Journal of
eISSN: 2373-4426


Case Report Volume 9 Issue 5
University of Tennessee Health Science Center, USA
Correspondence: Tsega Temtem, University of Tennessee Health Science Center, 51N. Dunlap, Memphis TN 38103, Tennessee
Received: July 31, 2019 | Published: September 3, 2019
Citation: Temtem T. Biliary botryoid rhabdomyosarcoma in a pediatric patient. J Pediatr Neonatal Care. 2019;9(4):121-123. DOI: 10.15406/jpnc.2019.09.00391
Biliary rhabdomyosarcomas are rare, making up about 1% of all liver malignancies. These tumors are often an embryonal subtype and generally large, measuring multiple centimeters. We present an 11-year-old female with a history of intermittent painless jaundice and imaging suspicious for a choledochal cyst. Endoscopy identified a lesion protruding from her ampulla, and pathology diagnostic of a botryoid variant of embryonal rhabdomyosarcoma. She improved with chemotherapy and radiation. Botryoid biliary rhabdomyosarcomas typically have rapid growth with early presentation of jaundice around 3.5years old; however, this case was reported in an older child with a protracted history of intermittent jaundice.
Keywords: rhabdomyosarcomas, jaundice, pathology, diagnostic, embryonal, polypoid
MRCP, magnetic resonance cholangiopancreatography; VAC, vincristine adriamycin and cyclophosphamide
Biliary rhabdomyosarcomas are a rare malignant tumor of the bile ducts, making up about 1% of all liver malignancies. The most common subtype is embryonal with botryoid features. These tumors progress rapidly and present early in childhood, with an average age of 3.5years. At diagnosis, they are typically large, often measuring multiple centimeters in diameter and having a polypoid appearance in the biliary ducts. Symptoms include jaundice in about 80% of patients, as well as abdominal distension and hepatomegaly. Patients often require surgical excision, as well as chemotherapy and radiation. 5-year survival with this treatment course is around 66%. Here, we present an 11-year-old female who was asymptomatic except for intermittent jaundice, atypical findings on imaging, and pathology diagnostic of embryonal rhabdomyosarcoma of the biliary tract.
An 11-year-old girl with history of sickle cell trait and allergic rhinitis presented to the emergency department for pruritus. She had been evaluated at an urgent care clinic three weeks prior for generalized rash and pruritus, and was diagnosed with contact dermatitis. At current presentation, rash had resolved but she had persistent pruritus. No abdominal pain. She had scleral icterus, but family reported this was not uncommon as it occurred for over a year and seemed to get worse with her “seasonal allergies”. Initial assessment showed a thin nontoxic appearing girl with normal vital signs and an exam significant for icteric sclerae, excoriations but no rash, and a nontender abdomen with liver palpable 2cm below the right costal margin. Laboratory results showed elevations in direct bilirubin, alkaline phosphatase, and GGT. Ultrasound showed intrahepatic biliary dilation with an echogenic area in the common hepatic duct suggestive of sludge. She had a magnetic resonance cholangiopancreatography (MRCP) that showed diffuse dilation of the intrahepatic, common hepatic, and common bile ducts; a distended gallbladder; and a T2 hypodense lesion in common bile duct extending into common hepatic duct that was consistent with biliary sludge (Figure 1), with suspicion for choledochal cyst. She then had an upper endoscopy, which was significant for a lesion protruding from the ampulla that had the appearance of a blood clot. It was extracted after sphincterotomy, and noted to have a thin stalk-like attachment, measuring 1.3cm in length, which was partially resected and sent to pathology (Figure 2&3). Pathology was significant for a polypoid tumor with variable cellularity, and “tadpole” shaped cells having cytoplasmic cross striations, and a high proliferative index by Ki67 stain. These findings were diagnostic of a botryoid variant of embryonal rhabdomyosarcoma. She was started on chemotherapy with vincristine, adriamycin, and cyclophosphamide (VAC), and improved with this regimen. She has not required surgery or radiation (Figure 4A-4C).
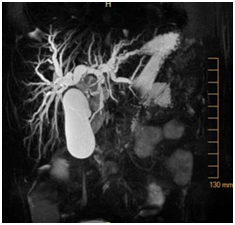
Figure 1 Magnetic resonance cholangiopancreatography (MRCP) showing diffuse dilation of the intrahepatic, common hepatic, and common bile ducts; distended gallbladder. T2 hypodense lesion in common bile duct extending into common hepatic duct, consistent with biliary sludge.
Bile duct rhabdomyosarcomas are quite rare and have been described only in small case series and case reports, and they present a malignant cause of biliary obstruction. They are rapidly progressing, with an average age of presentation around 3.5 years, and they are most often the embryonal subtype with botryoid features. Around 80% of cases present with jaundice, and sometimes also fever, hepatomegaly, and abdominal distension. Laboratory values usually reflect biliary obstruction. Tumors are typically large and thus visible on imaging. The success rate of surgical resection alone is less than 50% due to local extension into the liver. The recommended management includes biopsy of the mass for diagnosis and staging followed by chemotherapy and radiation, which results in a 5-year survival of around 66%.
Our patient’s painless protracted jaundice and the small tumor size are atypical as biliary rhabdomyosarcoma typically presents with rapid growth and subsequent clinical manifestation. The differential for jaundice in an older child is broad, including various viral infections, autoimmune etiology, obstruction such as cholelithiasis or choledochal cysts, metabolic disease, or inherited diseases of cholestasis. Referral to a pediatric gastroenterologist is recommended as preliminary evaluation for these more common etiologies should be performed in patients with protracted jaundice. Gilbert syndrome should be considered in children presenting with episodic painless scleral icterus occurring during periods of physical stress, although this is seldom detected prior to puberty. Our patient described worsening of jaundice related to seasonal allergies, however this historical account is likely inaccurate as jaundice due to rhabdomyosarcoma should not be intermittent in nature. A reasonable differential diagnosis in this patient is a choledochal cyst. These are congenital biliary tree abnormalities characterized by cystic dilation of intrahepatic or extrahepatic bile ducts and can present at any age with a female predominance. The triad of this condition includes abdominal pain, a right upper quadrant mass, and jaundice, although this is triad is not always seen. The most common presentation is cholestasis, as seen in our patient, and ultrasound may show cysts and biliary duct dilation.1‒8
Regarding choice of imaging, ultrasound is typically the initial study utilized when laboratory data or history are suggestive of an obstructive jaundice. This may show dilation of bile ducts and in some cases of larger masses, it may identify presence of a tumor. Magnetic resonance imaging should be employed to further assess the etiology and characteristics of the obstruction. In this case report, the patient’s imaging showed diffuse dilation of the biliary tree which could suggest choledochal cyst. On retrospective review of the clinical case, imaging with contrast may have provided more information regarding the diagnosis; however this would not have changed her clinical outcome as she ultimately would have required intervention, whether endoscopic with ERCP or surgical. While rare, our case illustrates the importance of considering malignancy in cases of obstructive jaundice, particularly if imaging and presentation are not classic for common causes.
None.
The authors declared there is no conflict of interest.
None.

©2019 Temtem. This is an open access article distributed under the terms of the, which permits unrestricted use, distribution, and build upon your work non-commercially.