Journal of
eISSN: 2373-4426


Research Article Volume 8 Issue 2
1Consultant Neonatologist & Head of Pediatric Department, Neonatal Intensive Care Unit, Pediatric Department, Latifa Hospital, Dubai Health Authority, UAE
2Consultant Neonatologist, Neonatal Intensive Care Unit, Pediatric Department, Latifa Hospital, Dubai Health Authority, UAE
3Specialist Registrar, Neonatal Intensive Care Unit, Pediatric Department, Latifa Hospital, Dubai Health Authority, UAE
Correspondence: Khaled El-Atawi, Consultant Neonatologist, Neonatal Intensive Care, Pediatric Department, Latifa Hospital, Dubai Health Authority, UAE
Received: December 25, 2017 | Published: March 13, 2018
Citation: Elhalik M, Habibullah J, El-Atawi K, et al. Epidemiology of sepsis in NICU; A 12 years study from Dubai, U.A.E. J Pediatr Neonatal Care. 2018;8(2):84–88. DOI: 10.15406/jpnc.2018.08.00315
In a retrospective analytic study from NICU, Latifa Woman and Children Hospital - Dubai, UAE. over a period of 12 years (2005 to 2016), 380 neonates and infants had clinical signs of sepsis, confirmed by blood or CSF culture. In very early onset sepsis (< 24 hours), E. Coli represented as the most common organism. In infants with early onset sepsis (2-6 days), Klebsiella Pneumoniae was the most common organism. While in late (7-28 days) & very late onset (29-90 days) the most common organism was Coagulase Negative Staphylococci (CONS) followed by Klebsiella Pneumoniae.
Keywords: Neonate, Sepsis, Meningitis
Sepsis remains one of the most common diseases of the neonatal period and is still a significant cause of morbidity and mortality. It contributes to 30-50% of all deaths during the neonatal period in developing countries.1 Sepsis related mortality is, however, largely preventable with rational antimicrobial therapy and aggressive supportive care. Use of intra partum antimicrobial prophylaxis has dramatically decreased the early onset of Group B streptococcal (GBS) infection, but it remains one of the most common causes of neonatal mortality and morbidity in preterm population. Late onset sepsis (LOS) occurs at 7-90 days of life and 80% acquired from caregivers and environment. Trends in late onset sepsis shows an increase in CONS as the causative organism, majority being sensitive to Glycopeptides and Aminoglycosides.2 The last few decades have experienced a trend towards changing pattern of organisms causing neonatal septicaemia. Additionally, variation in different geographical areas, calls for more research in this field. The objective of this study is to determine the incidence, microbiological pattern and clinical outcome of neonatal sepsis at the Neonatal Intensive Care Unit (NICU) of Latifa Woman & Children Hospital (LWCH)-Dubai, UAE.
Patient and method
This study retrospective analysis of culture verified cases of sepsis and meningitis in infants aged 0 - 90 days admitted to NICU of LWCH, which is a level III & tertiary care centre over a period of 12 years (First of January 2005 till end of December 2016). Sepsis is defined as a clinical syndrome characterized by systemic signs of infection accompanied by bacteremia in the first 90 days of life. Perinatal risk factors such as maternal fever, chorioamnionitis, GBS carrier mothers and rupture of membranes >18 hours were the reasons to obtain blood culture at birth. Clinical findings such as temperature instability, lethargy, apnea, poor feeding, tachypnea, cyanosis, vomiting, diarrhea and abdominal distention were considered clinically significant. Laboratory investigations other than positive blood culture & serology included, radiology, abnormal leukocyte count (> 30000 cells/μl or <5000 cells/μl and C-reactive protein >10 mg/dl. Infants were classified into ‘very early’ (≤ 24 h), ‘early’ (2-6 days), and ‘late’ (7-28 days) and ‘very late’ onset (29-90 days) based on postnatal age at onset of sepsis. Infants were further, divided into different birth weight groups, (450 to 1000 grams, 1001 to 1500 grams, 1501 to 2500 grams, and more than 2500 grams). Additionally, infants were also subdivided into two groups based on whether the infant was born in our hospital (inborn) or in another hospital (out born) and transported for further management and treated for sepsis in our hospital.
Laboratory methods
Blood culture: 1 or 2 ml of blood by venipuncture was inoculated directly in two blood culture bottles containing tryptisoya and thioglucolate growth media. The bottles were loaded into BactAlert / Bacteer for five to seven days. The presence of a positive culture was indicated by an audible alarm produced by blood culture system. Subculture was performed on day 1,2,3,&7 of incubation on blood agar and MacConkey’s media. Cerebrospinal fluid (CSF) bacterial cultures were plated from centrifuged deposits of CSF on the blood agar, chocolate agar, and MacConkey’s media. More than one culture in the same infant, which grew the same organism with the same antibiotics susceptibility, was considered as a single case. Mortality was considered related to the infection if it occurred within 7 days of the positive blood culture. Two positive blood cultures with CONS was required for the clinical diagnosis of sepsis in preterm neonates.
Statistical analysis
A standard structured data collection form was designed to obtain the following data; gestation age, birth weight, gender, age at the onset of clinical signs and symptoms of sepsis, causative organisms and related mortality. The incidence of sepsis was estimated by dividing the number of inborn infants with sepsis by 1000 live births. The case fatality rate was estimated by dividing the number of deaths from sepsis by the total number of sepsis cases. Statistical analysis was performed in SPSS 21.0. Frequency and percentage were used to describe the data. Chi-square test was used to assess the associations between different factors related to sepsis. Multiple logistic regression models was used to find the predictors of outcome of sepsis. Significance level was set at p value < 0.05. The Dubai scientific research ethics committee of Dubai Health Authority approved this study.
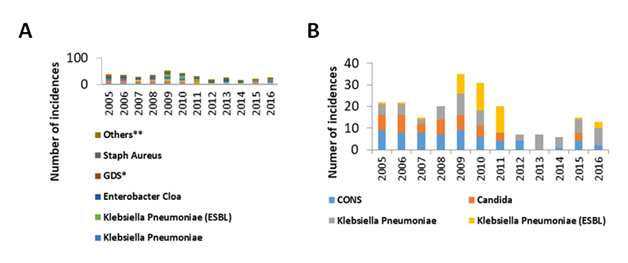
During the study period, from January 2005 until December 2016, there were 76674 live births of which 9684 were admitted to NICU of Latifa Women & Children hospital. Of them, 380 infants had culture verified septicemia and /or meningitis. Seventeen infants were positive for both blood and CSF culture while 363 were positive for only blood culture. The sex distribution was 210 male and 170 females. Of the total, 349 patients were inborn while 26 were transported out born. The characteristics of the infants with proven sepsis, incidence of neonatal sepsis and/or meningitis was 2.4/1000 live birth in infants from 0 to 28 days and 4.5/1000 live birth in infants from 0 to 90 days is shown in Table 1. In this study, Gram-ve bacteria (47.9%) was isolated more frequently than Gram+ve (39.7%) and fungi (12.4%) (χ2 = 78.953, df =2, p < 0.001, Figure 1A). The Commonly isolated organisms based to their prevalence was Klebsiella Pneumoniae (n=64, 16.8%) followed by CONS (n=62, 16.3%), Candida (n=42, 12.1%), Klebsiella Pneumoniae (ESBL) (n=41, 10.7%) and S. Aureus (n=35, 9.2 %) (χ2=88.311, df=10, p <0.001, Figure 1B). Yearly analysis showed that most of the organisms were evenly distributed, except for Candida, Klebsiella Pneumoniae (ESBL) and CONS (Figure 2A). After year 2012, a decrease in sepsis cases caused by Candida, Klebsiella Pneumoniae (ESBL) and CONS was observed. Organisms that were very frequently isolated in septic infants from 2005 until 2016 were CONS, Candida, Klebsiella Pneumoniae (ESBL and non-ESBL) (Figure 2B).
Characteristics |
|
Live births in Latifa Hospital |
76674 |
NICU admissions |
9684 |
Total number of cases |
380 |
Male/Female ratio |
210:170 |
Inborn |
349 |
Transported |
31 |
Incidences of sepsis/1000 live births |
|
0-28 days |
181(2.4%) |
0-90 days |
349 (4.5%) |
Number of cases with meningitis |
17 |
Incidence of meningitis /1000 Live births |
0.22% |
Mean Gestational age (weeks) |
32 (SD±12) |
Mean birth weight (G) |
978 (SD±512) |
Mean age of presentation (days) |
45.5 (SD±63) |
Overall mortality |
66/380 (17.3%) |
Table 1 Characteristics of neonates with proven sepsis (Jan. 2005 - Dec.2016)
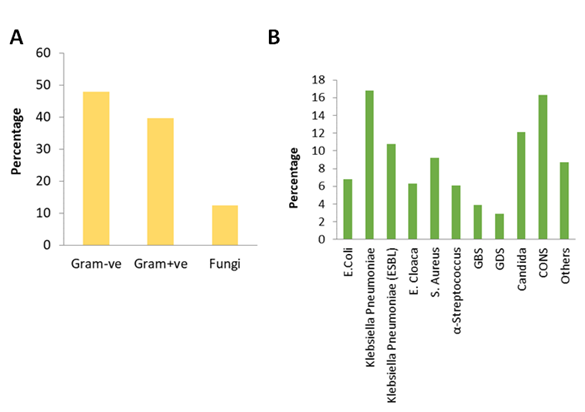
Figure 1 Causative organisms of sepsis in infants and neonates. (A) Percentage of Gram-ve bacteria was higher in the isolates followed by Gram+ve and Fungi (p<0.001). (B) Klebsiella Pneumoniae (16.8%) and CONS (16.3%) were the main causative organisms for sepsis in infants from 2005 until 2016. Candida infection (12.1%) followed by Klebsiella Pneumoniae (ESBL) (10.8%) and S. Aureus (9.2%) were the less frequent causes for sepsis in the infants during the study period (p<0.001).
Gram-ve organisms were the main cause of sepsis in infants<1500g, while Gram+ve organisms frequently caused sepsis in infants>1500g. Sepsis due to fungal infection was present in a minor proportion of low birth weight infants (χ2=33.920, df=6, p<0.001, Figure 3A). In infants with birth weight <1000g, organisms of 10 different genus were detected (Figure 3B). Organisms with a higher prevalence were CONS (20.4%), Candida (16.2%), Klebsiella Pneumoniae (15.8%), Klebsiella Pneumoniae (ESBL) (10.9%) and Group D Streptococcus (GDS) (10.9%). With increase in birth weight, the number of organisms infecting infants decreases. In infants with birth weight between 1000g to 1500g, 7 organisms of different genus were detected; Klebsiella Pneumoniae (31.1%), S. Aureus (20%), E. Coli (17.8%), and Klebsiella Pneumoniae (ESBL) (15.6%). In weight group 1500-2000g, 6 different genus were detected, predominantly, S. Aureus (36.1%), and GBS (22.2%). Similarly, in birth weight >2000g, organisms of only 3 different genus were detected; S. Aureus (53.3%), GBS (33.3%), and E. Coli (13.3%) (χ2=241.824, df=30, p< 0.001, Figure 3B). In this study, the percentage of late and very late onset of sepsis was very high as compared to very early and early onset of sepsis (χ2 =271.2, df =3, p < 0.001). Age at onset of sepsis was significantly associated with the causative organisms. When the sepsis was detected within first 24 hrs or 2 - 6 days after birth, Gram-ve organisms were found to be the dominant. Gram+ve organisms were the main causative agents for sepsis in infants with late (7–28 days) or very late (29 - 90 days). Interestingly, no fungal infection was observed in early onset groups. However, a minor proportion of fungi was detected in late onset group (χ2 =16.215, df =6, p< 0.05, Figure 4A). In very early onset group (<24 hrs), E. Coli (57.1%) was the dominant organism detected followed by GBS (21.4%) and Klebsiella Pneumoniae (14.3%) (Figure 4B). In early onset group (2-6 days) Klebsiella Pneumoniae (37.5%) was the major organisms followed by E. Coli (18.8%), Klebsiella Pneumoniae (ESBL) (12.5%), S. Aureus (12.5%) and GBS (12.5%). In late (7-28 days) and very late (29 -90 days) onset groups, many organisms were detected with predominant forms being CONS (19.0%) and Klebsiella Pneumoniae (18.7%) respectively (χ2 =122.235, df= 30, p< 0.001). Further, the birth weight of infants was inversely proportional to the time of onset of sepsis (Pearsons coefficient, r = -0.302, p< 0.001).
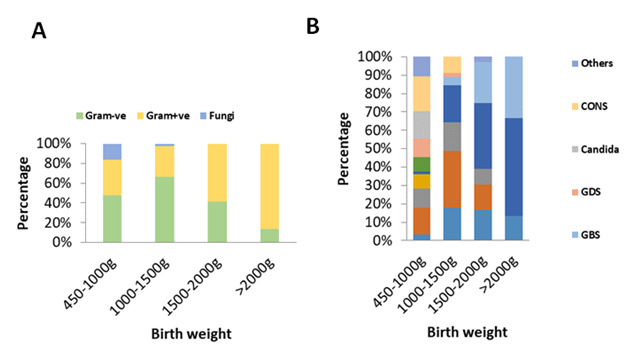
Figure 3 Distribution of organisms according to birth weight. Gram-ve bacteria mainly contributed to sepsis in preterm babies below 1500g weight while Gram+ve bacteria mainly caused sepsis in infants with birth weight >1500g (p<0.001) (B) CONS infection (20.4%) was the common cause of sepsis in preterm babies within 450-1000g of birth weight. Klebsiella Pneumoniae infection (31.10%) was the dominant cause for sepsis in preterm babies with birth weight 1000g-1500g while S. Aureus infection (36.10% vs. 53.3%)was the main cause of sepsis in preterm babies with birth weight 1500-2000g and >2000g respectively (p<0.001).
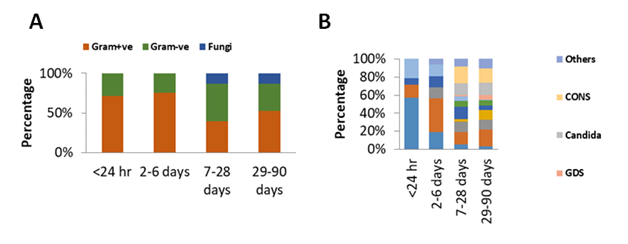
Figure 4 Distribution of organisms according to sepsis onset. (A) Gram-ve bacterias were mainly isolated in very early and early sepsis cases while Gram+ve bacterias were isolated mainly from late and very late sepsis cases. Fungal infection was also present in small percentages in late and very late sepsis cases (p<0.001). (B) E.Coli (57.1%) most frequently caused sepsis in neonates (< 24 hrs) while Klebsiella Pneumoniae (37.5%) predominantly caused sepsis in 2-6 days old neonates. In late (7-28 days old) and very late (29-90 days old) infants, multiple organisms were the cause of sepsis; the predominant forms were CONS (19.0%) and Klebsiella Pneumoniae (18.7%) respectively (p<0.001).
Meningitis was diagnosed in 17 infants with sepsis. Even though meningitis was increasingly observed in Gram-ve bacteria than Gram+ve and fungi, this difference was not statistically significant (χ2 =0.709, df=2, p=0.883). Infection with GBS accounted for 29.4% of meningitis followed Klebsiella Pneumoniae (23.5%), CONS (17.6%) and E. Coli (17.6%) (χ2=1.529, df=4, p=0.821). Considerably higher incidences of mortality were observed in Gram-ve bacteria (23.1%) than Gram+ve (11.9%) and fungi (12.8%) (χ=7.949, df=3, p<0.05, Figure 5A). Increasing number of deaths was associated with α-Streptococcus (26.1%), E. Cloacae (25%), Klebsiella Pneumoniae (20.3%), E. Coli(19.2%) and Candida (13.0%) (χ2=31.979, df=10, p< 0.001, Figure 5B). Moreover, a minor group of organisms denoted by “others” containing Pseudomonas Aeruginosa, Group C Streptococcus (GCS), Listeria Monocytogene, Serratia Marcescens and Sphingomonas Paucimobilis also accounted for increasing number of deaths (χ2=7.33, df=4, p=0.119). Furthermore, birth weight of infant was significantly associated with the number of deaths (χ=10.177, df=3, p<0.05, Figure 5C). The lower the birth weight the higher was the incidence of deaths due to sepsis. However, time of onset of sepsis was not significantly associated with the mortality of the infants (χ=0.211, df=3, p=0.976).
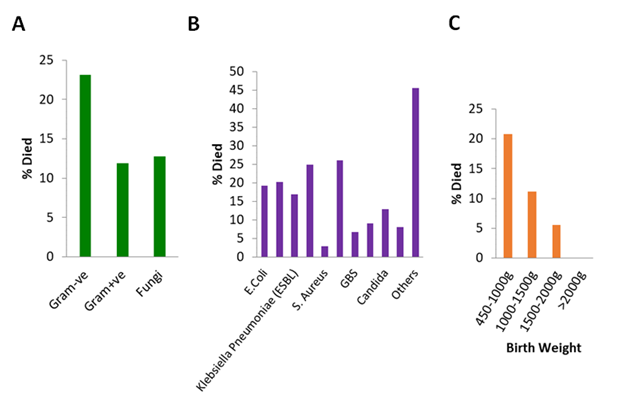
Figure 5 Death caused by different organisms. (A) Higher percentage of death was observed in Gram-ve bacteria as compared to Gram+ve and fungi (p<0.05). (B) Infection with α-Streptococcus (26.1%) and E. Cloacae (25.1%) caused highest number of deaths in septic infants when compared to other organisms (p<0.001). (C) Higher incidences of death was associated with birth weight group 450-1000g.
Advances in neonatal intensive care medicine and improved obstetrical management has led to improvement in the survival of extreme preterm babies. Although early onset neonatal sepsis is becoming less frequent because of intra partum prophylactic antibiotics for GBS carrier mothers, there is an increase rate of late onset sepsis.1–4 This report describes the risk factors of sepsis and the outcome of sepsis in neonates and infants of Dubai over a 12 years period. The pathogen pattern of neonatal sepsis has demonstrated change with time and relevant to different regions of the world. Many studies have been undertaken to identify the organisms and their changing patterns responsible for sepsis/meningitis in neonates and infants. A report of national neonatal Perinatal database (National neonatology forum) from India revealed the incidence of infantile sepsis as 30/1000 live births with Klebsiella Pneumoniae and S. Aureus being the most common organisms.5 Another report from India shows a higher overall sepsis rate (38/1000) live births as compared to developed countries.6 In US, overall neonatal sepsis affects approximately 1-5% of live birth with lower incidence (1-2/1000) in the term infants.7 Similarly, the sepsis rate in very low birth weight infants were 7 times higher in infants with birth weight ≥ 2500 g.8 Our present study reveals an overall incidence of neonatal and infantile sepsis of 2.4/1000 live births with the age of onset from 0-28 days and 4.5/1000 live births with age of onset from 0-90 days in very early onset and early onset of sepsis. Klebsiella Pneumoniae was the most common organism isolated followed by CONS, Candida, E. Coli, Klebsiella Pneumoniae (ESBL) and S. Aureus in late onset sepsis. After implementation of antimicrobial stewardship program, strict infection control measures and restriction of usage of 3rd generation cephalosporin and Glycopeptides in NICU, there has been a dramatic decrease in sepsis with multi-resistant organisms and Candida.9–11 Similarly, in our unit, after implementation of these guidelines since 2012 resulted in a sharp decline in Klebsiella Pneumoniae (ESBL), CONS and Candida was demonstrated. The incidence of early onset sepsis in developing countries is 0.9 to 1.5/1000 live births.
The most common cause of early onset sepsis was GBS (43-58%) followed by E. Coli (18-29%), S. Aureus (2-7%), CONS (1-5%), and Listeria (0.6 - 6%). Gram negative microorganism only contributed to one quarter of the early onset infantile sepsis.12 On the contrary, in developed countries like USA, the incidences of early onset sepsis varies from 9.6 to 17/1000 live births. Moreover, the Gram-ve bacteria was the prevalent cause of the sepsis.13 The incidence of early onset sepsis in our cohort was 2.4/1000 live births which was between those reported in developing and developed countries. Similar to developed countries, infection with Gram-ve bacteria predominantly caused sepsis in early onset group. E. Coli infection was frequently observed when sepsis onset was < 24 hrs of delivery while infection with Klebsiella Pneumoniae was majorly observed when onset of sepsis occurred 2 - 6 days after delivery. Increase in Gram-ve bacterial infection was reported by many studies after the use of intra partum antibiotics prophylaxis against GBS.3,4,14 In developing countries, late onset sepsis was frequently caused by both Gram-ve bacteria e.g. Klebsiella Pneumoniae (16-28%) and E. Coli (8-18 %) as well as Gram+ve bacteria by S. Aureus (13-26%) and CONS.14–18 The incidence of late onset of sepsis in developed countries such as UK was 3/1000 live births (7/1000 live birth including CONS).19 Contrary to the developing countries, in developed countries Gram+ve bacteria commonly caused late onset of sepsis which included primarily CONS (54%), Enterobacteriaceae (21%) and S. Aureus (18%), while fungus accounted for 9% of late onset sepsis.19 Our data on late onset of sepsis showed both Gram-ve (Klebsiella Pneumoniae) and Gram+ve (CONS) as well as fungal infection (Candida) as the major cause. However, the incidences due to these organisms were much lower in our study than those reported earlier.14–19 Very low birth weight (<1500g) as well as low birth weight (≤ 2500g), including preterm and term infants, has been reported to be associated with early onset sepsis which was mainly attributed to obstetrical complications.20 However, early onset of sepsis in low birth weight infants is decreasing due to increased intra partum antibiotic prophylaxis. Rather, the incidences of late onset of sepsis is increasing in this group. Early onsets of sepsis in low birth weight have the highest mortality rate.20 In our study, we found that mortality rate was highest in infants with birth weight < 1000g. Low birth weight infants are prone for sepsis with more than one organism, as compared to higher birth weight, indicating a role of impaired immune system in the low birth weight infants.21 Mortality was twofold higher in Gram-ve bacteria than in Gram+ve and fungi. Among Gram-ve bacteria, e.g. E. Coli, Klebsiella Pneumoniae, Enterobacter Cloacae, Pseudomonas Aeruginosa, Serratia Marcescens and Sphingomonas Paucimobilis are increasingly associated with mortality. In Gram+ve bacteria, α-Streptococcus contributed maximally to overall mortality while other Gram+ve bacteria such as S. Aureus, GBS, GDS, and CONS was associated with less mortality. Multiple regression analysis in our study showed that significant independent predictors of mortality were very low birth weight infant and Gram-ve bacterial sepsis. Other studies have also reported similar observations. An impaired immune system in low birth weight infants makes them more prone to acquire healthcare associated infections.21,22 Although, time of onset of sepsis has been shown by different studies to be an independent predictor of mortality in neonates and infants, it was not significantly associated with mortality in our cohort.
Sepsis in neonates and infants is the commonest cause of mortality and morbidity in this group. There is a trend of changing pattern of organisms responsible for neonatal sepsis based on antibiotics usage policy, time of onset and Perinatal risk factors. Neonatal mortality, morbidity and bacterial resistance can be reduced by early diagnosis, treatment, increased awareness of strict infection control practices and implementation of an antimicrobial stewardship program in the NICU.
None.
There is no conflict of interest.

©2018 Elhalik, et al. This is an open access article distributed under the terms of the, which permits unrestricted use, distribution, and build upon your work non-commercially.
 World Down Syndrome Day is observed on 21 March 2026 to raise awareness about Down syndrome and to
promote inclusion, early intervention, and quality healthcare for children with genetic conditions. This day highlights the importance
of pediatric monitoring, developmental support, and continued research to improve health outcomes and overall well-being.
Researchers, pediatricians, and healthcare professionals are invited to submit their original research articles, reviews, and clinical
studies related to Down syndrome, neonatal screening, developmental pediatrics, and child health. Manuscripts submitted on the occasion
of World Down Syndrome Day will be eligible for a special publication discount of 30–40% in the Journal of Pediatrics & Neonatal Care (JPNC).
World Down Syndrome Day is observed on 21 March 2026 to raise awareness about Down syndrome and to
promote inclusion, early intervention, and quality healthcare for children with genetic conditions. This day highlights the importance
of pediatric monitoring, developmental support, and continued research to improve health outcomes and overall well-being.
Researchers, pediatricians, and healthcare professionals are invited to submit their original research articles, reviews, and clinical
studies related to Down syndrome, neonatal screening, developmental pediatrics, and child health. Manuscripts submitted on the occasion
of World Down Syndrome Day will be eligible for a special publication discount of 30–40% in the Journal of Pediatrics & Neonatal Care (JPNC).