Journal of
eISSN: 2373-4426


Research Article Volume 11 Issue 4
1Shone primary hospital, Shone, Ethiopia
2Department of midwifery, Hosanna College of health science, Ethiopia
Correspondence: Mengistu Lodebo Funga, Midwifery department, Hosanna College of Health Sciences, Hosanna, Ethiopia, P.O.Box 159, hosanna; Ethiopia
Received: April 24, 2021 | Published: December 31, 2021
Citation: Thomas M, Lodebo M. Assessing practice of essential new born care and associated factors among mothers who gave birth last 6 months in east Badewacho Woreda, Hadiyya Zone, Ethiopia. J Pediatr Neonatal Care. 2021;11(4):66-73. DOI: 10.15406/jpnc.2021.11.00446
Purpose: Globally, more than 2.7 million new-borns die before reaching neonatal age every year and most of the new born deaths occur at home. Half of these surprisingly occur within the first 24 h of delivery and 75% occur in the early neonatal period. Promotion of essential new-born care practice is one of a cheap approach to improve health outcomes of new-born babies. Thus, this study was aimed to assess essential new born care practice and associated factors among mothers who gave birth last 6 months in East Badewacho woreda, Hadiyya zone.
Patient and methods: Community based cross sectional study design was done from March 1 to April 30, 2018. The sampled population were 399 mothers who gave live births within the last six months prior to actual data collection using multistage random sampling technique. Data was collected by using semi-structured questionnaire and entered in Epi-data version 3.1 then exported into SPSS version 21 for analysis. Binary logistic regression analysis with 95 % CI was carried out.
Result: Less than half (34.1%) of the mothers were utilized essential new born care. Educational status of the husband [AOR=0.24,CI(0.089,0.64)] and [AOR=0.314,CI(0.126,0.78)], place of delivery
[AOR=0.024,CI(0.009,0.068)] and knowledge on essential newborn care [AOR=2.03,CI(1.223,3.371) were significant predictors for utilization of essential newborn care.
Conclusion: The study result revealed that practice of essential newborn care in East Badewacho Woreda was low. Therefore, enhance linkage of health centers with health posts to increase ANC, institutional delivery and PNC service utilization.
Keywords: Essential, Ethiopia, Knowledge, Newborn care, practice
ENC, Essential Newborn Care; NMR, Neonatal mortality rate
Essential new born care (ENC) is a set recommendation that designed to improve the health of new-borns through interventions before conception, during pregnancy, at and soon after birth and in the postnatal period. It includes thermoregulation, clean delivery and cord care, initiation of breastfeeding, immunization, eye care, recognition of danger signs, care of the preterm or low birth weight infant and management of newborn illnesses.1,2
Neonatal mortality is one of the world’s most neglected health problems. It is estimated that globally, 2.7 million neonates die before they reach one month of age and 98 % of this neonatal deaths occur in low and middle-income countries. Most of neonatal deaths are preventable regardless of whether delivery was in the home or in a health care facility, and regardless of whether a skilled attendant was present at birth. The major contributing factors for neonatal mortality include: Unhygienic cord care, Neonatal hypothermia (early bathing), lack of early breastfeeding, lack of identification and appropriate referral of sick neonates.3-5 Neonatal mortality rate (NMR) in Africa remains the highest at 32 deaths per 1,000 live births contributing 38% to the global NMR and 30% to the continental burden of under-five mortality.6
In Ethiopia, around 87,000 newborns die every year in the first one month of life. The risk of death is highest in the first 24 hours of life when more than half of deaths occur and about three-quarters of all neonatal deaths occur within the first weeks of life and most of neonatal deaths occur at home. According to 2016 national report in Ethiopia the NMRs were estimated to be 29 per 1000 live births. Also, in Southern Nation Nationalities and peoples regions (SNNPR) the NMRs were estimated to be 35 per 1000 live birth which is somewhat higher than national report.7,8
Several factors have been identified as barriers to access care to the newborn especially in developing countries; these include unavailability of the services, inadequate number of skilled personnel, geographical inaccessibility and poor quality of care, financial constraints, no perceived need for such services, cultural practices, mothers awareness or knowledge about newborn care, maternal health and socio- demographic characteristics.9 Evidence from different studies which was conducted in Ethiopia stated that mothers have poor utilization regarding to the ENC. This shows that newborn care is strongly influenced by home care traditional practices in the community.10-14
According to Hadiya zone health office report neonatal deaths were estimated to be 23 per 1000 live births in 2017/18. Assessment of practice on essential new born care was one of the key prerequisite information required in designing strategy that can improve newborn health outcomes and end the preventable causes of neonatal morbidity and mortality. Also mothers utilize on essential new born care is important for promotion essential new born care and for reducing of neonatal death. Therefore, the aim of this study was to assess the practice of essential newborn care and its associated factors among mothers in East Badewacho Woreda, Hadiyya Zone, South Ethiopia.
Study design and setting
A Community based cross sectional study design was conducted among mothers with an infant less than six months old in East Badewacho woreda, Hadiya zone, Southern Ethiopia from March 1, 2018 to April 30, 2018. The East Badewacho woreda is located at 342km far in the south from Addis Ababa and about 121 Km far from Hawassa and 97 Km in East from the Zonal capital of hosanna.
According to woreda health office report total population were 175,660 and 2130(1.23%) of the mothers had less than six month of age children in the woreda.
Sample size determination and sampling technique
By comparing the sample size of each objective we take the largest sample size which was 242, then by considering non-response rate 10% and design effect 1.5 the final sample size would become 399.n= [(242x0.1) +242) x1.5)] =399 (Table 1).
|
Prevalence |
Proportion |
Formula |
Sample size |
Objectives |
P1= knowledge on essential newborn care |
P1=80.4% |
Single population |
|
P2= practice on essential newborn care |
P2=92.9 |
Single population |
101 |
|
P11= factors associated with knowledge of ENC |
P11*=69% |
Epi info7 software |
168 |
|
P22= factors associated with practice of ENC |
P22*=79% |
Epi info7 software |
160 |
Table 1 Sample size determination for outcome variables and associated factors15
Multi-stage sampling technique was employed for the Selection of the study population. Initially, the woreda is stratified as rural and urban kebeles. In East Badewacho woreda there are 33 rural and 3 urban Kebeles. From those, 10 Rural and 2 Urban Kebeles were selected by using lottery method. According to data obtained from East Badewacho woreda health office, those mothers who have less than six month old infants were estimated to be 2130. Among those, 793 mothers gave a birth in the last six month in selected Kebeles.
Those mothers who had gave a live birth in the last six (6) months from August 28, 2017 to February 28, 2018 was taken from family registration folder from each selected Kebeles health post and coded before actual data collection to create a sampling frame. Sample size was determined proportionately to each Kebeles. Study participants were selected by Simple random sampling method from coded mothers once proportionately to size allocation. Again, the selected mothers ticked by name and address from registered mothers in each health post were given to HEWs and leaders.
The name and addresses of mothers who have less than six month old infants are specified and locations would be identified in collaboration with the Kebele’s HEWs and leaders. The identified mothers who have less than six months infant were interviewed by house to house visit. Selected study participant who refused to participate in this study was considered as non-respondent.
Data collection instrument
The semi structured questionnaire was adapted from 2016 national report and previously done related studies.7,15,16 It consists of information on socio-demographic characteristics (15 question), Obstetric characteristics (10 question) and Utilization of the mothers on ENC (19 question). Finally, the questions related to knowledge and utilization on ENC was dichotomized into good and poor based operational definition.
Data collection procedure
The data was collected from March 1-30/2018 from selected Kebeles. It was collected from all selected Kebeles by face to face interviewing the mother using hadiyisa language version instrument. A respondent who was not present at home during data collection time were revisited. Two BSc nurses for supervision and six diploma nurses for data collection were recruited.
Data processing and analysis
The collected data was checked manually for its completeness and consistency before data entry. The gathered data was coded, cleaned and entered into Epi-data version 3.1 and export to SPSS version 21 for data analysis.
Descriptive analysis such as statements, tables, charts and graphs were used to present the result of analysed data. Binary logistic regression was performed. Both bivariate and multivariate logistic regression models were used to determine factors associated with utilization of ENC.
To identify factors associated with utilization of essential newborn care, variables with P-value ≤ 0.25 in the bivariate logistic regression were entered into multivariate logistic regression model. The statistical association between the different independent variables in relation to dependent variables were measured using OR at 95% CI. P-values <0.05 in multivariate logistic regression was considered as statistically significant. Model of fitness were checked by Hosmer and Lemeshow statistics test and its p-value were equals to 0.824.
Data quality management
The semi structured questionnaire already prepared in English was translated into local language hadiyisa, and then retranslated back to English in order to ensure its consistency. The pre-test was done on 5 % of sample size outside of the study area in west Badewacho woreda which is 18km far from the study areas. Sequences of the question, grammar and spelling errors were amended. The Cronbach’s α test was used to assess the internal reliability of the questions pertaining to socio-demographic characteristics, which was 0.87, Obstetric characteristics, which was 0.75and relating to practices on ENC, which was 0.8.
Six diploma nurses were recruited to conduct an interview. Two supervisors’ who has first degree in nursing were assigned to supervise the data collection process with the responsibility of supporting the data collectors, checking filled out questionnaires daily for completeness and providing feedback for data collectors. Data collectors and supervisors were selected based on the ability to speak the local language hadiyisa and previous experience of data collection.
Training was given for one day on the area of the objective of the study, relevance of the study, confidentiality of information and techniques of interview for data collectors and supervisors. Supervisors would supervise and check their respective data collectors during data collection time. Every questionnaire was cross checked daily by the supervisor’s and principal investigators. Problems faced during data collection were discussed over night with data collectors and the supervisors.
Ethical considerations
Ethical clearances were obtained from the institutional Review Board (IRB) of Jimma University, institute of Health faculty health science. Official letter were written from school of Nursing and Midwifery to East Badewacho woreda health office. Similarly, verbal consent was obtained from each study participant after explanation of the objective of the study. All responses were kept confidential.
Socio demographic characteristics of respondent
A total of 387 mothers were participated in the study yielding a response rate of 97%. Accordingly, analysis was done based on 387 participants. The women’s age range from 18 to 39 years, with a mean of 26.85 (± 5.42) years. Half of the respondents (51.4%) were between the ages of 25-34 years. Three hundred seventy three (96.4%) of respondents were married. Regarding to educational status, 164(42.5%) of the mothers were completed primary level and 144(37.2%) of the husbands were complete secondary level. Regarding to their religion and ethnicity, 292(75.5%) of the respondents were protestant and 291(75.2%) of the respondents were Hadiya. Concerning their occupation, 252(65.1 %) of the mothers were house wives (Table 2).
Variables categories |
Frequency |
Percent |
|
Age of the mother |
18-24 |
139 |
35.5 |
Residency |
Rural |
323 |
83.5 |
Religion
|
Protestant |
292 |
75.5 |
Ethnicity |
Hadiya |
291 |
75.1 |
Marital status |
Married |
373 |
96.4 |
Educational status
|
Not educated |
64 |
16.5 |
Educational status |
Non educated |
29 |
7.5 |
Mother’s occupation
|
House wife |
252 |
65.1 |
Husband’s occupation |
Gov’t Employee |
97 |
25.1 |
Monthly income
|
<1000 |
76 |
19.6 |
Age of the child |
<3 months |
122 |
31.5 |
Sex of the child |
Male |
235 |
60.7 |
Table 2 Socio demographic characteristics of women in East Badewacho woreda, Hadiya Zone, Southern, Ethiopia 2018 (n=387)
*,Oromo, Tigre, Amahara;**,divorced &single
Source of information
Among the respondents, 157(40.6%) of mothers were heard about ENC. From them 90 (57.3%) of the mothers were heard from health professional and 151(96.2%) of the mothers were heard about breast feeding (Table 3).
Variables |
Categories |
Frequencies |
Percent |
Ever heard about ENC |
Yes |
157 |
40.6 |
Source of information, ever heard about ENC |
Health professional |
90 |
57.3 |
HEWs |
68 |
43.3 |
|
Mass media |
58 |
36.9 |
|
Relative and friends |
15 |
9.5 |
|
Areas of information heard about ENC |
Breast feeding |
151 |
96.1 |
Cord care |
81 |
51.6 |
|
Thermal care |
84 |
53.5 |
|
Immunization |
123 |
78.3 |
|
Neonatal danger sign |
29 |
18.4 |
Table 3 Source of information of the mothers on ENC in East Badewacho woreda, Hadiya Zone, Southern Ethiopia 2018 (n=387)
Obstetric characteristics of respondent
Out of the total respondent, 316 (81.7%) of the mothers attended ANC follow up during last pregnancy and 249 (78.8%) of the mothers followed four times and above. In case of counselling about ENC during ANC, only130 (41.1%) of the mothers were counselled about ENC and 118(90.7%) of the mothers were received counselled on breast feeding.
Three hundred thirty six (86.4%) of study participants were gave birth at health institution while only 152(39.3%) of the respondents attended PNC follow up and 132(86.8%) follows one times. Concerning counselling about ENC during PNC follow up, 118(64.4%) of the mothers were counselled about ENC and 76(64.4%) of the mothers were counselled on breast feeding (Table 4).
Variables |
Categories |
Frequency |
Percent |
|
|
Number of pregnancy |
<2 |
127 |
32.8 |
|
|
Number of child born alive |
<2 |
124 |
32 |
|
|
ANC follow up during last pregnancy |
Yes |
316 |
81.7 |
|
|
Times of ANC follow up |
one times |
10 |
3.2 |
|
|
Counselled about ENC during ANC |
Yes |
130 |
41.1 |
|
|
No |
186 |
58.9 |
|
||
Area of counselling during ANC |
Breast feeding |
118 |
91.5 |
|
|
Cord care |
79 |
60.7 |
|
||
Thermal care |
76 |
58.4 |
|
||
Immunization |
90 |
69.2 |
|
||
Neonatal danger sign |
19 |
14.6 |
|
||
Place of delivery |
At health institution |
336 |
86.4 |
|
|
At home |
51 |
13.6 |
|
||
PNC follow up |
Yes |
152 |
39.3 |
|
|
No |
235 |
60.7 |
|||
Times of PNC follow up |
<3 times |
132 |
86.8 |
|
|
Counselled about ENC during PNC follow up |
Yes |
118 |
77.6 |
|
|
No |
34 |
22.4 |
|
||
Area of counselling during PNC follow up |
Breast feeding |
76 |
64.4 |
|
|
Cord care |
63 |
53.4 |
|
||
Thermal care |
58 |
49.1 |
|
||
Immunization |
56 |
47.4 |
|
||
Neonatal danger sign |
16 |
13.5 |
|
||
Table 4 Obstetric characteristics of the mothers in East Badewacho woreda, Hadiya Zone, Southern Ethiopia 2018 (n=387)
Practice of essential newborn care
From the study participant, 132(34.1%) of the mothers practice ENC and 255(65.9%) of the mothers not practice ENC (Figure 1). For cord care practices, 215(55.6%) of the mothers apply substance on the cord and only 31(14.4%) of the mothers applied the drug on the cord that ordered by health professionals. Regarding to thermal care of baby, 274(70.8%) of the respondents were practice skin to skin contact and 215(55.6%) of the mothers gave bathing after 24 hours.
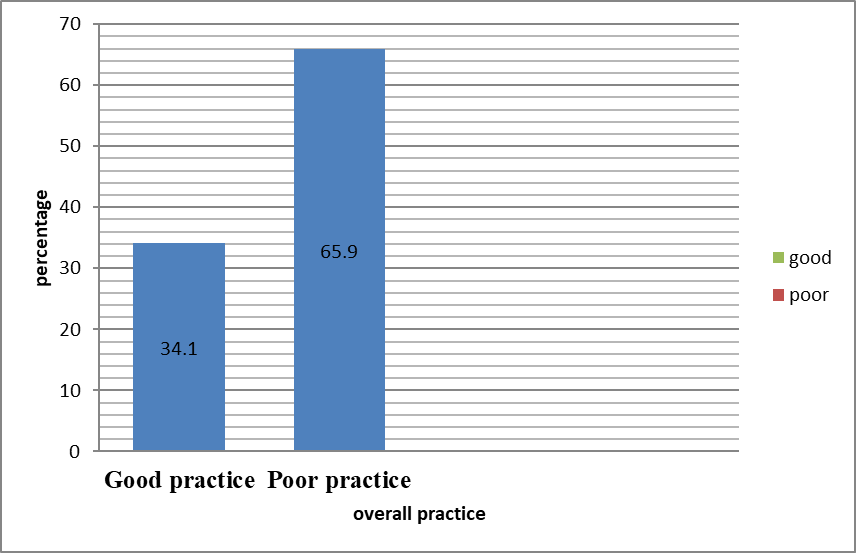
Figure 1 Over all essential newborn care practice among mothers in East Badewacho woreda, Hadiya zone, southern Ethiopia, 2018.
Breastfeeding within one hour was carried out by 209 (54%) and 281 (72.5%) of the mothers gave colostrum for their newborn. As far as immunization was concerned, 297(76.7%) of the respondents started immunization immediately after birth (Table 5).
Practice question |
Response |
Frequency |
% |
Instrument used to cut the cord at home |
New blade |
50 |
98 |
Instrument boiled before cutting of the cord at home |
Yes |
46 |
90.2 |
Materials used to tie the cord at home |
New &boiled thread |
41 |
80.4 |
Washing of hands before handling of the baby at home |
Yes |
27 |
52.9 |
Apply substance on the stump after the cord cut |
Yes |
215 |
55.6 |
Substances applied on the stump of the cord after cut |
Chlorohexidine |
31 |
14.4 |
Butter |
165 |
76.7 |
|
Vaseline |
18 |
8.3 |
|
putting of babies on the abdomen to encourage skin to skin contact |
Yes |
274 |
70.8 |
Covering of babies with cloth to encourage thermal care |
Yes |
338 |
87.3 |
Time of first bath given for newborn |
Immediately |
70 |
18 |
Within 24 hr |
102 |
26.4 |
|
After 24 hr |
215 |
55.6 |
|
Time of initiation of breast feeding |
Within 1 hr |
209 |
54 |
Giving of colostrum |
Feed the baby
|
281 |
72.6 |
What you feed the baby on first |
breast milk |
343 |
88.8 |
Started immunization |
Yes |
297 |
76.7 |
If the newborn has any manifestation of illness what did you do |
Take to health institution |
284 |
73.4 |
Give home Rx |
89 |
23 |
|
Take to traditional healer |
10 |
2.6 |
|
Do nothing |
4 |
1 |
Table 5 Utilization of ENC in East Badewacho woreda Hadiya Zone, Southern, Ethiopia 2018(n=387)
*cow’s milk, sugar with water, breast milk from other women
Factors associated with practice of essential newborn care
In multivariate logistic regression educational status of the husband, place of delivery and knowledge of the mother on ENC were significantly associated with utilization of ENC.
Educational status of the husband has significant predictors for practice of ENC. Husbands who complete primary levels were 86% more likely support practice of ENC compared with husbands educational level of not educated [AOR at 95%CI, 0.24(0.089, 0.64)], also husbands who complete secondary level were 68.6% more likely support practice of ENC when compared with husbands educational level of not educated [AOR at 95%CI, 0.314(0.126, 0.78)].
Place of delivery was significant relationship with practice of ENC. Mothers who gave birth at health institution were 97.6% more likely utilize ENC compared to mothers who had gave birth at home [AOR at 95%CI,0.024(0.009,0.068)]. Mother’s knowledge on ENC was significantly associated with practice of ENC. Mothers who had good knowledge on ENC were two times more likely practice ENC when compared with mothers who had poor knowledge on ENC [AOR at 95%CI,2.03(1.223,3.371)] (Table 6).
Variable |
Categories |
Practice of ENC |
COR at 95% CI |
AOR at 95% CI |
|
Good |
Poor |
||||
Educational of status husband |
Non educated |
14(48.3) |
15(51.7) |
1 |
0.24(0.089,0.64)a |
Place of delivery |
Health institution |
87(25.6) |
249(74.4) |
0.047(0.019,0113) |
0.024(0.009,0.068)c |
Knowledge on ENC |
Good |
57(39.3) |
88(60.7) |
1.442(0.938,2.218) |
2.03(1.223,3.371)d |
Table 6 Factors associated with utilization of ENC on multivariate logistic regression in East Badewacho woreda, Hadiya Zone, Southern, Ethiopia 2018
Key: 1=reference, a, b, c, d=significant, p-value<0.05; a=0.005, b=0.013, c=0.001, d=0.001
In this study essential newborn care practice and associated factors were analysed. The study showed that the prevalence of ENC practice was 34.1%. This result is higher than studies conducted in Ghana (15.8%),17 Eastern Uganda (11.7%),18 Aksum, Ethiopia (26.7%)10 and East Gojjam, Ethiopia (23.1%).13 This discrepancy might be due to an increased awareness of maternal health services and great intervention focusing on child health. But lower than the study done in South west Ethiopia (59.5%)11 and Northwest Ethiopia Mandura district (40.6%).19 This disparity might be due to socio-cultural difference between study areas and access to health facility.
In this finding, husbands who complete primary level 86% and secondary level 68.6% were more likely support practice of ENC compared with husband’s educational level of not educated. This result was consistent with study conducted in Bangladesh.20 The reason might be educated husband acquire knowledge through their academic life and play a key role in providing information about ENC practice at home.
The finding of this study showed that mothers who gave birth at health institution were 97.6% more likely practice ENC compared to mothers who had gave birth at home. This finding was in line with study done in India21 and Uganda.22 This could be mothers who gave birth at health institution have counselled about ENC; which increase knowledge of the mother concerning the essential newborn care practice.
The study showed that mothers who had good knowledge on ENC were two times more likely practice ENC compared to mothers who had poor knowledge on ENC. This finding was supported by studies conducted in Western Uganda23 and Ethiopia.15 This might be due to having mothers knowledgeable on ENC makes them more likely to utilize essential newborn care.
The study result revealed that practice of essential newborn care in East Badewacho Woreda was low. Husbands’ educational level, place of delivery and knowledge on ENC were statistically significant association with utilization of mothers on essential newborn care. Therefore, promote strong community based behavior change communication on the importance of ENC utilization to change the poor ENC utilization in the study area. Also, enhance linkage of health centers with health posts to increase ANC, institutional delivery and PNC service utilization.
First of all I would like to thank Jimma University School of Nursing and Midwifery for providing me the opportunity to carry out this study. I would like to thank East Badewacho woreda health office, health extension workers, kebele leaders, study participants, supervisors and data collectors for their cooperation.
The authors declare that they have no competing interests.

©2021 Thomas, et al. This is an open access article distributed under the terms of the, which permits unrestricted use, distribution, and build upon your work non-commercially.