24 with TTN with the clinical and chest x ray findings. The gestational age of the subjects ranged from 28 to 39 weeks (31.6 weeks, mean 1.95±SD) in RDS group and 35weeks,mean1.8± SD in TTN group. The mean birth weight was 1514.7 g (SD 434) in RDS group and 2270.6(SD 551) in TTN group. The infants of the RDS group had, as expected, a significantly lower birth weight, gestational age.
In RDS group 25 were males and 24 were females and in TTN group 15 were males and 9 were females. Thirty (61.2%) infants were inborn and 19(38.8%) were outborn in RDS group and seven (29.1%) infant were inborn and 17(70.8%) outborn in TTN group.
Surfactant was endotracheally administered in 10 (20.4.5%) patient in RDS group whereas no surfactant received in TTN group. Initial respiratory support was required in Mechanical ventilation was required in all 49 (100%) infants with RDS and 20 (83.3%) in TTN patient.
Mechanical ventilation was required in 14 (18.1%) patient and CPAP was required in 72(93.5%) patient. Surfactant was endotracheally administered in 12 (15.5%) patient.
The cause for respiratory distress from the clinical diagnosis and chest x ray was respiratory distress syndrome (n=49), transient tachypnea of newborn (n=24), meconium aspiration (n=2), pneumonia (n=1) and pneumothorax (n=1) is presented in (Table 2).
|
RDS(n =49) |
TTN(n=24) |
P value |
Birth weight, gram |
1514.7 ± 434 |
2270.6±551 |
0.001 |
<1000 |
2 |
0 |
|
1000- 1499 |
29 |
0 |
|
1500-2499 |
17 |
16 |
|
≥ 2500 |
1 |
8 |
|
Gestational age, weeks |
31.6± 1.9 |
35±1.8 |
0.001 |
28- 30.6 |
18 |
0 |
|
31-33.5 |
23 |
5 |
|
34 – 36.5 |
8 |
14 |
|
>37 |
0 |
5 |
|
Apgar score |
|
|
|
1 min median (IQR) |
7 (6-7) |
7 (6-7) |
0.542 |
5 min median (IQR) |
9 (8-9) |
9 (8-9) |
0.825 |
Gender |
|
|
|
Male |
25 (51.0%) |
15(62.5%) |
0.346 |
Female |
24 |
9 |
|
Inborn |
30 (61.2%) |
7 (29.1%) |
0.006 |
Outborn |
19 (38.8%) |
17 (70.8%) |
0.006 |
Initial Respiratory assistance |
|
|
|
CPAP |
37 (75.5%) |
20 (83.3%) |
|
Mechanical vent |
12 (24.5%) |
0 |
0.006 (Fishers exact test |
Surfactant therapy |
10 (20.4%) |
0 (0.0%) |
0.025 (Fishers exact test ) |
Table 1 Demographic data
Final diagnosis- RD CLINICIAN |
|
RDS |
49 (63.6) |
TTN |
24 (31.1) |
Pneumothorax |
1 (1.2) |
Meconium aspiration |
2 (2.5) |
Neonatal pneumonia |
1 (1.2) |
Total |
77 |
Table 2 Amplitude in mill volts of the Lead-1 of electrocardiography in sheep
*Significant (P≤0.05); NSNot significant (P>0.05)
CXR was performed in all 49 infants with RDS and in 24 in the TTN group.CXR was considered consistent with the final diagnosis of RDS in 40 cases with 9 false negative. CXR showed a sensitivity of 81.6%, a specificity of 96.4%, a PPV of 97.5% and a NPV of 75% for RDS (Table 3). CXR was considered consistent with the final diagnosis of TTN in 19 cases with 5 false negative. CXR showed a sensitivity of 79.1%, a specificity of 98.1%, a PPV of 95%, and a NPV of 91.2% for TTN (Table 4).
|
RDS- Clinician Diagnosis |
Other |
Total |
CXR suggestive of RDS |
40 |
1 |
41 |
CXR not suggestive of RDS |
9 |
27 |
36 |
Total |
49 |
28 |
77 |
Table 3 Correlation of chest x ray diagnosis in neonates with Clinicians Diagnosis of RDS
Sensitivity: 81.6%; specificity: 96.4%; PPV: 97.5%; NPV: 75%
Positive likelihood ratio 22.6, Negative likelihood ratio 0.1908
|
TTN- Clinician Diagnosis |
Other |
Total |
CXR suggestive of TTN |
19 |
1 |
20 |
CXR not suggestive of TTN |
5 |
52 |
57 |
Total |
24 |
53 |
77 |
Table 4 Correlation of chest x ray diagnosis in neonates with TTN and other causes of respiratory distress in neonates
Sensitivity: 79.1%; specificity: 98.1%; PPV: 95%; NPV: 91.2%.
Positive likelihood ratio 41.6, Negative likelihood ratio 0.213
LUS was consistent with the final diagnosis of RDS in 43 of 94 cases, with 6 false negative. LUS showed a sensitivity of 87.7%, a specificity of 89.2%, a PPV of 93.4%, and a NPV of 80.6% for RDS (table 5). LUS was consistent with the final diagnosis of TTN in 22 of 24 cases, with 2 false negative. LUS showed a sensitivity of 91.6%, a specificity of 90.5%, a PPV of 81.4%, and a NPV of 96% for TTN (Table 6).
|
RDS-Clinician Diagnosis |
Other |
Total |
LUS suggestive of RDS |
43 |
3 |
46 |
LUS not suggestive of RDS |
6 |
25 |
31 |
Total |
49 |
28 |
77 |
Table 5 Correlation of lung ultrasound diagnosis in neonates with RDS and other causes of respiratory distress in neonates
Sensitivity: 87.7%; specificity: 89.2%; PPV: 93.4%; NPV: 80.6%.
Positive likelihood ratio 8.1, Negative likelihood ratio 0.137
|
TTN – Clinician Diagnosis |
Other |
Total |
LUS suggestive of TTN |
22 |
5 |
27 |
LUS not suggestive of TTN |
2 |
48 |
50 |
Total |
24 |
53 |
77 |
Table 6 Correlation of lung ultrasound diagnosis in neonates with TTN and other causes of respiratory distress in neonates
Sensitivity: 91.6%; specificity: 90.5%; PPV: 81.4%; NPV: 96%.
Positive likelihood ratio 9.6, Negative likelihood ratio 0.092
The use of ultrasound for immediate management of life-threatening conditions is one among the main changes of these last decades. Lung ultrasound has become more and more popular in the first decade of the 21st century, both in neonatal and in paediatric age groups.
The lung ultrasound may be tool in differential diagnosis of respiratory distress in Newborns.
This study was conducted in a tertiary NICU to evaluate the role of ultrasound in diagnosis of neonates with respiratory distress especially in first 6 hours. Total 77 neonates were included in the study. The sonologist was blinded to the clinical diagnosis and so was the Radiologist blinded when interpreting chest x ray. The authors showed reliable results with LUS to diagnose RDS and TTN in neonates.
According to the findings of our study, the main features of RDS that can be visualized by ultrasound imaging include bilateral white lung or alveolar-interstitial syndrome and pleural line abnormalities and lung consolidation with air bronchograms.
Pleural line abnormality is one of the most common ultrasound observations in RDS patients, but also exists in other lung diseases such as pneumonia, bleeding, and transient tachypnea of the newborn. Therefore, pleural line abnormalities as visualized by ultrasound are not specific to RDS.12 According to the literature, the sensitivity and specificity of pleural line abnormalities for diagnosis of RDS are 100% and 45%, respectively.13
According to the results of this study, the main ultrasonic imaging features of TTN include double lung point, interstitial lung syndrome/white lung, pleural line abnormalities, and A-line disappearance.
In a Study done by Liu et al found most common ultrasonic findings of RDS was lung consolidation with air bronchograms (100%); in addition, pleural line abnormalities, the disappearance of A-lines, and interstitial syndrome could also be seen.
Double lung point was only observed in infants with TTN and not in infants with RDS;14 therefore, the sensitivity and specificity of double lung point for the diagnosis of TTN was 76.7%, but the specificity was 100%.
Double lung point is a specific feature of TTN and lung consolidation is observed only in patients with RDS, Double lung point and lung consolidation with air bronchogram are the most important features for differentiating TTN from RDS using LUS.
Our study is comparable to study by Cattarossi et al. who looked for the lung ultrasound accuracy in respiratory distress syndrome and transient tachypnea of newborn.
In a study by Cattarossi, et al.15 ultrasound chest was done within 1 hour after admission in 4 trans- thoracic views and all are longitudinal views. In their study fifty-nine neonates were studied (mean gestational age: 33±4 weeks, mean birth weight: 2,145±757 g). Twenty-three infants had a final diagnosis of RDS and 30 of TTN.
We include 77 neonates with respiratory distress within 6 hours of life. . In our study (mean gestational age: 32.9±2.5 weeks, mean birth weight: 1813±625.9 g). Forty nine infants had a final diagnosis of RDS and 24 of TTN.
Cattarossi et al.15 study show LUS showed a sensitivity of 95.6% and specificity of 94.4%, with a PPV of 91.6% and a NPV of 97.1% for RDS, and a sensitivity of 93.3% and specificity of 96.5% with a PPV of 96.5% and a NPV of 93.4% for TTN.
In a study by Copetti, et al.16 With the simultaneous presence of three ultrasound findings: abnormalities of the pleural line, white lung image, and absence of spared areas in all lung fields. This profile had sensitivity and specificity of 100% in their series of 55 premature infants.
In a study by Ahuja, et al.17 Trans abdominal USG of lung bases (TASL) in the evaluation of HMD in premature neonates with respiratory distress soon after birth in the diagnosis and follow up of HMD and for the early prediction of BPD.
Subcostal approach for both transhepatic and Trans splenic views were taken and analyzed for retro diaphragmatic echogenicity. Their study showed 85.7% sensitivity, 75% specificity, 88.88% positive predictive value, and 69.2% negative predictive value for the diagnosis of HMD. The abnormal Sonographic findings on day 14 had 94.1% accuracy for prediction of eventual occurrence of clinical BPD.
We obtained a specificity and sensitivity in RDS (87.7 and 89.2%, respectively) and TTN (91.6 and 90.5%, respectively). The PPV and NPV were 93.4 and 80.6%, respectively, in RDS and 81.4 and 96%, respectively, in TTN. We found less sensitivity and specificity as compared to previous studies because we currently introduced this diagnostic tool modality in our unit.
Blinding of the radiologist, and uniform protocol for all the patients are the main strength.
Small sample size and failure to evaluate role of LUS in other lung conditions causing RD in neonates are the major limitations of present study.
The LUS is an upcoming imaging modality for neonates with respiratory distress. It’s not only reliable, feasible; time saving but also avoids harmful radiation exposure seen with the use of x-rays.
VG, NP, AV, DKC cared for the patient and drafted the initial manuscript; Dr AP drafted, reviewed and edited the manuscript; and all authors approved the final manuscript and agree to be accountable for all aspects of the work.

©2018 Gupta, et al. This is an open access article distributed under the terms of the, which permits unrestricted use, distribution, and build upon your work non-commercially.