Journal of
eISSN: 2373-4426


Case Report Volume 5 Issue 1
Department of Pediatric Surgery, Maternity & Children's Hospital, Saudi Arabia
Correspondence: Rajendran Ramaswamy, Consultant in Pediatric Surgery, Department of Pediatric Surgery, Maternity & Children's Hospital (under Ministry of Health), PB no.3600, Najran, Saudi Arabia, Tel 966-536-427602, Fax 966-075-29391
Received: June 21, 2016 | Published: July 12, 2016
Citation: Ramaswamy R, Shawky M, Baz RA, Saeed S, Mukttash G (2016) Mischief of a Mini Magnet: Report of a Case and Review of Literature. J Pediatr Neonatal Care 5(1): 00166. DOI: 10.15406/jpnc.2016.05.00166
Accidental ingestion of foreign bodies is commonly seen in pediatric practice. A particularly dangerous situation is ingestion of magnetic foreign bodies. There are increasing reports of complications of multiple magnet ingestion by children.1-3 The spectrum of complications is possibly only unfolding. Increased awareness of the problems associated with magnet ingestion is necessary for parents, healthcare givers, toy makers and marketers. Life-threatening complication following ingestion of one magnet has not been reported in literature. A case of multiple bowel perforations due to ingestion of one magnet is presented and the literature is reviewed.
Fourteen months old boy was admitted at 3AM with excessive cry, fever, vomiting and constipation of 1day duration. There was no history of trauma or foreign body ingestion. There was no relevant past history. During morning-rounds, his temperature was 38.6 °C, he was grunting, and in severe abdominal pain. His FLACC pain score4 was 7 in a scale of 0-10. He was not pale or dehydrated. There was mild abdominal distension, generalised tenderness and rigidity. Digital rectal examination showed some mucus in rectum, and no pelvic mass. Bowel sounds were absent. Blood examination showed polymorphonuclear leukocytosis (WBC count=12.07x103, neutrophils=76.8%), hyponatremia (Na=129 mmol/dl, K=3.9mmol/dl), normal renal and liver function tests and serum amylase. Plain abdominal radiograph at the time of admission showed dilated oedematous bowel loops on left side. Many circular radioopaque shadows within and outside pelvis were considered as due to buttons of infant-diaper (Figure 1). Supine and upright abdominal radiographs done 8hours after admission showed minimal pneumoperitoneum Figure 2 (A&B). One opaque shadow noted within the pelvis in front of right sacroiliac joint was fairly constant in all the pictures with very little change in shape due to oblique position of child. USS of abdomen revealed dilated bowel loops with thickened, oedematous wall, very slow peristalsis mainly in left side, and minimal free fluid in hepatorenal region. Provisional diagnosis was perforation peritonitis due to? Magnetic foreign body in the gut.
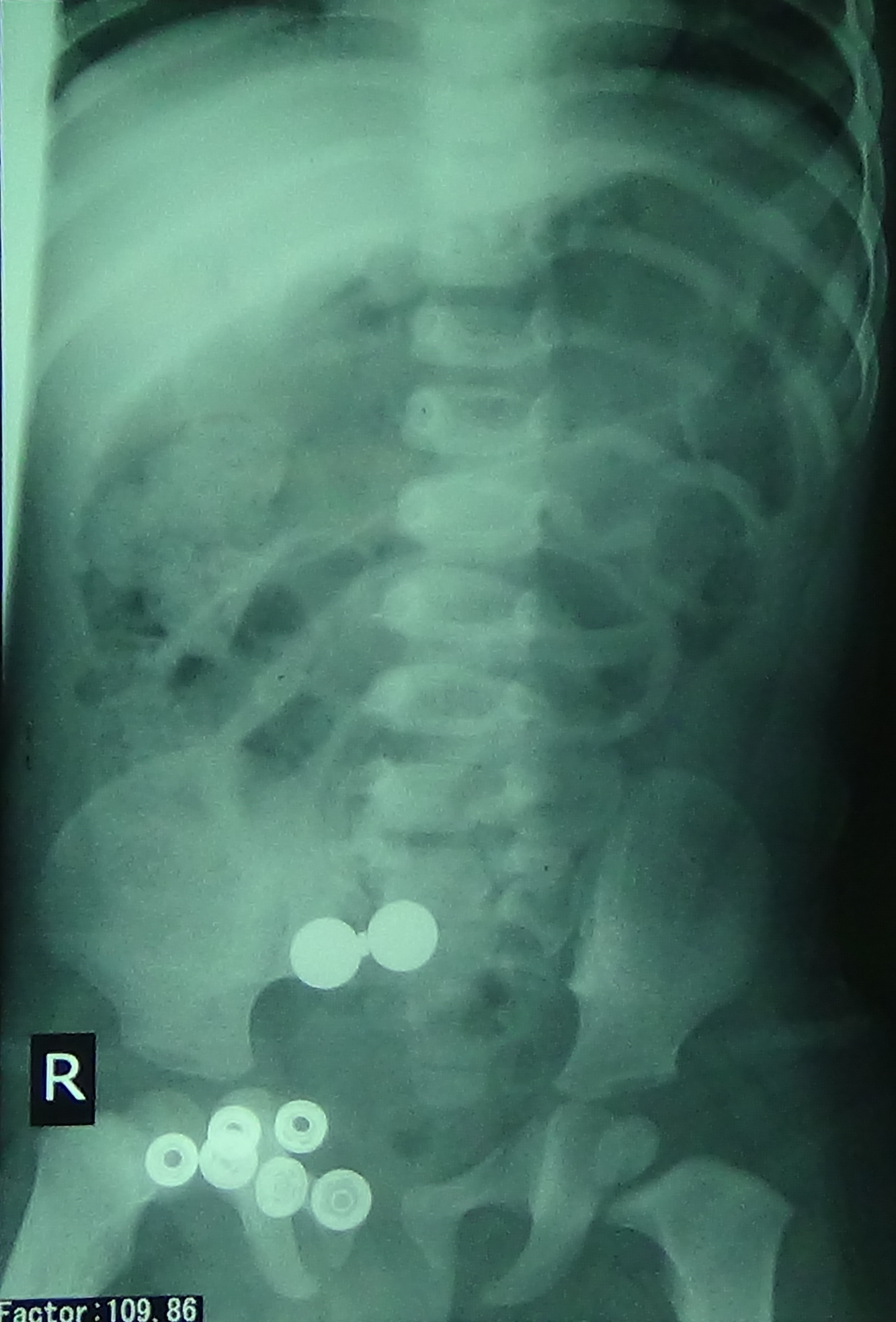
Figure 1 Abdominal radiograph showing oedematous bowel loops and multiple radioopaque shadows in and out of abdomen.

Figure 2A Supine abdominal radiograph showing a radioopaque shadow only at the level of sacrum, and dilated bowels in upper left quadrant.
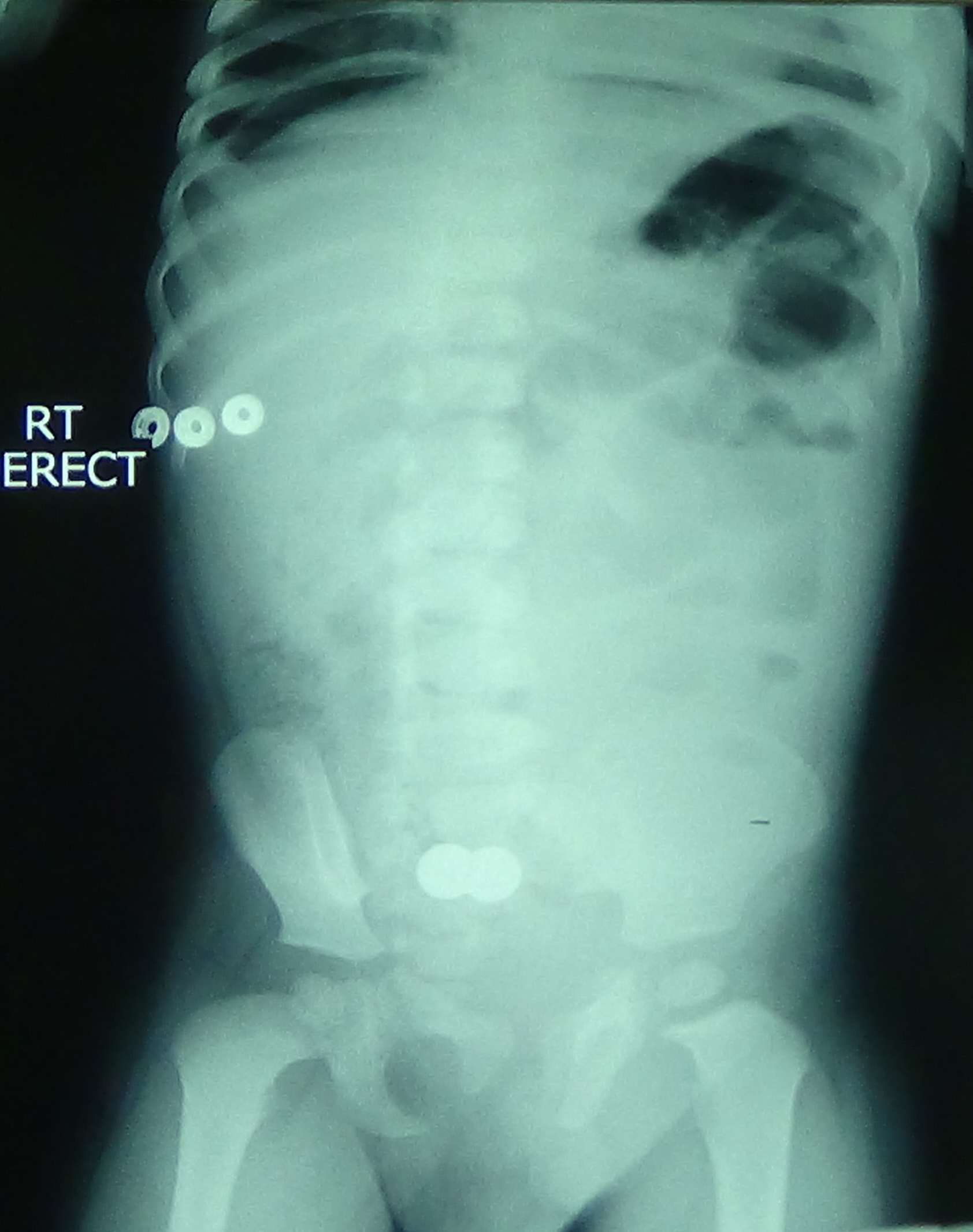
Figure 2B Erect abdominal radiograph showing free gas under diaphragm and a radioopaque shadow at the level of sacrum.
Emergency laparotomy showed plenty of purulent fluid due to general peritonitis. Two ileal perforations were detected. Each was about 10mm in diameter. One was in proximal ileum. A metal ball of 11mm diameter was removed from distal jejunum through the perforation. There was one necrotic patch of 5mm in diameter about 15cm distal to perforation (Figure 3). The second ileal perforation was about 45cm proximal to ileocaecal junction, followed by another necrotic patch of 5mm in diameter, about 15cm distal to perforation. A second metal ball of 11mm diameter, with an adherent metal disc (4mm diameter & 1mm thick) was removed from distal ileum through the distal ileal perforation (Figure 4). This metal disc was found to be a magnet. Margins of perforations were healthy. Vermiform appendix and colon were unaffected. Pus flakes were present in left lower abdomen. Thorough peritoneal toilet was done, margins of perforations were excised and closed in 2 layers. Necrotic patches were over sewn. Two peritoneal drains were put. Peritoneal swab culture showed E.coli. Oral fluid was started on 7th postoperative day, and slowly increased. On 12th postoperative day, he developed fever and subcutaneous abscess in the operation wound, which was let out. Abdominal USS was unremarkable. He was discharged cured on 16th day.
Retrospective analysis of the radio opaque shadow in front of right sacroiliac joint in all the x-ray pictures was done after operation. The position of that shadow was fairly constant. On magnification of that radio opaque shadow in Figure 1, a minute gap between the narrow central part and the circular right part was appreciable (Figure 5). This was suggestive of bowel between two magnetic foreign bodies.
Al-Salem studied 40 children with swallowed foreign bodies in Saudi Arabia, over a five-year period from April 1989 to March 1994. There was no magnetic foreign body in this series.5 Chung et al reported ingestion of multiple magnets causing ileo-ileal fistula.1 Since 2003, the Consumer Product Safety Commission (CPSC) of USA has identified one death, and 19 other cases of injuries requiring gastrointestinal surgery resulting from ingestion of small powerful rare-earth magnets in toy products.2 The 20 patients ranged in age from 10 months to 11 years, 6 months (mean: 5 years, 6 months); 16 (80%) of the patients were aged >3 years. Boys accounted for 16 (80%) of the patients. One fatality was caused by volvulus, bowel necrosis, and sepsis. Nineteen patients swallowed more than one magnet. Only one case was swallow of one magnet plus a metal disc, which caused superficial ulcers. Some children had autism, attention-deficit/hyperactivity disorder, developmental delays, and neurologic disorder.2,6 In 2010 Ahmed reported from Saudi Arabia, of 5 year old girl who ingested two magnets causing jejunocolic fistula.7 Strickland8 studied 94 patients of magnet ingestion below 18 years age between 2002-2012. The median age was 4.5 years and 65% were male. He concluded that the incidence of pediatric magnet ingestions increased from 2002 to 2003 from 0.57 cases per 100,000 children per year to a peak in 2010 to 2011 of 3.06 cases per 100,000 children per year. These injuries have increasingly involved multiple, smaller magnets and required operative intervention. Most ingested magnetic foreign bodies (73%) and multiple magnet ingestions (91%) occurred in 2007 or later. The volume of the magnets decreased from 878.6mm3 to 259.8mm3. Modern NIB (alloy of Neodymium, Iron and Boron) toy magnets are 10 times more powerful than traditional magnets capable of producing attractive forces up to 1300 G. Although small enough to pass through the digestive tract, they can attach to each other across intestinal walls. These erode through the intervening bowel wall resulting in perforation, internal enteric fistulae, internal herniation, adhesions, volvulus, obstruction, mesenteric hemorrhage and death. Enteric fistulae reported are jejunoileal, jejuno-caecal, jejuno-colic, ileo-ileal and duodenojejunal.6 The magnet in the present case was a very powerful miniature magnetic disc of 4mm diameter and 1mm thickness only, which stuck to two metal balls having three times its diameter across different bowel loops, eroding the intestinal walls to perforate, and crushing to cause necrotic patches with impending perforation.
The diagnosis of presence of magnetic foreign body within the abdomen is extremely difficult. History of the child having played with building sets and other toys containing magnets may be available. To aid in diagnosis, a compass might be passed close to the abdomen to determine whether an unidentified object in the bowel is magnetic.2 On radiologic examination, a health-care provider cannot ascertain whether objects swallowed are magnetic and whether they are in separate sections of the gastrointestinal tract with tissue between them.2 This was very true of our case also. Subtle separation or gaps within the radio opaque shadow suggest the presence of bowel wall between the objects. The absence of movement on follow-up radiographs should also raise the suspicion of magnetic objects apposed across bowel wall.3,9 Our patient had no developmental delay/behavioral disorder. The parents could not remember foreign body swallow by the child or source of such magnetic materials. The constant position of foreign body in radiographs taken eight hours apart, and the subtle gap within the radio opaque shadow (on retrospective examination) are pointers to the diagnosis of magnetic foreign bodies stuck together across bowel walls. MRI of the abdomen should never be used as it can precipitate a perforation.6
A review of treatment of magnetic foreign bodies recommends that with one magnet <5cm devoid of sharp edges without coexistence of other metallic objects and underlying intestinal illness, observation is indicated with the following precautions. Serial radiographs should be performed to confirm that the magnet progresses through the gastrointestinal tract and to confirm that multiple magnets are not present. Both AP and lateral radiographs should be performed initially, and all subsequent radiographs should be closely examined for any indication that multiple magnets might be present. The child should be kept away from any magnetic or metallic materials (including metallic buttons or buckles in clothing), until the magnet has passed out. Because even single magnet has some risk, endoscopic removal should be considered if the magnet is accessible. However, when more than one magnet is ingested, or a magnet along with another magnetic foreign body is ingested they should be removed with an endoscope. If they can’t be retrieved, emergency laparotomy, their removal and necessary repairs should be the performed.10,11 Magnetic probes have been used to retrieve magnetic and metallic foreign bodies with varying success. In the present case, the compelling reason for emergency laparotomy was perforation peritonitis, though we concluded the presence of a magnetic foreign body. Waters12 studied 99 magnet ingestions. Thirty-two children underwent endoscopy. Seventy-three children required either laparotomy (51) or laparoscopy (22) for magnet removal, and 90% of these children were discovered to have invested more than one magnet. The present case is unique from previous reports of peritonitis due to multiple magnet ingestion.1,3,13-15 The ingestion of magnetic foreign body was unwitnessed. There was only one miniature magnet. This and two bigger metal balls have caused multiple intestinal perforations. There were minute radiological evidences of magnetic foreign bodies preoperatively.
An infant boy presenting with perforation peritonitis and possible magnet in gut was found at operation, to have multiple bowel perforations due to a miniature magnet and 2 magnetic foreign bodies. This case is reported to alert the family physicians, pediatricians and pediatric surgeons of the hazards and radiological findings of magnetic foreign bodies in the gut. Public and healthcare workers need to be educated about the perils of magnet ingestion.
None.
None.

©2016 Ramaswamy, et al. This is an open access article distributed under the terms of the, which permits unrestricted use, distribution, and build upon your work non-commercially.
 World Down Syndrome Day is observed on 21 March 2026 to raise awareness about Down syndrome and to
promote inclusion, early intervention, and quality healthcare for children with genetic conditions. This day highlights the importance
of pediatric monitoring, developmental support, and continued research to improve health outcomes and overall well-being.
Researchers, pediatricians, and healthcare professionals are invited to submit their original research articles, reviews, and clinical
studies related to Down syndrome, neonatal screening, developmental pediatrics, and child health. Manuscripts submitted on the occasion
of World Down Syndrome Day will be eligible for a special publication discount of 30–40% in the Journal of Pediatrics & Neonatal Care (JPNC).
World Down Syndrome Day is observed on 21 March 2026 to raise awareness about Down syndrome and to
promote inclusion, early intervention, and quality healthcare for children with genetic conditions. This day highlights the importance
of pediatric monitoring, developmental support, and continued research to improve health outcomes and overall well-being.
Researchers, pediatricians, and healthcare professionals are invited to submit their original research articles, reviews, and clinical
studies related to Down syndrome, neonatal screening, developmental pediatrics, and child health. Manuscripts submitted on the occasion
of World Down Syndrome Day will be eligible for a special publication discount of 30–40% in the Journal of Pediatrics & Neonatal Care (JPNC).