Journal of
eISSN: 2373-4426


Case Report Volume 8 Issue 4
Department of Pediatrics, Jeju National University School of Medicine, South Korea
Correspondence: Yun Ju Lim, MD. Department of Pediatrics, Jeju National University School of Medicine, Aran 13 gil 15, Jeju-si, 23241, Korea, Fax 82 64 717 1656
Received: April 22, 2018 | Published: July 17, 2018
Citation: Lim YJ. Management of intractable supraventricular tachycardia unresponsive to primary therapy with Verapamil in a neonatal case. J Pediatr Neonatal Care. 2018;8(4):165-167. DOI: 10.15406/jpnc.2018.08.00331
We present a case of intractable Supraventricular tachycardia managed with intravenous Verapamil in a newborn with successful cardio version, followed by complication with reversible hypo perfusion. The electrocardiogram of our case confirmed that the Supraventricular tachycardia did not respond to multiple adenosine injections and direct-current electrical cardio version as first-line therapy. Although amiodarone infusion two times with the loading dose, followed by a maintenance dose was administered, the Supraventricular tachycardia never changed, displaying a rapid heart rate of 240 per minute. Two Verapamil injections caused a transient decline of the Supraventricular tachycardia to sinus tachycardia with an abrupt return to Supraventricular tachycardia. The third injection of intravenous Verapamil at a higher dose succeeded to change the sinus rhythm, but the patient collapsed with apnea and bradycardia with a heart rate of 87 per minute. Intubation with intravenous injection of calcium was promptly performed, and the patient regained hemodynamic stability without delay. We report intractable Supraventricular tachycardia converted successfully to a normal sinus rhythm in a neonatal case, although the use of this drug was controversial with fear and little experience for neonates. Verapamil was considered an effective therapy for refractory tachycardia in neonatal cases with a life-threatening risk. In addition, we recommend the careful monitoring of its dose and preparation with intravenous calcium to manage the circulatory crisis in our case.
Keywords: intractable supraventricular tachycardia, neonatal supraventricular tachycardia, neonatal tachyarrhythmia, verapamil infant therapy
Supraventricular tachycardia (SVT) is the most common arrhythmia in children, and 40% of cases arise during the first year of life. The incidence of neonatal SVT has been estimated to be 1 of 15,000–25,000 live births.1 SVT arises from atrioventricular nodal reentrant tachycardia, atrioventricular reciprocating tachycardia, and atrial tachycardia. Most tachycardias are revealed by signs of shock and heart failure such as pallor, poor feeding, hypotension, and tachypnea.2 The prognosis of SVT is usually good, but mortality rates of 2–10% have been reported as a medical emergency.3 Chronic tachycardias can lead to dilated cardiomyopathy.4 Vagal maneuvers and adenosine are an appropriate first treatment in patients with hemodynamically stable SVT, although circulatory collapse with tachycardias needs synchronized direct-current cardio version during acute episodes.2 For infants in whom cardio version is difficult or who have recurrent or intractable SVT, a more powerful anti arrhythmic drug such as digoxin, sotalol, flecainide, or amiodarone, is needed with intensive monitoring. Radiofrequency ablation could be attempted when the infant is approximately 15 kg, although the long-term potential for coronary artery stenosis exists in young cases.4–6 Verapamil is a class IV anti arrhythmic agent that acts as a selective inhibitor of myocardial calcium channels. It is used for the acute termination of SVT when first therapeutic options fail with a strong effectiveness in over 90% of children, although it is unlikely to be indicated in infants due to the risk for circulatory hypo perfusion2,4,7 Many articles have recommended Verapamil for infants as a second-line agent for unresponsive-to-first-line therapies for SVT.8–10 Here, we report a case of an intractable Supraventricular tachycardia successfully managed with intravenous Verapamil in a newborn unresponsive to multiple first-line therapies. In addition, we suggest that Verapamil is the most effective anti arrhythmic drug against refractory SVT and requires caution for neonatal cases due to the risk for circulatory collapse.
A 3-week-old male newborn with tachycardia was referred to the neonatal intensive care unit at Jeju National University Hospital (Jeju-do, South Korea). He was born with a birth weight of 3.5kg at 37 weeks of gestation via spontaneous vaginal delivery. His mother had no history of medication during pregnancy. There was no perinatal history of fetal arrhythmia or fetal hydrops. At admission, the initial heart rate was 250 beats per minute, and the blood pressure was within the normal range at 86/51mmHg with a body temperature of 36.3°C. He had mild chest retraction with tachypnea at a respiratory rate of 70 beats per minute and pulse oximetry saturation at 94% in room air. On chest X-ray, there was no active lung lesion without cardiomegaly. Two-dimensional echocardiography showed no congenital structural disease. A 12-lead electrocardiogram demonstrated the Supraventricular tachycardia with a narrow QRS (Figure 1). Three intravenous injections of adenosine (0.1,0.2,0.3mg/kg) changed the state to transient bradycardia with rapid recovery of supra ventricular tachycardia (Figure 2). In addition, we performed direct-current electrical cardio version (0.5–1J/kg) and intravenous amiodarone infusion two times with the loading dose (each 5mg/kg), followed by a maintenance dose, that could not convert the state to a normal sinus rhythm; thus, Supraventricular tachycardia had persisted. On the following day, Verapamil (0.075mg/kg) was slowly administered intravenously over 4 min with a transient decline of the heart rate to 170 beats per minute, but Supraventricular tachycardia returned with a rapid heart rate increase to 230 beats per minute. A second dose of Verapamil (0.15mg/kg) with a 20 min interval time was administered without a response.
We attempted a third injection of Verapamil (0.25mg/kg) greater than the recommended schedule within the maximal total dosage limitation with a 20 min interval time. After a third injection of Verapamil, the Supraventricular tachycardia was slowly terminated with a heart rate decline to 178 beats per minute with a normal sinus rhythm (Figure 3A). However, 20 min later, the patient appeared lethargic with apnea and bradycardia with a heart rate of 87 beats per minute (Figure 3B). We immediately performed intubation with an oxygen supply, and administered intravenous calcium already prepared at his bedside that resulted in recovery to a hemodynamic stability with the normal sinus rhythm (Figure 4). Serial venous blood gas analyses revealed the following: initially, at pH 7.0, pCO2 78 mmHg, pO2 53 mmHg and HCO3 17.5 mM per liter; subsequently, at pH 7.35, pCO2 43 mmHg, pO2 47 mmHg and HCO3 23.9 mM per liter at FiO2 0.3. On chest X-ray after treatment, pulmonary congestion with mild cardiomegaly was revealed. After Verapamil therapy, his electrocardiogram mostly appeared as a normal sinus rhythm, and intermittent Supraventricular tachycardia recurred with clearly effective termination by adenosine injection. In addition, an intermittent recurrence of Supraventricular tachycardia was treated with oral amiodarone and oral propranolol. He exhibited no adverse effects with maintenance of oral amiodarone.
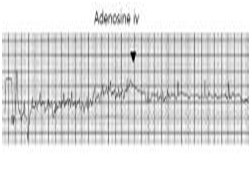
Figure 2 An intravenous injection of adenosine (black triangle arrow) led to transient bradycardia with abrupt recovery to supraventricular tachycardia.
Supraventricular tachycardia is the most common arrhythmia in newborns and infants requiring rapid conversion as a medical emergency. Its incidence in the neonatal period was 1 out of 15,000-25,000 live births and predisposing condition including congenital heart disease is found in 15% of cases.11 Most SVT affects structurally normal hearts and is caused by re-entrant tachycardia with accessory pathway. These episodes of SVT in neonates are benign and usually well tolerated; however, in some cases, they cause hemodynamic instability and circulatory shock with mortality by heart failure signs Chronic tachycardia causes a secondary dilated cardiomyopathy.1,3,8 The diagnosis is easy when the heart rate is>220 beats per minute with a narrow QRS<0.08 s on an electrocardiogram. SVT is caused by one of three mechanisms as reentry, increased automaticity, or triggered activity.2 Most SVTs are caused by atrioventricular re-entry with an accessory pathway and appear persistently in resistant neonatal cases. Sustained tachyarrhythmia in infants requires multi-drug combination therapy such as propranolol and amiodarone with catheter ablation.11 SVT management depends on many factors including age, the hemodynamic condition of the patient, coexisting heart disease, and recurrence.8 During an acute episode, adenosine is the drug of first choice in any tachycardias with advantages including a short half-life and minimal negative inotropic effects.12 Unstable critical patients with SVT need direct-current electrical cardio version emergently.
Usually, in SVT sensitive to adenosine, a beta-blocker is recommended. For infants in whom cardio version is difficult and with recurrent episodes of SVT, they need stronger anti arrhythmic drugs such as sotalol, flecainide, or amiodarone alone or in combination with a beta-blocker.4,5,11 In addition, digoxin is usually used as a classic drug for tachycardia within limitations. Furthermore, it is not used in the presence of a delta wave, and its slow onset time of 10 h is distressingly long in intolerable patients who may require other anti arrhythmic drugs with combined adverse effects.13 In the acute and chronic management of SVT, digoxin remained a frequent choice, although its efficacy as chronic therapy has been questioned.8 Intravenous Verapamil is a useful drug to treat SVT in older children and adults because of its rapid action and quick elimination, but it is contraindicated in infants and patients of any age receiving beta-blocker agents, with a high degree of atrioventricular block, and significant hemodynamic compromise of severe heart failure.5 Previous reports have warned against complications of verapamil in infants.3,12 Radford reported two infants with adverse effects of Verapamil. Two infants aged 3 weeks and 6 weeks developed life-threatening bradycardia and hypotension with near cardiac arrest as first-line therapy for SVT. Many reports of Verapamil treatment in infants have documented an anti arrhythmic effect with explanations of the complications.3,9,10 After Verapamil injection, SVT was terminated, but recurrent episodes were controlled by additional digoxin and electrical cardio version.10 In another report, Soler et al.,13 reviewed 29 infants with SVT who were treated with Verapamil (ages 5 days to 18 months).13 Before Verapamil was administered, SVT had developed 15 min to 5 days prior, particularly in 18 cases with heart failure. In 28 of 29 infants with SVT, a stable sinus rhythm was obtained with a dramatic effect of Verapamil. Only one case was terminated by a precordial blow after Verapamil injection of a higher dose, although the same maneuver before the injection of Verapamil was ineffective against SVT. Thus, Verapamil may be an effective drug for the treatment of SVT in infants without underlying heart disease due to high effectiveness, rapid action, and lack of undesirable side effects. In addition, it may be necessary to administer a higher dose. Furthermore, in our case, a higher dose of Verapamil had terminated a sustained SVT unresponsive to the first-line therapy of adenosine, electrical cardio version, and intravenous amiodarone. After Verapamil therapy, intermittent recurrent episodes of SVT were terminated rapidly by adenosine injection and oral amiodarone with a difference in the unresponsiveness for all of therapies before using Verapamil.
We agree that neonate administered intravenous Verapamil might be susceptible to the complications of severe hypotension, near cardiac arrest and heart block related to over-dosage instead of a definite conversion to the sinus rhythm in our case. We should finally use a third injection of dose-up Verapamil for its effectiveness. Although rapid conversion occurred within 20 min after Verapamil was injected, our case also needed additional therapy and intravenous calcium for the reversal of hemodynamic collapse due to its adverse effect. Roguin et al.,3 suggested that intravenous calcium gluconate prior to the use of Verapamil was helpful to avoid the negative inotropic effects of Verapamil.3 The authors reported that one case had serious side effects of Verapamil and another case with calcium injection prior to Verapamil therapy prevented the negative effects of PSVT. Our case was a rare newborn with refractory SVT unresponsive to multiple primary standard therapies, so we choose initially a Verapamil instead of a digoxin and a beta-blocker. We had to choose a more effective next therapy because longer delayed termination for SVT could increase the risk of circulatory failure, if it also would be failed. Finally, we suggest that Verapamil is a useful anti arrhythmic drug for terminating sustained refractory SVT and requires caution to avoid circulatory collapse risk in neonatal cases without underlying heart disease. Our case had limitations for over-dosage of Verapamil with efficacy of terminating SVT. Also, additional anti arrhythmic drug of amiodarone and propranolol had been needed for treatment of recurrent episodes although sustained tachycardia was terminated by Verapamil. More studies are needed to establish its efficacy and safe dosage of Verapamil to prevent the undesirable adverse effects associated with using a Verapamil in pediatric and neonatal SVT.
None.
Author declares that there is no conflict of interest.

©2018 Lim. This is an open access article distributed under the terms of the, which permits unrestricted use, distribution, and build upon your work non-commercially.
 World Down Syndrome Day is observed on 21 March 2026 to raise awareness about Down syndrome and to
promote inclusion, early intervention, and quality healthcare for children with genetic conditions. This day highlights the importance
of pediatric monitoring, developmental support, and continued research to improve health outcomes and overall well-being.
Researchers, pediatricians, and healthcare professionals are invited to submit their original research articles, reviews, and clinical
studies related to Down syndrome, neonatal screening, developmental pediatrics, and child health. Manuscripts submitted on the occasion
of World Down Syndrome Day will be eligible for a special publication discount of 30–40% in the Journal of Pediatrics & Neonatal Care (JPNC).
World Down Syndrome Day is observed on 21 March 2026 to raise awareness about Down syndrome and to
promote inclusion, early intervention, and quality healthcare for children with genetic conditions. This day highlights the importance
of pediatric monitoring, developmental support, and continued research to improve health outcomes and overall well-being.
Researchers, pediatricians, and healthcare professionals are invited to submit their original research articles, reviews, and clinical
studies related to Down syndrome, neonatal screening, developmental pediatrics, and child health. Manuscripts submitted on the occasion
of World Down Syndrome Day will be eligible for a special publication discount of 30–40% in the Journal of Pediatrics & Neonatal Care (JPNC).