Journal of
eISSN: 2379-6359


Case Report Volume 4 Issue 4
Surgical Oncology, The Royal Marsden Hospital, UK
Correspondence: James Shaw, Level 1, 122 Remuera Road, Remuera, Auckland, 1050, New Zealand, Tel +64 (9) 524 9599
Received: June 27, 2016 | Published: August 19, 2016
Citation: Cohen-Hallaleh RB, Aldameh A, Dixon P, Wilson C , Shaw JHF (2016) Critical value of CT angiography and fine needle aspirate cytology for a high intra-vagal parathyroid adenoma. J Otolaryngol ENT Res 4(4): 00107. DOI: 10.15406/joentr.2016.04.00107
Introduction: Intravagal undescended parathyroid adenomas are rare, with only a few cases reported in English literature.
Case presentation: We report a case of a 21-year-old man referred for further evaluation of persistent primary hyperparathyroidism following two unsuccessful neck explorations. His symptoms included mood swings, feeling depressed, weak and irritable, thirst and poor concentration.
Management and Outcome: An ectopic parathyroid adenoma was excised on the third exploration due to prior localization within the vagus nerve near the skull base using CT angiography, MRI, and fine needle aspiration cytology. The patient’s symptoms resolved, and serum calcium and PTH levels normalized.
Discussion: This case report emphasizes the importance of CT angiography and fine needle aspiration in localization of ectopic parathyroid adenomas.
Keywords: parathyroid, ectopic, accessory, intravagal
Intravagal undescended parathyroid adenomas are rare, with only few cases reported in the English literature. Although the success rate of initial parathyroid surgery is very high in expert surgical hands (up to 98% for conventional four-gland surgery and 97% for focused minimally invasive surgery) there is a need for some patients to have a re-operation. This group represents approximately 2-7% of all parathyroid operations.1 The objective of this report is to describe preoperative localization and operative management of a high cervical intra-vagal capsule parathyroid adenoma in a young man with persisting primary hyperparathyroidism following two initial surgical explorations.
A 21-year-old man presented to the original surgeon with a diagnosis of primary hyperparathyroidism. His symptoms included mood swings, feeling depressed, weak and irritable, thirst and poor concentration. The calcium level was 3.12 mmol/l and PTH 15 pmol/l. There was no family history of endocrinopathy and prolactin, gastrin and calcitonin levels were normal. Genetic studies for MEN I and II were negative.
Prior to the initial operation, ultrasound and sestamibi scanning failed to localize an adenoma. A neck exploration revealed two parathyroids on the right side with one being low down in the thymic horn. On the left side, a normally situated superior parathyroid only was found. A decision was made for a conservative approach and further investigation. Post-operatively, selective venous sampling for PTH identified a level >500 pmol/l at the level of the thyroid cartilage on the left side of the neck.
A second procedure involved re-exploration of the carotid sheath to a higher level on this occasion. No abnormality was found and a left thyroid lobectomy was performed. Histology identified a normal subcapsular parathyroid. Further investigations included repeat venous sampling which confirmed the previous findings. A CT angiogram identified a 15x8x6mm fusiform swelling within the carotid sheath near the base of the skull. A fine needle aspirate caused the patient to gag and cytology confirmed parathyroid cells.
At the third operation, this swelling was identified within the vagus nerve near the skull base and it was removed leaving an intact nerve. The patient was noted to have a left sided Horner’s syndrome post-operatively. Histology confirmed parathyroid tissue. Two years later, serum calcium and PTH levels remain normal. The patient’s symptoms have resolved.
The etiology of persistent hyperparathyroidism is most frequently a missed adenoma that is often in an ectopic location. Of these, undescended adenomas represent a small but important proportion. Undescended glands generally lie at the level of the common carotid bifurcation, anterior to or within the carotid sheath.
Embryologically intravagal parathyroid, also known “undescended parathymus,” are inferior glands that fail to descend, remaining at the level of the pharyngeal pouch of origin (third) and often surrounded by a rim of thymic tissue. Gilmour first described the embryological explanation for ectopic parathyroid tissue within the vagus nerve in still born infants, where accessory parathyroid tissue was found within the ganglion of the vagus nerve. The third branchial pouch which gives rise to the inferior parathyroid is in direct relation to the vagus nerve.2 Doppman also demonstrated the occasional development of intravagal parathyroid adenomas.3,4 The objective of this report is to describe a rare case of persisting hyper functioning parathyroid gland found within the vagus nerve following two previous initial operations. A high cervical localization was established by selective venous sampling, MRI and FNA. Successful removal of the intravagal parathyroid gland was achieved with subsequent resolution of calcium and parathyroid levels. The adenoma was located within the vagus nerve above the level of the carotid bifurcation at the skull base and the tumor was enucleated without sacrificing the vagus nerve.
Although rare, intravagal parathyroid adenomas do occur. Therefore, examination of the vagus nerve should be strongly considered when four normal glands are found, as intravagal adenomas appear to represent accessory ectopically located parathyroid tissue in patients with persisting high calcium level post four-gland parathyroidectomy. Our experience serves to emphasize that, in re-operative parathyroid surgery, preoperative localization of the offending parathyroid gland is critical. This should include selective venous sampling to identify the sight of the missed gland. Formal CT and MRI can identify site of parathyroid adenomas. Finally, CT or USS guided FNA allows the surgeon to histopathologically confirm the offending parathyroid gland prior to surgery (Figures 1a-1c, 2 & 3).
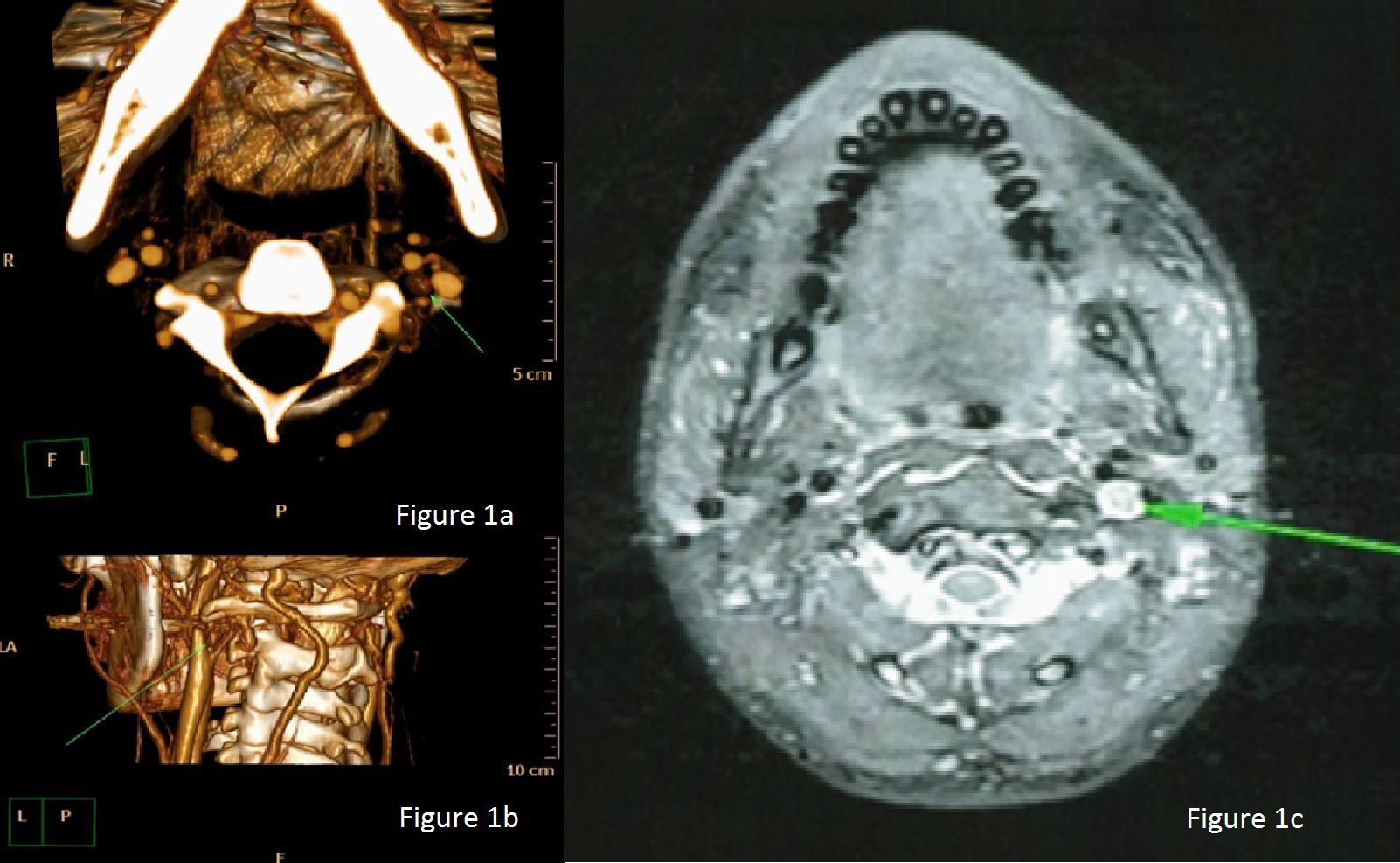
Figure 1a 3D-reconstructed Axial Computed Tomography Angiogram image demonstrating a small mass in the left carotid triangle.
Figure 1b 3D reconstructed image of a Computed Tomography Angiogram showing the mass posterior to the left internal carotid artery.
Figure 1c Axial contrast-enhanced T1-weighted Magnetic Resonance Imaging shows an avidly enhancing mass in the left carotid space.
None.
Author declares there are no conflicts of interest.
None.

©2016 Cohen-Hallaleh, et al. This is an open access article distributed under the terms of the, which permits unrestricted use, distribution, and build upon your work non-commercially.