Journal of
eISSN: 2373-6410


Case Report Volume 12 Issue 1
1University Master’s Degree in Drug Dependency and Other Addictions, Filiation: Ministerio de Salud Pública del Ecuador-
2University Master’s Degree in Health Management and Direction, Universidad de Cuenca, Maestría de Medicina Legal y Forense, Ecuador
Correspondence: Andrés Joaquín Guarnizo Chávez, University Master’s Degree in Health Management and Direction, Universidad de Cuenca, Maestría de Medicina Legal y Forense, Ecuador, Tel +593 958967098
Received: September 29, 2021 | Published: January 21, 2022
Citation: Heredia NAR, Chávez AJG. Psychocutaneous disorder due to university stress-A case study. J Neurol Stroke. 2022;12(1):5-7. DOI: 10.15406/jnsk.2022.12.00488
Psychocutaneous disorders, or allergies exacerbated by psychological factors in adults, are a group of dermatological diseases, where an underlying condition such as atopic dermatitis is triggered by psychological stressors, and whose diagnosis is made by clinical, questioning, and ruling out others most frequent skin pathologies. It is closely linked to certain triggering psychological factors, which can be stress or anxiety. The present article includes a case study of an undergraduate patient, with the classic symptoms of a skin allergy. However, her case undergoes diagnostic trials without revealing any apparent cause. By means of a more thorough anamnesis, the stress factors that produce the skin affectation are identifiable.
Keywords: Dermatitis, Urticaria, Stress psychological, Allergy, Psychodermatology, Psychological factors
Human physiology is so complex and interlinked that it is practically impossible to separate the physical component from the psychological in an affectation,1 and dermatological affectations are not the exception. In fact, it is widely accepted that factors such as anxiety and stress can induce or exacerbate skin pathologies such as psoriasis, hives, eczemas, and atopic dermatitis.2 This psychological component is not unusual in the clinical practice of the field.
Regarding epidemiology, the number of reported cases is not clear, either due to their underdiagnosis, or because of the little literature available so far, however, a high prevalence of psychiatric disorders is described in the dermatological consultation, mainly related to major depression. Between 20% and 40% of dermatological patients suffer from psychiatric or psychological illnesses, and it is described that these types of patients have up to 20% more alterations than the general population. It is also estimated that a third of dermatological patients require a joint assessment of emotional and psychosocial factors, showing an important relationship between these two specialties, which several authors indicate as a consequence of the common ectodermal origin of the skin and the central nervous system.3
Approximately 75% of specialists consider psycho-dermatological pathologies as a frequent phenomenon in their clinics.4 In this context, its important to recognize Psychocutaneus disorders as a psychosomatic illness which emerges as a reaction from the immune system as a result of an uncomfortable or stressful situation or event, that in some way alters the psychological homeostasis of the individual, and which manifests in the skin through: itching, hives, eczemas, etc.
Due to the limited number of articles on this pathology and its importance in the differential diagnosis of other skin allergies, the corresponding case report is made below. The present study follows the guidelines of the CARE guidelines (consensus-based clinical case reporting guideline). Our patient signed the respective informed consent for academic purposes and its confidentiality has been respected.5
The patient is a 23-year-old woman, a medicine undergraduate student, that consulted with a physician since she has manifested intense itching for about a week, eczematous marks on both cheeks, as well as on her upper extremities. Patient indicates no significant allergic history in his family, mother in psychological treatment for anxiety symptoms 3 years ago. Neither does her medical record report any previous allergy or atopic illnesses, only stems from a sinusitis treatment, nor can the apparition of these injuries be attributed to any contact, food intake, or medications. In the physical exam an urticarial lesion is revealed, its diameter is around 5 centimeters, with hives of slightly elevated edges, on the right cheek, no flaking (Figure 1) a similar lesion is visible, but smaller, on the left cheek. The same lesions appear to be on the internal part of the forearm. On physical examination, the skin does not react with dermographism or temperature changes.

Figure 1 Lesions at the beginning of consultation.
Urticaria-like lesion with erythema, hives, and papules is observed in the right cheek.
An unspecific allergic reaction is diagnosed and, second generation antihistamines are prescribed, which the patient prefers to take, but with a considerable side effect of drowsiness that affects her studies. In a following consultation she is given a low dosage of topical corticoids, without evidencing any clinical improvement. It is at this point that the patient indicates that the symptoms and signs appear in a fluctuating manner, with short periods of exacerbations and referrals, for which besides beginning the use of third generation antihistamines (Fexofenadine) to avoid the drowsiness effect, which certainly improves the chart (Figure 2). She is referred to the dermatological specialist, whom after the pertinent percutaneous exams like Late Reading Patch Test, rules out that the patient is sensitive to any investigated allergen. Controlled oral provocation tests are not performed, because there is no antecedent substance suspected of being desiccated. Additionally, hematic biometry and IgE tests are performed, which do not reveal any unusual value except in mean corpuscular hemoglobin and its concentration, without diagnostic relevance for our case. (Table 1) Histopathological studies were also not performed due to the absence of signs and symptoms related to another type of urticaria, such as leukocytoclastic vasculitis or urticarial vasculitis. So, in this case, she only continues with the same treatment for necessary reasons.
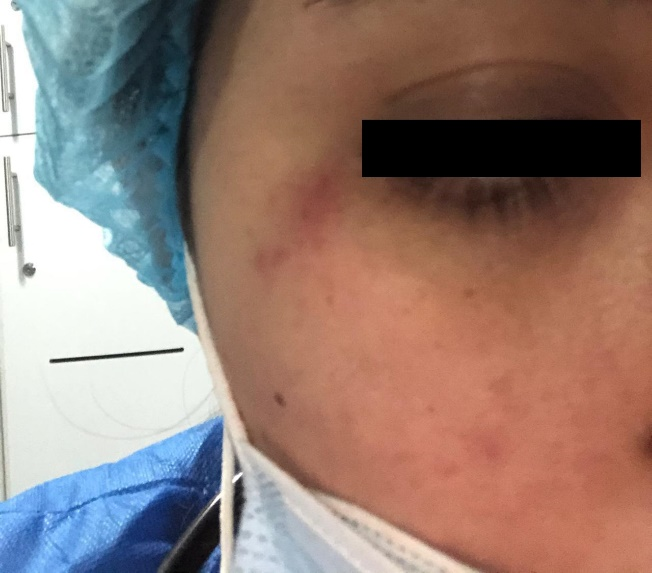
Figure 2 Lesions with Fexofenadine treatment.
Reduction of lesions and hives is observed after one week of treatment.
| Parameters | Results | Normal range |
| WBC# | 8.0 K/µL | 4.0 - 12.0 |
| LYM# | 2.4 K/µl | 1.0 - 5.0 |
| MID# | 0.6 K/µL | 0.1 - 1.0 |
| GRA# | 5.0 K/µL | 2.0 - 8.0 |
| LYM% | 30.40% | 25.0 - 50.0 |
| MID % | 7.40% | 2.0 - 10.0 |
| GRA% | 62.20% | 50.0 - 80.0 |
| RBC | 4.48 M/µL | 4.00 - 6.20 |
| HGB | 15.9 g/dL | 11.0 - 17.0 |
| HCT | 45.10% | 35.0 - 55.0 |
| MCV | 100.7 Fl | 80.0 - 100.0 |
| MCH | 35.5 pg | 26.0 - 34.0 |
| MCHC | 35.3 g/Dl | 31.0 - 35.5 |
| RDW | 10.70% | 10.0 - 16.0 |
| PTL | 249 K/µL | 150 - 400 |
| MPU | 7.8 Fl | 7.0 - 11.0 |
| IgE | 46.7 U.i/mL |
Table 1 Laboratory values
Weeks later, after returning to the consultation, the patient once again refers to the reoccurrence of the chart, for which a much more thorough new anamnesis is initiated, focusing on the psychological aspects when the skin manifestations occurred. The anamnesis revealed in the same that these eczemas concordantly appeared during days of high stress and anxiety in the educational environment; test taking, thesis, important reports in the study program, etc. In light of this new circumstantial evidence, besides the exposure of emotional stress factors, and the absence of suggestive clinical data of any other allergic pathology that inclusively has been rejected by the specialist. Signs and symptoms are consistent with atopic dermatitis that occurs in adulthood, triggered by psychological stressors from college. although it is notable that factors such as elevation of IgE are not found.
Psycho-skin disorders occur when a skin condition like atopic dermatitis is exacerbated when exposed to uncomfortable emotional situations that build up, high levels of stress, anxiety, and burnout,6 being this particularity what motivated the presentation of the case. The most predominant skin manifestations tend to be irruptions, hives, and highly itchy eczemas. In other parts of the body, that go from the upper body and extremities, up until the face; as in the stated case. Other psychosomatic feedback frequently described and related that triggers the stress of this dermatitis can be: migraines, gastritis ulcers, amenorrhea, alopecia, abdominal pain, etc. Since the case is a psychologically triggered allergy, its diagnosis is done by first discarding and then a thorough anamnesis, once all the interventions and exams give a negative. The patient’s specific physiopathology has still not been determined. However, the importance of psychological factors has been proven, from a psycho-neuroimmunology standpoint, in its development, its permanence and deterioration, and its shared situation with other type of atopic and skin illnesses.7 In the case presented, the diagnostic criteria referred to as negativity to all types of skin tests and prevalence of psychological factors have been met. It is also important to note that our patient has normal IgE values for an adult, although most patients with atopic dermatitis (approximately 80%) present elevated IgE values,8 this if a concomitant parasitic disease has been ruled out.
Regarding the best treatment recommended, evidence shows that Nervous Dermatitis has a good therapeutic response to the use of low dosed corticoids and even topical formulations, as well as doses of antihistamines respond. Due to this, and to various skin pathologies are exacerbated by high levels of unchained anxiety through emotional loss, work or work-related tensions,9 and simultaneously the same illness conditions the appearance of stress in a vicious cycle. These patients are also recommended to visit a professional consultation in psychology or in mental health. Among these main psychological recommendations, the patient should receive psychological education, with the purpose of providing information of the cause of the nature of this problem, to provide emotional support, and to enhance an efficient use of free time, physical activity and a healthy and balanced diet.
Studies on psycho-cutaneous disorders indicate that the most common diagnoses for referral are: Anxiety Disorder, Depression, Mood Disorder, Obsessive Compulsive Disorder, Adjustment Disorder, Stress, and Personality Disorder. When psychotropic drugs have been prescribed, the most widely used are anxiolytics, mainly benzodiazepines, followed by antidepressants such as sertraline, followed by mood stabilizers and antipsychotics.10
None.
The authors declare to not have any conflicts of interests.
The authors of the article declare that they do not receive any type of financing for it.

©2022 Heredia, et al. This is an open access article distributed under the terms of the, which permits unrestricted use, distribution, and build upon your work non-commercially.