Journal of
eISSN: 2373-4426


Case Report Volume 13 Issue 3
1Department of Pediatrics, University Santiago de Compostela (USC), Spain
2Department of Pediatric Surgery, University Santiago de Compostela (USC), Spain
3Department of Radiology, Hospital Alvaro Cunqueiro, University Santiago de Compostela (USC), Spain
Correspondence: Pilar Fernández Eire, Department of Pediatrics, Pediatric Surgery Hospital Alvaro Cunqueiro Estrada Clara Campoamor- 325, 36212 Vigo, Spain, Tel 34-986811111
Received: September 02, 2023 | Published: September 28, 2023
Citation: Espinosa Pereiro CE, Fernández Eire P, Berbel Rodríguez A, et al. Choledochal cyst in association with agenesis of the gallbladder. What is the best diagnostic method?. J Pediatr Neonatal Care. 2023;13(3):181-182. DOI: 10.15406/jpnc.2023.13.00513
This manuscript presents the review of a clinical case late diagnosed due to the lack of symptoms and clinical signs associated with the very rare association of choledochal cyst and gallbladder agenesis. This led to multiple radiological tests being performed in an attempt to reach a correct diagnosis.
We report the case of a 9-year-old-girl with self-limited episodes of vomiting and abdominal pain for years that was finally diagnosed with gallbladder agenesis and choledochal cyst. Due to the possibility of malignancy of the choledochal cyst (especially in types I and IV of the Todani classification), she underwent surgery by performing a resection of the cyst and a hepaticojejunostomy.
Parental informed consent and ethical board clearance was obtained, although no data that could identify the patient is presented.
Keywords: Gallbladder diagnostic imaging, choledochal cyst, hepatobiliary surgery in children
Gallbladder agenesis (GA) is a very rare congenital anomaly which shaded clinical and radiological features which make the preoperative diagnosis really challenging, especially when it is associated with other biliary and extrabiliary anomalies.1
The combination of GA and choledochal cyst (CC) is extremely rare, even though it has been identified biliary atresia and CC in the antenatal screening.2–4
In spite of those features, nowadays more and more cases are diagnosed thanks to great technological innovations. The most important thing is to make an adequate preoperative diagnosis, in order to avoid further surgical damage.3–5
Cholangioresonance is the most used test today. Endoscopic retrograde cholangiography can offer good anatomical images but it is a very invasive method. Its use in children of young age and weight is very limited.6 Both clinical presentation and radiological findings may mimic other biliary diseases, which can lead to misdiagnosis and improper treatment especially in children. Due to its infrequency it is not easy to think about it.5
A 9-year-old girl presented a history of recurrent episodes of dyspepsia, vomiting and diffuse abdominal pain. Her past medical history included short stature, heart valve disease with paroxysmal supraventricular tachycardia, vesicoureteral reflux, uterus didelphys and sellar cyst. Also she had undergone many ultra-sonographic studies, magnetic resonance cholangiography, CAT-scan and multiple medical and endoscopic treatments (for reflux) in the previous years due to all the pathologies that she had presented since her birth.
No other symptoms and signs were associated during “attacks”. Laboratory tests were always normal during the episodes. During a new episode (9 year-old) other ultrasound was performed. A cyst was observed in the hepatic hilum and the gallbladder fossa was apparently empty (Figure 1: A, B). Trying to clarify the anatomy a CT-scan was perfomed and an upper gastrointestinal contrast study to rule out a duodenal duplication cyst. Again other Magnetic Resonance Cholangiopancreatography (MRCP) was accomplished (Figure 2).
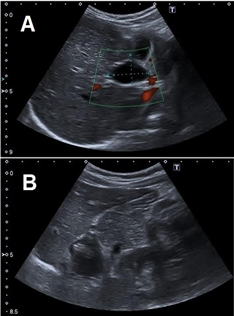
Figure 1
A: Ultrasound scans showing a Cystic formation in the hepatic hilum.
B: Gallbladder fossa apparently empty, suggestive of “atrophic gallbladder”.

Figure 2 Coronal MRCP T2 image shows a cystic ductal formation in the hepatic hilum (arrow) suggestive of a choledochal cyst.
An Endoscopic Retrograde Cholangiopancreatography (ERCP) was attempted without success, and an exploratory laparoscopy was performed where multiple adhesions in the hepatic hilum were observed which prevented a proper visualization. Finally, an exploratory laparotomy was done, finding an agenesis of the gallbladder and cystic duct as well as a type I choledochal cyst. Intraoperative cholangiopancreatography was undertaken showing intrahepatic bile ducts and confluency of hepatic ducts without any dilatation, entering then the lateral wall of the cyst. An omphalomesenteric duct was also found, which was considered to be the probable cause of the symptoms.
Excision of the omphalomesenteric duct and the choledochal cyst and reconstruction by hepaticojejunostomy was carried out. The patient was discharged after 7 days without complications. The pathology report confirmed the diagnosis.
The postoperative period had no incidence and after more than 2 years of evolution the patient is asymptomatic.
The combination of GA and choledochal cyst (CC) is extremely unusual.2,4 GA is classified into three types:
GA maybe associated with other biliary anomalies including biliary atresia or choledochal cyst but this, is even rarer.4
When the gallbladder is not properly visualized on abdominal ultrasound, we should consider agenesis of the gallbladder. We think that in our patient the choledochal cyst was misinterpreted as the gallbladder and the all subsequent studies, for a long time, were based on that initial erroneous diagnosis.
MRCP is the preferred imaging modality given that ERCP is an invasive technique with potential risks, and it can avoid an unnecessary surgery in case of isolated agenesis of the gallbladder.3–7 If the diagnosis remains unclear, it can be clarified with laparoscopy or even perform a laparotomy if the radiological findings justify it and according to the availability and experience of the surgical team.2–5,8
This case describes an extremely rare association between gallbladder agenesis and atypical CC and the complexity of its diagnosis and surgical treatment.9,10
We believe that pathological ultrasound findings in the hepatobiliary tree should be confirmed by more sensitive and specific radiological tests such as magnetic resonance cholangiography and even exploratory laparoscopy which can become therapeutic if adequate resources are available.
None.
All the authors approved the final version of this paper.
Parental written consent was obtained for the publication of the report.
The authors have not declared a grant for this research from any funding agency in the public, commercial or not-for-profit sectors. This investigation has not received specific contributions from public sector, commercial sector or nonprofit entities.
The author declares no conflicts of interest.

©2023 Espinosa, et al. This is an open access article distributed under the terms of the, which permits unrestricted use, distribution, and build upon your work non-commercially.