Journal of
eISSN: 2373-6410


Clinical Images Volume 12 Issue 6
Serviço de Medicina Interna, Hospital da Senhora da Oliveira, Portugal
Correspondence: Sara Fernandes da Silva, single. Rua David Mourão Ferreira, nº 78, 3 DRT-FT, 4700-442 Braga, Portugal , Tel +351914312872
Received: September 26, 2022 | Published: December 15, 2022
Citation: Silva S, Leite LM, Barbosa S, et al. When a headache ends in death. J Neurol Stroke. 2022;12(6):203-204. DOI: 10.15406/jnsk.2022.12.00529
A 42-year-old female, emigrant on vacation in our country, with a history of triple negative breast cancer, status post right radical mastectomy and lymph node dissection, neoadjuvant chemotherapy and radiotherapy went to the emergency department for severe headache, nausea, vomiting and dizziness with a week of development. The analytical study showed an unchanged blood count, renal and liver function, and tumor markers CEA, CA 125, CA 19.9, CA 15.3 negative. Brain computed tomography scan showed a voluminous lesion occupying space at the left frontal cortico-subcortical interface, with a rounded configuration and relatively well-defined limits, measuring about 3.1 cm in maximum anteroposterior and transverse diameters. The lesion takes up the contrast product, compatible with secondary nature and is accompanied by edema. This set of alterations leads to molding of the ventricular system and deviation of the median structures to the right by about 0.8 cm. Whole body scintigraphy: No evidence suggestive of osteoblastic metastases. Nuclear magnetic resonance imaging with 3.5 cm anterior fronto-insular cortico-subcortical space-occupying lesion on the left, intense heterogeneous enhancement after gadolinium and extensive vasogenic edema, with right lateral deviation of midline structures up to 1 cm (Figures 1–3). Patient was medicated with levetiracetam, dexamethasone and 20% mannitol and transferred to the Neurosurgery Service of Centro Hospitalar de São João for continued care, where she died.
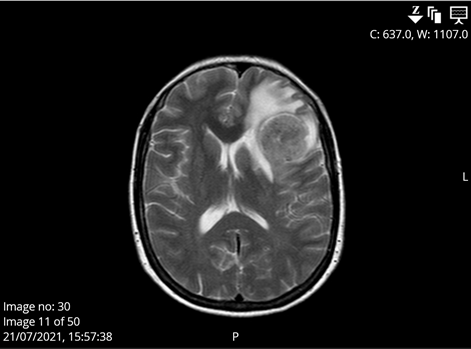
Figure 1 Cross-section of CT scan showing a lesion occupying space at the left frontal cortico-subcortical interface measuring about 3.1 cm in maximum anteroposterior and transverse diameters. The lesion takes up the contrast product, compatible with secondary nature and is accompanied by edema. The ventricular system is deviated from the median structures to the right by about 0.8 cm.

Figure 2 Sagittal section of CT scan showing a lesion occupying space at the left frontal cortico-subcortical interface measuring about 3.1 cm in maximum anteroposterior and transverse diameters. The lesion takes up the contrast product, compatible with secondary nature and is accompanied by edema.

Figure 3 Coronal section of CT scan showing a lesion occupying space at the left frontal cortico-subcortical interface measuring about 3.1 cm in maximum anteroposterior and transverse diameters. The lesion takes up the contrast product, compatible with secondary nature and is accompanied by edema. The ventricular system is deviated from the median structures to the right by about 0.8 cm.
None.
The authors declare no conflicts of interest.

©2022 Silva, et al. This is an open access article distributed under the terms of the, which permits unrestricted use, distribution, and build upon your work non-commercially.