Journal of
eISSN: 2373-6410


Research Article Volume 14 Issue 3
1Medical student, University of Ribeirão Preto, Brazil
10Medical Student, Nove de Julho University, Brazil
11Physiotherapist, Universidade Paulista UNIP, Brazil
12Medical student, UCP, Central University of Paraguay, Ciudad del Este, Paraguay
13Bachelor of Medicine, Faculty of Medical Sciences of Paraíba - FCM/ PB, Brazil
14PhD in Medical Sciences. University of São Paulo, Ribeirão Preto Medical School, Brazil
2Medical student, Nove de Julho University, Brazil
3Medical student, Central University of Paraguay
4Medical student, University of Southern Santa Catarina. Tubarão, Brazil
5Medical student, Potiguar University– UNP, Natal, Brazil
6Medical student, University of Rio Verde, Aparecida de Goiânia. Goiás, Brazil
7Medical student, University of Rio Verde, Formosa. Goiás, Brazil
8Bachelor of Medicine. Severino Sombra University,Vassouras. Rio de Janeiro, Brazil
9Physiotherapist, Nove de Julho University, Brazil
Correspondence: Thiago A Rochetti Bezerra, Medical student, University of Ribeirão Preto. Guarujá, São Paulo, Brazil
Received: April 30, 2024 | Published: May 8, 2024
Citation: Malaquias DTM, Vivas AD, Paschoal JFB, et al. The use of immunomodulators in multiple Sclerosis: diagnosis, treatment and neurological examination. J Neurol Stroke. 2024;14(3):56-61. DOI: 10.15406/jnsk.2024.14.00584
Introduction: Multiple sclerosis (MS) is the most common autoimmune, demyelinating, chronic disease of the central nervous system (CNS) in young adults. It is a complex and heterogeneous condition due to the involvement of various pathophysiological processes including inflammation, demyelination, axonal injury and repair mechanisms. These processes characterize MS as a progressive and unpredictable disease. The diagnostic definition of MS is no easy task, as there is no specific marker.
Objectives: To carry out a descriptive review study on the use of immunomodulators in multiple sclerosis, from diagnosis to treatment.
Material and methods: A descriptive review study was carried out on the use of immunomodulators in multiple sclerosis, from diagnosis to treatment. The studies were analyzed from February to March 2024, with a sample of 34 scientific articles analyzed.
Results and discussion: The initial assessment of a patient with MS usually begins with the patient's medical history and a detailed account of the symptoms, including their onset, duration and pattern. Neurologists pay particular attention to the type of symptoms, their progression and any relapses or remissions.
Conclusion: In conclusion, navigating the complexities of Multiple Sclerosis (MS) requires a comprehensive and personalized approach to diagnosis and treatment. From the intricate process of diagnosing the disease, through a combination of clinical assessments, MRI scans and other diagnostic tools, to the wide range of treatment options, including disease-modifying therapies, symptomatic treatments and lifestyle modifications, managing MS is a multifaceted endeavor.
Keywords: multiple sclerosis, central nervous system, cerebrospinal fluid tests
Multiple sclerosis (MS), an idiopathic inflammatory disease of the central nervous system, is pathologically characterized by demyelination and subsequent axonal degeneration.1 According to Tilbery et al,2 the disease usually presents in young adults and affects twice as many women as men. The most common symptoms include numbness, weakness, visual impairment, loss of balance, dizziness, urinary urgency, fatigue and depression. The diagnosis of multiple sclerosis should be made by a doctor with experience in identifying the disease.3
For De Oliveira et al.4 the diagnosis should be based on objective evidence of two or more neurological signs located in the brain or spinal cord and disseminated in time and space (i.e. occurring in different parts of the central nervous system with an interval of at least three months). The process of diagnosing Multiple Sclerosis (MS) is as complex as the disease itself, requiring a careful and methodical approach from neurologists to ensure accuracy. Since the symptoms of MS can mimic those of many other neurological conditions, neurologists employ a multifaceted strategy to rule out other causes and confirm the presence of MS.5
Multiple sclerosis (MS) is considered a disease with unknown etiology, although there is evidence of multifactorial causes. It mainly affects young adults, predominantly females, of white ethnicity and aged between 20 and 40 years.6 This disease is slow and progressive, with remission of outbreaks, presenting itself in different ways according to the type: a) Recurrent remitting (RR); b) Secondary progressive (SP); c) Primarily progressive (PP); and d) Progressive recurrent (PR). It is therefore extremely necessary to carry out up-to-date studies on immunomodulators in multiple sclerosis, from diagnosis to treatment.3
To carry out a descriptive review study on the use of immunomodulators in multiple sclerosis, from diagnosis to treatment.
A descriptive review study was carried out on the use of immunomodulators in multiple sclerosis, from diagnosis to treatment. The studies were analyzed from February to March 2024, with a sample of 34 scientific articles analyzed. This type of method allowed for a broad description of the subject, but did not exhaust all sources of information, since it is not carried out through a systematic search and analysis of the data. Its importance lies in the rapid updating of studies on the subject.
In the State of Knowledge, methodologies were used considering some sectors of publications on the subject to be analyzed, through articles, complete works, books, and it was not necessary to cover all means of production. This required a more in-depth review of the specific literature on immunomodulators in multiple sclerosis, as well as an overview of the data that has been valued over time, in addition to identifying the theoretical references presented in the publications.
Study participants
Medical undergraduates from various periods took part in the study.
Initial assessment
The initial assessment of a patient with MS usually begins with the patient's medical history and a detailed account of the symptoms, including their onset, duration and pattern. Neurologists pay close attention to the type of symptoms, their progression and any relapses or remissions. This historical insight is crucial, as MS is characterized by symptoms that can fluctuate and recur over time.7,8
Neurological examination
This is followed by a comprehensive neurological examination, where the neurologist assesses functions such as vision, balance, coordination, strength and reflexes. This examination helps to identify deficiencies that may be indicative of central nervous system involvement, a hallmark of MS.9
Magnetic resonance imaging (MRI)
According to Thompson et al,10 MRI scans are fundamental in the process of diagnosing MS. They provide detailed images of the brain and spinal cord, revealing lesions or areas of demyelination that suggest MS. Neurologists often use MRI scans to look for evidence of damage in various areas of the central nervous system that occurred at different times. The use of contrast material (gadolinium) can help distinguish between old and new lesions, offering insights into disease activity. Figure 1 shows the characteristic appearance and locations of demyelinating lesions in MS.
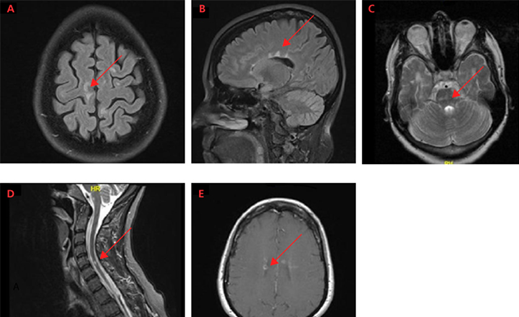
Figure 1 Characteristic appearance and locations of MS demyelinating lesions: (A) juxtacortical lesions;(B) periventricular lesions (Dawson's fingers); (C) pontine lesions (infratentorial lesions are better visualized in T2 sequences); (D) spinal cord lesion in C5-C6; (E) lesions with gadolinium enhancement.
Magnetic resonance imaging is altered in 87 to 95% of cases and shows hypointense lesions in T1 and hyperdense lesions in long TR slices (T2, PD, FLAIR) and contrast enhancement of active lesions. The most frequently affected areas are the semi-oval centers, periventricular white matter, corpus callosum, brainstem, optic radiations, cerebellar peduncles, cerebellum, optic nerves and spinal cord.7 The need for the patient to present 2 outbreaks for diagnosis can currently be replaced by 1 outbreak associated with the progression of lesions on MRI (new lesions or the appearance of gadolinium impregnation in previously unimpregnated lesions, or an increase in the size of previous lesions), after the first outbreak.9
In MS, CT scans of the skull are altered in 36 to 44% of cases, showing hypotensive areas in the white matter, ventricular enlargement and cerebral atrophy. Active lesions show enhancement in the contrast phase.9 According to Garg & Smith,11 MRI with gadolinium contrast, especially during or after a first attack, can be useful for providing evidence of lesions in other parts of the brain and spinal cord. A second MRI scan can be useful at least three months after the initial attack to identify new lesions and provide evidence of spread over time.12
Magnetic resonance imaging (MRI) has been shown to be highly sensitive in detecting clinically silent MS plaques. Consequently, the findings of this imaging modality have been included in the diagnostic criteria proposed by a number of researchers. The main advantage of the proposed criteria is that an early diagnosis of MS can be made if an MRI performed three months after a clinically isolated attack demonstrates the formation of a new lesion. The proposed diagnostic criteria also define the characteristics of MRI lesions that increase the likelihood of MS, including the number of lesions (nine or more), the location of the lesions (position next to the ventricles; just cortical, infratentorial or spinal position) and the enhancement of the lesions with the use of contrast medium.
It is essential to exclude other diseases that can mimic multiple sclerosis, including vascular disease, spinal cord compression, vitamin B12 deficiency, central nervous system infection (e.g. Lyme disease, syphilis) and other inflammatory diseases (e.g. sarcoidosis, systemic lupus erythematosus, Sjögren's syndrome).13 For Myhr,5 the diagnosis of MS is based on the presence of lesions in the central nervous system (CNS) that are disseminated in time and space (i.e. occur in different parts of the CNS with an interval of at least three months), without a better explanation for the disease process. Since no single test is completely reliable in identifying MS and a variety of conditions can simulate the disease, diagnosis depends on clinical features complemented by the results of certain studies.
Typical clinical and MRI activity in MS (Figure 2). MRI activity is typically more frequent than clinical relapses (peaks of clinical disability), indicating that more disease activity is occurring than is clinically apparent. Loss of brain volume and increased disease burden (total lesion volume), both measured on MRI, indicate permanent tissue damage, which is present early in the disease and progresses gradually over time.13
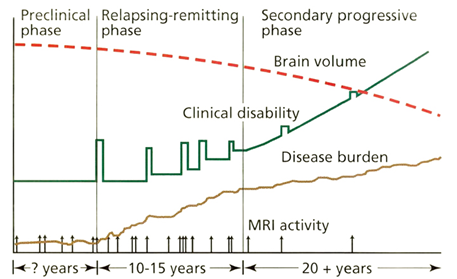
Figure 2 MRI activity (vertical arrows) indicates an inflammatory process, measured on brain MRI by gadolinium enhancement or new hypertensive brain lesions.
Etiology
It is still little known, but it is assumed that the causes are multifactorial, such as genetic susceptibility, autoimmune mechanisms, exposure to stress factors, exposure to sunlight, smoking and viral infections. The increase in immunoglobulin oligoclonal bands in the cerebrospinal fluid of 65 to 95% of patients with multiple sclerosis is evidence of a persistent viral infection, or of a CNS autoantigen.2
Lumbar puncture (pin prick)
Although not always necessary, a lumbar puncture can be performed to analyze cerebrospinal fluid (CSF) - the fluid that surrounds the brain and spinal cord. This test looks for abnormalities linked to MS, such as high levels of specific proteins or the presence of oligoclonal bands, which are bands of immunoglobulins found in the CSF of most people with MS.14
Evoked potential tests
Evoked potential tests measure electrical activity in the brain in response to visual, auditory or sensory stimuli. These tests can detect delayed responses due to MS-related nerve damage, even when symptoms are not present, providing additional evidence of MS.15
Differential diagnosis
An essential part of the diagnosis of MS is the exclusion of other conditions that can cause similar symptoms. Conditions such as Lyme disease, vitamin B12 deficiency and lupus (among others) can mimic MS, so neurologists usually perform a variety of tests to exclude them. This process ensures that the diagnosis of MS is made with a high degree of confidence.16
The McDonald criteria: a diagnostic tool for MS
The McDonald Criteria is a tool that neurologists use to facilitate the diagnosis of MS. Periodically updated to reflect advances in understanding and technology, these criteria incorporate the findings of MRI scans, clinical assessments and additional tests, such as CSF analysis. The McDonald Criteria allow for an earlier and more accurate diagnosis of MS by defining specific guidelines on the evidence of damage to the central nervous system and its spread over time and space.17,18
Emphasizing early and accurate diagnosis
Early and accurate diagnosis is crucial to managing MS effectively. It allows for the timely initiation of treatment to control symptoms, reduce relapses and potentially slow down the progression of the disease. The MS diagnosis process reflects the complexity of the disease, but is designed to ensure that patients receive an accurate diagnosis and the best possible care.19
Variety of therapeutic approaches
Treatment options for Multiple Sclerosis (MS) are multifaceted and tailored to manage the complex nature of the disease, with the aim of reducing disease activity, managing symptoms and improving quality of life. MS treatment has evolved significantly, offering patients a variety of therapeutic approaches.18
Disease-modifying therapies (DMTs)
Mahad et al20 cites that DMTs are at the forefront of MS treatment, designed to reduce the frequency and severity of relapses, slow the progression of disability and limit new disease activity as seen on MRI scans. These drugs target the inflammatory processes of the disease and can be categorized based on their mode of administration:
✓ Injectables: Include interferon beta preparations and glatiramer acetate, which have been used for many years and are often considered for initial therapy.
✓ Oral Medications: Such as fingolimod, dimethyl fumarate, teriflunomide and siponimod, offer an alternative to injections and vary in mechanisms of action and side effect profiles.
✓ Infusions: Highly effective treatments such as natalizumab, ocrelizumab, alemtuzumab and rituximab are administered via intravenous infusion and are usually used for more aggressive forms of MS or when other therapies have failed.
Treatment for MS relapses
MS relapses or exacerbations, characterized by new or worsening neurological symptoms, are often treated with corticosteroids to reduce inflammation. Intravenous methylprednisolone is the most common treatment, sometimes followed by a course of oral steroids. For severe relapses that do not respond to steroids, plasmapheresis (plasma exchange) can be considered.3,21
Symptomatic treatments
Symptomatic treatments in MS are crucial for improving quality of life and are tailored to the specific symptoms each patient experiences.22,23 These can include:
✓ Mobility and Spasticity: Physiotherapy, muscle relaxants (e.g. baclofen, tizanidine) and sometimes botulinum toxin injections.
✓ Fatigue: Management strategies include energy conservation techniques, exercise and medication such as amantadine or modafinil.
✓ Pain: Treatments for neuropathic pain include anticonvulsants (e.g. gabapentin, pregabalin) and antidepressants (e.g. amitriptyline, duloxetine).
✓ Bladder and bowel problems: Anticholinergics for bladder control and dietary modifications, laxatives or stool softeners for bowel management.
✓ Cognitive and Emotional Health: Cognitive rehabilitation and psychotherapy, along with medication for mood disorders.
Lifestyle modifications and complementary therapies
Lifestyle changes and complementary therapies can play an important role in the management of MS.24–26
Examples:
✓ Diet and Nutrition: Although no specific diet has been proven to alter the course of MS, healthy eating patterns can support overall well-being.
✓ Exercise: Regular physical activity can help improve strength, fatigue, mobility and mood. Stress Management: Techniques such as meditation, yoga and mindfulness can help control stress, which can exacerbate symptoms.
✓ Alternative therapies: Some patients find relief with acupuncture, massage or other complementary therapies, although these should not replace conventional treatments.24–26
Medical cannabis
The use of medical marijuana for the treatment of Multiple Sclerosis (MS) symptoms has attracted significant interest and research in recent years.27–29
Examples:
✓ Active compounds in cannabis, such as THC (tetrahydrocannabinol) and CBD (cannabidiol), have been explored for their potential to relieve various MS symptoms, including pain, muscle stiffness (spasticity) and sleep disturbances.
✓ Clinical studies suggest that medical marijuana may provide relief for some individuals with MS, leading to improvements in quality of life and functional outcomes.
✓ Healthcare professionals recommend careful consideration of the benefits versus potential side effects, such as cognitive impairment, dizziness and interactions with other medications.
Emerging therapies
The field of multiple sclerosis research is active, with ongoing clinical trials investigating new treatments, including stem cell transplantation and therapies targeting specific immune mechanisms. These emerging therapies offer hope for even more effective treatments in the future.30
Tailor-made treatment plans
It is important to note that MS treatment is highly individualized. Neurologists work closely with patients to develop a treatment plan that suits their specific form of disease, lifestyle and treatment goals. Regular monitoring through clinical evaluations and MRI scans is crucial to assess the effectiveness of treatment and make adjustments as necessary.12
Metz31cites that without specific medications for each symptom, spasticity, bladder dysfunction, depression and fatigue can be relieved. Five disease-modifying treatments for multiple sclerosis have been approved by the U.S. Food and Drug Administration. These treatments are partially effective in reducing exacerbations and may slow the progression of disability.
Discussion on the treatment of MS with Immunomodulators
The treatment of MS sufferers with immunomodulators and immunosuppressants has changed the course of the disease in recent years. The Ministry of Health is responsible for releasing the use of these drugs, which are: Interferon beta (INF) and glatiramer acetate (GA). This body has also decided to distribute them free of charge through the Unified Health System (SUS). With the growing demand for the prescription of these drugs and their high cost, protocols and recommendations for their use have been drawn up, which are the process of including or excluding patients from treatment.16
The recommendations are:
The use of Lovastatin and Simvastatin in MS patients has shown a reduction in the lesions visualized by magnetic resonance imaging and the absence of serious side effects. Despite the non-curative effects, several benefits of these drugs are known, but side effects have been reported in several studies, which, if properly identified and guided, can prevent treatment interruption.22
According to Filippi,33 most of the time the adverse effects are mild and transient and are related to poor application technique and may be the main cause of loss of adherence to treatment. Most patients receive instructions on the preparation and administration of immunomodulators, but it is important to assess their understanding of this information on a regular basis. Interferon plays an important role in the immune system by producing effects on T and B cells and influencing the blood-brain barrier. Several mechanisms of action have been proposed for Glutamic Acid, but its biological effects are not yet fully understood.
Glutamic acid is reported to act by inhibiting reactive T-cells, diverting them away from myelin. It is also assumed that it suppresses the immune system, thus reducing the destruction of the myelin sheath.34 According to research by Cree Ba,34 patients treated with 20mg of GA daily showed a 29% reduction in the relapse rate over a 2-year period. It also reduced the progression of disability by 12%. However, there are side effects, but these are milder, with only a reaction at the inoculation site, such as erythema and induration.
Renoux7 followed up a patient with MS, diagnosed according to the McDonald criteria, who was first treated with Interferon, but began to show side effects, leading her to refuse treatment with injectable drugs. She was then offered another form of treatment with Rosuvastatin, and after 6 months of use she had no undesirable effects. Two months after starting treatment, the patient's neurological condition had improved, and she was able to walk longer distances, exercise and no longer needed a bladder catheter. After 6 months of use, the EDSS dropped to 4.5 (previously 6.0) with improved pyramidal and bladder functions. Body balance depends exclusively on the integrity of the vestibular system (labyrinth, nerve, vestibulocochlear, nuclei, pathways and interrelationships in the CNS), the somatosensory system and vision, under the coordination of the cerebellum.
A person with MS has a lesion in one of these systems, leading to conflicting information, and thus symptoms of body imbalance and dizziness. The main forms of treatment for these vestibular dysfunctions are medication, surgery and vestibular rehabilitation (VR). This VR acts physiologically on the vestibular system through central neuroplasticity mechanisms known as adaptation, habituation and substitution to achieve vestibular compensation.25 In recent years, in addition to invasive treatment, there has also been physiotherapeutic treatment which, according to studies, is showing positive results in terms of the physical movement of sufferers, as well as improving their quality of life.
All the studies that were carried out found that this pathology predominates in young, female adults. It affects the white matter of the CNS, causing multiple lesions or plaques. It has no defined etiology, but is thought to be a multifactorial disease.
In conclusion, navigating the complexities of Multiple Sclerosis (MS) requires a comprehensive and personalized approach to diagnosis and treatment. From the intricate process of diagnosing the condition through a combination of clinical assessments, MRI scans and other diagnostic tools, to the wide range of treatment options, including disease-modifying therapies, symptomatic treatments and lifestyle modifications, managing MS is a multifaceted endeavor.
None.
The authors declare that there are no conflicts of interest.

©2024 Malaquias, et al. This is an open access article distributed under the terms of the, which permits unrestricted use, distribution, and build upon your work non-commercially.