Journal of
eISSN: 2373-4426


Case Report Volume 14 Issue 2
Department of Pediatrics, Medical College Baroda, Maharaja Sayajirao University, SSG Hospital, India
Correspondence: Dr. Kruti Shah, Senior Resident, Department of Pediatrics, Faculty of Medicine, Medical College Baroda, Maharaja Sayajirao University, SSG Hospital, A/162 Sandalwood society, B/H Vrajdham Temple, Manjalpur, Vadodara, Gujarat, India, Tel +91 8780527050
Received: April 22, 2024 | Published: May 6, 2024
Citation: Shah K, Dave D. Clinical profile, laboratory parameters and management outcomes in an eight-year-old female with childhood lupus nephritis. J Pediatr Neonatal Care. 2024;14(2):105-107. DOI: 10.15406/jpnc.2024.14.00549
Systemic lupus erythematosus (SLE) is a chronic, multisystem, autoimmune disorder characterized by widespread inflammation of connective tissues affecting the skin, joints, kidneys, heart, lungs and nervous system. SLE is most often diagnosed in women during the second to fourth decades of life, but 15-20% cases are found in childhood. Renal involvement occurs in the majority of childhood onset SLE (cSLE) patients and is often fatal and hence constitutes an important determinant of prognosis. Multidisciplinary care is necessary for children with lupus nephritis in terms of immunosuppressive regimes with a common goal of achieving and maintaining renal remission. Despite a low prevalence rate of cSLE, it manifests with fatal complications like lupus nephritis in majority of cases. Renal biopsy is gold standard for staging of lupus nephritis, thus, deciding the modality of management and prognostication of cSLE.
Keywords: childhood lupus nephritis, systemic lupus erythematosus, discoid rashes, renal biopsy, immunosuppressive therapy
SLE, systemic lupus erythematosus; cSLE, childhood onset SLE; ACR, American college of rheumatology; ESRD, end stage renal disease; ISN, international society of nephrology; RPS, renal pathology society
Childhood-onset systemic lupus erythematosus (cSLE) has an incidence of 0.3 to 0.9 per 100,000 children-years and a prevalence of 3.3-8.8 per 100,000 children which constitutes 10-20% of all patients of SLE with a median age of onset of 11-12 years.1,2 Renal disease occurs in 50-75% of all cSLE patients.2 Kidney involvement in lupus often warrants immunosuppression beyond that required for extrarenal manifestations. Renal biopsy is the gold standard for classification of kidney involvement in lupus and primarily drives treatment decisions.
We report a case of an eight-year-old female who presented with complaints of moderate fever, characteristic discoid purple scaly rash on the face sparing the nasolabial folds, on the scalp, lips and other sun exposed areas of body with discolored scarring over some areas with alopecia over the scalp involved regions (Figure 1) with polyarthritis for 10 days.

Figure 1 Picture of an 8-year-old girl with characteristic discoid purple scaly rash on the face sparing the nasolabial folds, on the scalp, lips and other sun exposed areas of body with discolored scarring over some areas with alopecia over the scalp involved regions.
Clinical examination revealed severe pallor with gallop rhythm, pedal edema and signs of congestive heart failure. She also had reduced urine output suggesting multi-systemic involvement. On investigating, blood picture revealed anemia (hemoglobin levels were 5.7gm/dl), thrombocytopenia (platelet counts: 102,000/microliter), total leukocyte counts were 8900 /microliter with a normal reticulocyte count of 0.5%, high LDH levels (769 U/L) and normal serum ferritin levels (47ng/ml). The cause of anemia was secondary to immune hemolysis as the Direct Coombs Test was positive (+2). CRP was 79mg/dl and ESR was 90mm/hr. Renal function was deranged. Blood urea nitrogen levels were 42 mmol/ liter and serum creatinine was 1.21 mg/dl with hyperkalemia with serum potassium levels were 4.6 mEq/ L. Urine microscopy suggested proteinuria (+1) with 24 hours urinary protein 0.3 gm/day. Hematuria with 20-30 RBCs/ hpf with epithelial granular casts (+2) was found. Liver function was unremarkable with cardiac 2D Echocardiography being normal. With the evidence of clinical features and immune hemolysis, polyarthritis with renal involvement, autoimmune profile was sent which showed presence of a positive Anti-Nuclear Antibody titer of 1:100 with a homogenous cytoplasmic granular pattern (+3) on immunofluorescence and anti-Ds-DNA antibodies (+2), anti-nucleosomes antibody (+1), anti-histone antibody (+1), anti-ribosomal P protein antibody (+1) with low serum C3 complement levels ( 64.7mg/ dL) and low serum C4 complement levels (6.10mg/ dl) was found remarkable; thus confirming the diagnosis of childhood onset systemic lupus erythematosus with a Clinical domains and criteria score of 42.3
With this strong evidence of SLE with changes of nephritis, a renal biopsy was done to stage the disease and decide the further line of management. The renal biopsy on light microscopy showed mesangial hypercellularity and acute tubular inflammation with minimal immune deposits and occasional glomeruli showing mild focal polymorph infiltrate which represented Class II lupus nephritis with developing Class III lupus nephritis. The immunofluorescence microscopy was weakly positive for IgG, IgM IgA antibodies, Complement C3, Complement C1q in mesangium and glomeruli and negative in tubules and vessels. Hence, on confirming the diagnosis of childhood onset SLE with developing Class III Lupus Nephritis, the patient was offered pulse doses of methylprednisolone at 30mg/kg/day for 5 days followed by oral corticosteroids at 2mg/kg/day for 9 months and immunosuppressive steroid sparing agents with six cycles of monthly Cyclophosphamide at 500mg/m2/day with Mesna at 200mg/m2 and oral Mycofenolate Mofetil at 500mg/m 2/day for 9 months with life-long Hydroxychloroquine treatment. With this immunosuppressive regime, after 10 days of treatment, the child went into renal remission (blood urea nitrogen 30.80, serum creatinine 0.85mg/dl) and correction of anemia (Hemoglobin was 10.gm/dl) and complete resolution of skin changes by 6 months (Figure 2). Thereafter, the child is followed up on outpatient care for assessing the therapeutic response and relapse of active disease.
Childhood onset SLE (cSLE), despite a lower incidence, has fatal complications with occurrence of renal disease in 50-75% of all cSLE patients, mostly within the first two years of diagnosis with a poor prognostic value.2 Lupus nephritis is hypocomplementemic glomerulonephritis. Initial manifestations of renal disease range from minimal proteinuria and hematuria to nephrotic-range, rapidly progressive glomerulonephritis, severe hypertension, and acute kidney injury. As per the American College of Rheumatology (ACR) criteria, lupus nephritis is defined as persistent proteinuria (>0.5 g/day or >3+ by dipstick) and/or cellular casts in the urine. A spot urine protein/creatinine ratio of >0.5 can be substituted for the 24-hour urine protein measurement and an ‘active urinary sediment’ (>5 RBC/high power field (hpf), >5 WBC/hpf in the absence of infection, or cellular casts limited to red blood cells or white blood cell casts) can be substituted for cellular casts.4 Initial manifestations of renal disease range from minimal proteinuria and hematuria to nephrotic-range, rapidly progressive glomerulonephritis, severe hypertension, and acute kidney injury. Nephritis is a major risk factor for morbidity and mortality in SLE and 10% of patients with lupus nephritis will develop end stage renal disease (ESRD) with a higher risk in patients with more severe histological classification.5 In cases where there might be a lack of clinico-pathologic correlation, a renal biopsy is accepted gold standard diagnosis. Histopathology is essential in guiding treatment modality, pressing its strong recommendation for all patients with clinical evidence of lupus nephritis to classify nephritis and evaluate progressiveness, severity and chronicity.6,7 The recommendations of the International Society of Nephrology (ISN) and the Renal Pathology Society (RPS) revised in 2018 are currently used as the basis for the classification of lupus nephritis (Figure 3).8
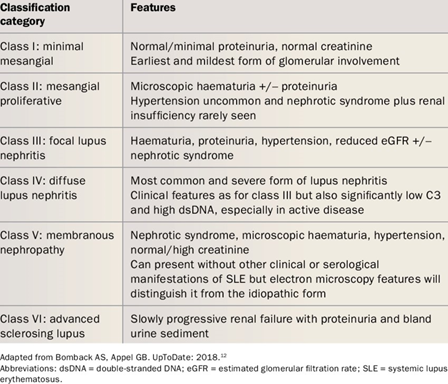
Figure 3 Histopathological classification of lupus nephritis as per WHO Class and ISN/RPS nomenclature.
Multidisciplinary care is necessary in children with SLE. General management includes induction and maintenance phases of administration of steroid sparing agents as per the histological class of lupus nephritis suggested by International Society of Nephrology Classification (Figure 4), hydroxychloroquine sulphate and application of sunscreen in children.
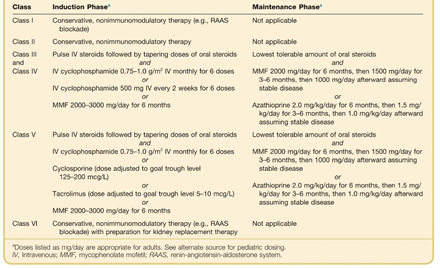
Figure 4 Treatment options for lupus nephritis stratified by International society of nephrology classification and phase of therapy.
Consequently, angiotensin converting enzyme inhibitors for hypertension/ proteinuria with HMG CoA inhibitors for dyslipidemia and vitamin D3 supplements are used as supportive management.
Childhood onset systemic lupus erythematosus is a multisystem disease with protean manifestations. Despite a low prevalence rate of cSLE, it manifests with fatal complications like lupus nephritis in majority of cases. Renal biopsy is gold standard for staging of lupus nephritis, thus, deciding the modality of management and prognostication of cSLE. Multidisciplinary approach with immunosuppressive therapy forms the base of treatment for lupus nephritis.
None.
None.
The authors declare that there are no conflicts of interest.

©2024 Shah, et al. This is an open access article distributed under the terms of the, which permits unrestricted use, distribution, and build upon your work non-commercially.