Journal of
eISSN: 2373-4426


Case Report Volume 1 Issue 3
1Department of Cardiovascular, Respiratory, Nephrological, Anaesthesiological and Geriatric Sciences, Sapienza University of Rome, Italy
2Department of Pediatric Cardiology, Sapienza University of Rome, Italy
3DEA, Radiology, Sapienza University of Rome, Italy
4Department of Radiological Oncological and Anatomopathological Sciences, Umberto I Hospital, Sapienza University of Rome, Italy
Correspondence: Federica Caldaroni, Department of Cardiovascular, Respiratory, Nephrological, Anaesthesiological and Geriatric Sciences, Sapienza University of Rome, Italy; Viale del Policlinico, 155, 00161 Rome, Italy, Tel 391000000000
Received: June 13, 2014 | Published: July 5, 2014
Citation: Caldaroni F, Rose D, Caiaro A, Casciani E, Martucci V, et al. (2014) Fetal Right Ventricular Diverticulum with Pericardial Effusion: To Drain or Not To Drain? J Pediatr Neonatal Care 1(3): 00016. DOI: 10.15406/jpnc.2014.01.00016
Congenital right ventricular diverticulum is a rare form of congenital heart disease often associated with pericardial effusion or other cardiac malformations. The optimal management of this disease has not yet been established. Reviewing the literature, the most common approach is excision or pericardial effusion drainage during fetal or post-natal life, based on morphology and hemodynamic pattern of diverticulum. Pericardiocentesis is recommended for decompressing the fetal thorax, avoiding the risk of pulmonary hypoplasia and allowing lung maturation, but especially in fetal life, it carries a very high risk of abort or fetal damage. We report a case in which, considering the asymptomatic clinical setting and the stability of the hemodynamic conditions, the treatment successfully chosen was a long-term watchful waiting. Our experience confirmed that, in asymptomatic patients, conservative management may be a reasonable option as the pericardial effusion rounding the diverticulum may progressively disappear not requiring any therapeutic intervention.
Keywords: congenital right ventricular diverticulum, congenital aneurysm, fetal pericardial effusion, pericardiocentesis
CHD, heart disease; RVOs, right ventricular outpouchings; MRI, magnetic resonance imaging
Congenital right ventricular diverticulum is an extremely rare form of congenital heart disease (CHD), often associated with pericardial effusion, for which little information exists regarding optimal management, natural history, or prognosis.1 The first case in history was described in 1838 by O’Bryan.2 in a patient affected by Ectopia cordis. Right ventricular outpouches are less common than those arising from the left ventricle, but both can be associated with other cardiac malformations,3 the most common of which appears to be conotruncal malformations followed by isolated ventricular septal defects.4,5
In literature, since 1940, fewer than 200 cases of ventricular aneurysms or diverticula have been reported and only 20 of these involved the right ventricle.6 The exact incidence of these lesions, however, is not known because antenatal detection has been infrequent and many affected neonates are asymptomatic.3,6
It is often difficult to distinguish between right ventricular aneurysms and diverticula on the basis of morphological findings, as both are presenting as right ventricular outpouching. These two lesions are differentiated histologically by presence or absence of myocardium.1 The wall of a diverticulum in fact comprises all three histological layers of a normal cardiac wall: endocardium, myocardium and epicardium and, on echocardiography, right ventricular diverticula show a narrow connection to the ventricle and an active contraction during systole,1,7 due to the presence of viable and well-structured myocardiocytes in the wall, whereas right ventricular aneurysms show a wide connection to the ventricle and a paradoxically motion in systole, due to the presence of few disorganized muscle fibers. Occasionally, however ventricular outpouches can have pathologically elements of both.1,8 We can also make a morphologic distinction between apical and non-apical right ventricular outpouchings (RVOs).6,7
Non-apical right ventricular outpouchings appear to be a more heterogenous group of lesions than apical diverticula in terms of location, size, and clinical course. For reasons not understood, both lesions are associated with a large pericardial effusion and may have related atrial and ventricular septal defects.1 Some investigators have suggested that rubbing between ventricle and pericardium is the most probable cause of effusion.8 Pathogenesis of cardiac diverticula and aneurysms in fetal life is poorly understood. They may occur as a result of focal weakening of the ventricular wall due to an interruption during embryogenesis, infection or localized ischemia of the ventricular wall due to stenosis, hypoplasia or intimal proliferation of the coronary arteries. In some cases, abnormal development of the microvasculature, involving terminal branches of the coronary artery leading to early ischemic changes in the papillary muscle, has been suggested as the etiology.4 The isolated form can be discovered as a subsequent finding to arrhythmia, congestive cardiac failure, chest pain or tamponade due to acute rupture, and even sudden death but, in the majority of cases, congenital ventricular diverticula are silent, with a benign clinical course.1,3,7
A 29-year-old woman, gravida 3, para 2, smoker, was referred at 31weeks of gestation for the incidental finding of fetum pericardial effusion on a routine prenatal echography. The first ultrasound scan showed an 8 mm pericardial effusion, due to a right sided cardiac protrusion with a narrow neck, synchronous with cardiac pulse, compatible with a diverticulum. Color flow mapping showed bidirectional flow into and from the dilatation. In this first examination both lungs were compressed and showed pulmonary hypoplasia, probably due to pericardial effusion, but no structural fetal anomalies and no other structural or functional heart defects were clearly evident (Figure 1).
As a consequence of this finding, serial echocardiograms for the evaluation of pericardial effusion, ventricular diverticulum size and fetal cardiac frequency were performed. It was shown a progressive increase of the amount of pericardial effusion and few episodes of fetal bradycardia, but no other structural abnormalities were identified. There was no evidence of maternal or fetal infection. At 32+2 weeks of gestation the patient underwent fetal cardiac magnetic resonance imaging (MRI) consisting of a static phase with multiplanar SSFP sequences and dynamic phase with real time SSFP sequences. Magnetic resonance imaging showed a large pericardial effusion of 13 mm at the rear wall of the left ventricle, with an outpouching measuring 15 mm x 10 mm developed on the right ventricular free wall, compatible with a right ventricular diverticulum (Figure 2). Both lungs were compressed with a normal regular intensity. In consideration of this pattern we decided to administer systemic corticosteroids to induce lung maturation. In delivery room, while emergency caesarean section was performed at 33+3 weeks of gestation, as a consequence of signs of fetal bradycardia, both cardiologist and cardiac surgeon were present. The mother delivered a live male infant in good conditions, weighing 1.880 Kg, with a 1 and 5 minute Apgar score of 8-9 respectively.
Post-natal echocardiography was performed after a few minutes of life and confirmed the presence of the diverticulum and the pericardial effusion, without any sign of cardiac tamponade, so the “heart team” decided not to perform a pericardiocentesis. The scan revealed a patent foramen ovale, patent ductus arteriosus and a multilocular outpouching of the lateral wall of the right ventricle close to the right atrium, just beside the tricuspid valve (Figure 1). During recovery and follow up the baby underwent serial echocardiograms: pericardial effusion regressed progressively and resolved completely by the 7th week of life, while the size of the diverticulum remained unchanged. It was never necessary to perform a pericardiocentesis. In consideration of the asymptomatic clinical setting and the stability of the hemodynamic conditions, the right ventricular diverticulum was not resected, since its contractile pattern was synchronous with the body of right ventricle and it contributed to a significant portion of the right ventricular stroke volume. At 2 and half years of age the diverticulum looks smaller compared to the right ventricle although its dimensions and features were unchanged. The right ventricle is growing up while the diverticulum remains unchanged in size and shape.
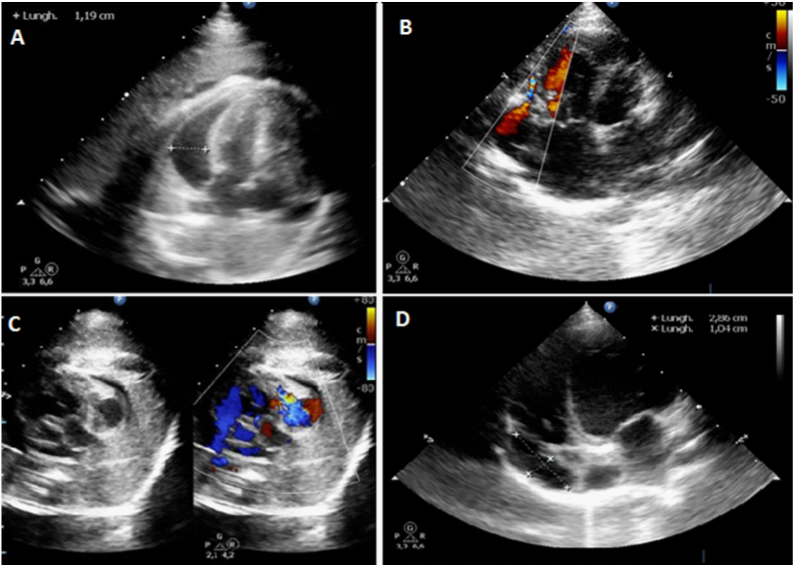
Figure 1 Right Ventricular Diverticulum Echocardiography (Fetal and Neonatal).
Panel A: Apical ultrasound scan revealing 12mm pericardial effusion (White arrow).
Panels B and C: Color-Doppler showing bi-directional flow into and from the diverticulum (White Arrows).
Panel D: Neonatal Echocardiogram demonstrating multilocular out pouching of the lateral wall of the right ventricle with a narrow neck, close to the right atrium (White Arrow), just beside the tricuspid valve. The diameters of the diverticulum were 29mm x 10mm.
The natural history of right ventricular diverticula is variable. Some cases are discovered incidentally at autopsy and others cause sudden death due to congestive heart failure, rupture or arrhythmias.6,8 Although the prenatal history of this condition remains unclear, the overall prognosis appears to be favorable and, even if associated with pericardial effusion, conservative management may be a reasonable option,8 unless there is impending risk of rupture (rare), cardiac tamponade or significative lung compression. Pulmonary hypoplasia may be a consequence of pericardial effusion during fetal life. Our patient was affected by right ventricular diverticulum with pericardial effusion without other cardiac anomalies, and the choice of our conservative treatment was guided by the absence of effusion related symptoms, by the extremely low risk of rupture, confirmed by the synchronous systolic and diastolic contractile pattern of diverticulum with normal cardiac wall, and by the absence of other cardiac malformations.
Among the therapeutic options, fetal pericardiocentesis has been suggested as a means of decompressing the fetal thorax, allowing reexpansion of the lungs and reduction in systemic venous pressure, leading to a theoretical reduction in the risk of pulmonary hypoplasia and hydrops in the fetus.1,5,8 We could have drained the pericardium during the antenatal period to improve lung maturation, but the risk was considered too high and therefore not worthwhile. Pulmonary hypoplasia completely resolved, managed only with corticosteroid therapy. In consideration of the hemodynamic stability, despite the amount of fluid, we decided to be conservative and not to drain. At the end we can say that was wise to wait and see because pericardial effusion disappeared progressively (Figure 2).
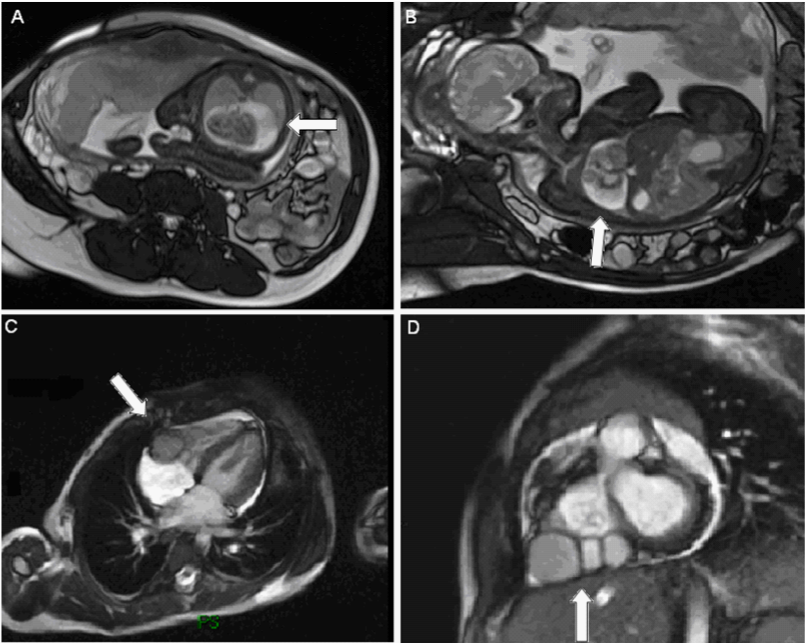
Figure 2 MRI Imaging Fetal MRI (A,B) in which is visible a large amount of pericardial effusion rounding the heart at the rear wall of left ventricle, compressing both lungs and showing pulmonary hypoplasia. Neonatal MRI (C,D) showing the multilocular diverticulum on the right ventricular free wall and the resolution of pericardial effusion.
The case we report has been diagnosed late in comparison with most of cases described in literature. Our experience confirmed that in the absence of hemodynamic impairment, small and asymptomatic diverticula, even associated with pericardial effusion, have a good prognosis. Pericardial effusion may have a spontaneous resolution even after birth and the diverticulum may not require surgical correction. So, prenatal and post-natal watchful waiting was chosen in our case and, to date, the two and half year old infant progresses asymptomatically not requiring any therapeutic intervention.
None.
The authors have no conflict of interests related to this publication and have not received any grants.
None.

©2014 Caldaroni, et al. This is an open access article distributed under the terms of the, which permits unrestricted use, distribution, and build upon your work non-commercially.
 World Down Syndrome Day is observed on 21 March 2026 to raise awareness about Down syndrome and to
promote inclusion, early intervention, and quality healthcare for children with genetic conditions. This day highlights the importance
of pediatric monitoring, developmental support, and continued research to improve health outcomes and overall well-being.
Researchers, pediatricians, and healthcare professionals are invited to submit their original research articles, reviews, and clinical
studies related to Down syndrome, neonatal screening, developmental pediatrics, and child health. Manuscripts submitted on the occasion
of World Down Syndrome Day will be eligible for a special publication discount of 30–40% in the Journal of Pediatrics & Neonatal Care (JPNC).
World Down Syndrome Day is observed on 21 March 2026 to raise awareness about Down syndrome and to
promote inclusion, early intervention, and quality healthcare for children with genetic conditions. This day highlights the importance
of pediatric monitoring, developmental support, and continued research to improve health outcomes and overall well-being.
Researchers, pediatricians, and healthcare professionals are invited to submit their original research articles, reviews, and clinical
studies related to Down syndrome, neonatal screening, developmental pediatrics, and child health. Manuscripts submitted on the occasion
of World Down Syndrome Day will be eligible for a special publication discount of 30–40% in the Journal of Pediatrics & Neonatal Care (JPNC).