Journal of
eISSN: 2373-6410


Research Article Volume 8 Issue 4
1University Headache Clinic, Russia
2Department of Neuroscience, IM Sechenov First Moscow State Medical University, Russia
3Faculty of Biology,Lomonosov Moscow State University, Russia
4University diagnostic laboratory, Russia
5Center of Experimental Embryology and Reproductive Biotechnologies, Russia
Correspondence: Eugene Klimov, Department of Genetics, Biological Faculty of Lomonosov Moscow State University, 119234, Moscow, Lenin Hills, 1-12, Russia,
Received: June 01, 2017 | Published: July 23, 2018
Citation: Azimova J, Skorobogatykh K, Sergeev A, et al. Migraine and depression: a comparative assessment of the efficacy and safety of antidepressants in patients with migraine. J Neurol Stroke. 2018;8(4):208-212. DOI: 10.15406/jnsk.2018.08.00311
A number of large-scale epidemiological studies have demonstrated the comorbidity of migraine and depression. Depression is a confirmed modifiable risk factor for chronic migraine. Nevertheless, screening for depression is not included in the migraine management guidelines and standards. The goal of the study was to evaluate the long-term effect of depression on the course of migraine, as well as the efficacy and safety of antidepressant therapy in patients with depression associated with migraine and the effects of this therapy on the prognosis of migraine. This observational, non-interventional study enrolled 544 patients suffering from migraine and assessed the clinical course of migraine and depression. Evaluations were conducted at the initial visit of a patient whose main complaint was headache (Visit 1), at 6 months (Visit 2), and at 12 months (Visit 3). After that, telephone interviews were conducted once a year (Visits 5, 6, 7, 8) to ask for the number of days of headache. Antidepressant therapy was administered in 240 patients with depression, and its long-term effect was later assessed. The longitudinal analysis revealed 6 variants of the course of migraine: persistent episodic migraine, migraine in remission, progression from episodic to chronic migraine, reversion of chronic migraine to episodic migraine, persistent chronic migraine, and recurring (relapsing) chronic migraine. The presence of depression and cutaneous allodynia are predictors of persistent and recurring chronic migraine. In patients with chronic migraine combined with depression, several groups of antidepressants are effective in reducing the number of days of headache: tricyclic antidepressants (TCA), selective serotonin reuptake inhibitors (SSRI), selective serotonin–norepinephrine reuptake inhibitors (SSNRI), and serotonin reuptake antagonists/inhibitors (SRAI). The most pronounced effect was observed with the TCA amitriptyline, the smallest effect was obtained with the SSRI paroxetine. Intermediate results were achieved with the SSNRI venlafaxine and the SRAI trazodone. Trazodone is better tolerated compared with other antidepressants, particularly during the first few weeks of treatment. Screening for and treatment of depression should be included in the migraine management standards.
Keywords: migraine, depression, antidepressant, trazodone
A migraine is a primary headache disorder that is associated with more years of disability than any other neurological condition.1 Episodic migraine (attacks on less than 15 days a month) and chronic migraine (headache on 15 or more days a month over more than 3 months) are distinguished.2 The progression from episodic migraine to chronic migraine (a process called transformation) occurs in approximately 2% of patients with episodic migraine each year.3 Epidemiological studies have identified a number of modifiable and non-modifiable risk factors for the progression to chronic migraine.4 Modifiable risk factors include depression, anxiety, stressful events, obesity, sleep disorders, snoring, excessive consumption of caffeine, excessive consumption of analgesics, and cutaneous allodynia.5,6 The state-of-the-art prevention and treatment programmes for chronic migraine are primarily directed to target modifiable risk factors, because chronic migraine is characterized by worse maladaptation, low quality of life, higher need for medical assistance, and greater occurrence of comorbid somatic and psychiatric diseases, including depression, as compared with episodic migraine.5,7–9 Depression is a psychiatric disease; its main characteristic is low mood. A diagnosis of a depressive episode (ICD-10) requires the presence of two major symptoms and at least three minor symptoms (Table 1).10
Major symptoms |
1. Depressed mood, irrespective of circumstances, for a long time (two weeks or longer) |
2. Anhedonia–loss of interest in or pleasure from activities previously found enjoyable |
3. Persistent fatigue, anergia |
Minor symptoms |
1. Sleep disorders |
2. Sense of guilt |
3. Low self-esteem |
4. Decreased power of concentration |
5. Agitated or retarded movement and speech |
6. Appetite disorders |
7. Thoughts of suicide or suicide attempt |
8. Decreased libido |
Table 1 Diagnostic criteria of a depressive episode
Other forms of depression observed in neurological practice include recurrent depression (recurrent depressive episodes) and dysthymia (persistent depressive disorder). These forms develop largely as a result of inadequate therapy, i. e. administration of drugs with different mechanisms of action (such as tranquilizers or neurometabolic agents) for the treatment of depression, insufficient duration of antidepressant therapy (less than 6 months), and insufficient therapeutic doses of antidepressant drugs.11
Epidemiological studies have demonstrated that the lifetime likelihood of depression in the general population is in the range of 5% to 17%.12 Migraine and depression are highly comorbid and interrelated pathophysiologically.13 Depression increases the risk of migraine 4.5 times.13 A recent study reported by Ashina S et al.,14 that included data collected in over 6,000 patients demonstrated that a depressive episode was the most significant predictor of the transformation of episodic migraine into the chronic form over the next year. The more severe the depression the higher the relative risk of transformation: it was found to be 1.8 in mild depression, 2.4 in moderate depression, and 2.5 in severe depression. Another population-based study showed that depression was the main factor, even regardless of socio-economic factors, number of days of headache per month, amount of analgesic medication, and other comorbidities. It should be underlined that antidepressant therapy, i. e. adequate treatment of depression, does not increase the risk of migraine.15
The objective of this study was to evaluate the long-term effect of depression on the course of migraine, as well as the efficacy and safety of antidepressant therapy in patients with depression associated with migraine and the effects of this therapy on the prognosis of migraine.
This observational, non-interventional study enrolled 544 patients with migraine from the University Headache Clinic (Moscow) database.The study was conducted according to the Declaration of Helsinki Principles.
The inclusion criteria were:
Evaluations were conducted at the initial visit of a patient whose main complaint was headache (Visit 1), at 6 months (Visit 2), and at 12 months (Visit 3). They were followed by telephone interviews (once a year, four visits) or office visits (at the patient's request). An office visit served to obtain the patient's complaints (including the number of days of headache and the qualitative characteristics of the cephalalgia) and medical history and to perform general clinical and neurological examinations. The Headache Diary was employed to verify the number of days of headache and the amount of analgesic medication used. The Beck Depression Inventory was utilized to measure the severity of depression.16
Prophylactic therapy was administered when indicated and in accordance with the international recommendations; the following drug classes were used: tricyclic antidepressants (TCA) (amitriptyline), anticonvulsants (topiramate), beta-blockers (anaprilin, propranolol), botulinum toxin type A.17 Patients with a depressive episode were administered antidepressants (TCA (amitriptyline), selective serotonin reuptake inhibitors (SSRI), selective serotonin–norepinephrine reuptake inhibitors (SSNRI), serotonin reuptake antagonists/inhibitors (SRAI)). Amitriptyline therapy was preferred, when not contraindicated and well tolerated, in patients with chronic migraine combined with a depressive episode. In other cases, SSRI, SSNRI, SRAI, SSRI, and SSNRI were administered for a combination of depression and asthenia and in the presence of multiple somatic complaints and depression symptoms. The SRAI trazodone was given for combinations of depression with sleep disorders and severe anxiety.
Various statistical tests were employed: comparative analysis was performed using Student’s t-test and Fisher’s exact test.
In the overall sample of 544 patients with migraine (82.9% of them female, mean age 42±10.6 years), 67.8%(368 subjects) suffered from episodic migraine and 32.2%(176 subjects) had chronic migraine. A depressive episode meeting the ICD-10 criteria was observed in 240 subjects (44.1% of the overall sample): 71.0% of patients with chronic migraine and 31.5% of those with episodic migraine. The differences between the depression rates in the episodic migraine and chronic migraine groups were statistically significant (р<0.0001).
The longitudinal analysis revealed 6 variants of the course of migraine depending on the number of days of headache per month: persistent episodic migraine, migraine in remission, progression from episodic to chronic migraine, reversion of chronic migraine to episodic migraine, persistent chronic migraine, and recurring (relapsing) chronic migraine. The clinical characteristics of each of the groups are presented in Table 2.
Table 2 demonstrates that the progression from episodic to chronic migraine is characterized by increasing depression levels and that all chronic forms of migraine (persistent migraine, recurring migraine, and reversion of chronic migraine to episodic migraine) are associated with high depression levels from the start. At the same time, the reversion of chronic migraine to episodic migraine is accompanied by a reduction in depression levels. It can thus be assumed that some forms of migraine are associated with depression and thus antidepressant therapy is one of the treatment strategies. A similar association is observed with medication overuse: as the attacks become more frequent while the headache proceeds to a chronic state, the proportion of patients overusing analgesics becomes higher. Afterwards, though, this factor makes the chronic headache persistent.
Symptom |
|
Type 1, persistent episodic migraine |
Type 2, migraine in remission |
Type 3, progression from episodic to chronic migraine |
Type 4, reversion of chronic migraine to episodic migraine |
Type 5, persistent chronic migraine |
Type 6, recurring chronic migraine |
||
Proportion of patients, % |
32% |
7% |
9% |
15% |
21% |
16% |
|||
Age, years |
42.1±7.9 |
31.4±6.5 |
39.9±5.3 |
38.5±7.5 |
43.7±7.8 |
42.8±8.0 |
|||
Number of days of headache per month |
At baseline |
4.1±1.6 |
2.6±1.1 |
6.3±2.3 |
27.1±3.0 |
26.9±2.4 |
27.4±1.2 |
||
At 6 months |
2.5±1.2 |
0.32±0.04 |
4.3±1.8 |
16.5±4.2 |
24.7±3.5 |
14.3±4.7 |
|||
At 1 year |
2.8±1.1 |
0.25±0.02 |
12.5±3.9 |
11.6±3.5 |
27.2±2.4 |
20.3±5.8 |
|||
At 2 years |
3.2±1.1 |
0.30±0.03 |
18.0±5.4 |
5.4±2.1 |
26.4±2.7 |
17.6±5.9 |
|||
At 3 years |
2.9±1.2 |
0.31±0.02 |
22.1±5.8 |
3.9±3.3 |
26.9±2.2 |
22.4±6.8 |
|||
At 4 years |
2.8±1.0 |
0.24±0.02 |
23.9±6.0 |
4.2±2.9 |
27.5±2.4 |
12.5±5.1 |
|||
At 5 years |
3.1±1.1 |
0.22±0.01 |
24.9±4.7 |
4.5±2.3 |
27.3±2.0 |
19.1±5.6 |
|||
Cutaneous allodynia, % of patients |
7% |
0% |
46% |
38% |
52% |
87% |
|||
Medication overuse, % of patients |
At baseline |
0% |
0% |
0% |
73,3 %* |
85.9 %* |
91,9 %* |
||
At 1 year |
0% |
0% |
12.2 %** |
14,6 %** |
76,3 % |
85,4 % |
|||
Depression (Beck Inventory), score |
At baseline |
4.1±1.2 |
4.0±1.2 |
8.6±2.5* |
13.1±3.2* |
14.6±2.0* |
11.3±2.1* |
||
|
At 1 year |
3.1±1.1 |
2.9±0.9 |
12.3±2.4** |
4.7±1.9** |
11.3±2.2 |
10.5±1.9 |
||
Table 2 Clinical characteristics of study subjects
* - p<0.001 (comparison between the groups at the initial visit)
* - p<0.001 (comparison between visits within a group)
All chronic forms of migraine, particularly persistent chronic migraine, were associated with cutaneous allodynia. Cutaneous allodynia is a sensory disorder manifested by painful sensations caused by normally non-painful stimuli (temperature, tactile). Based on the obtained data, one can assume that depression and cutaneous allodynia are predictors of persistent or recurring forms of chronic migraine.
Antidepressant therapy was administered at the initial visit to 240 patients with a depressive episode. Amitriptyline 50–75mg/day was given to 103 patients (42.9%), 44 subjects (18.3%) received the SSRI paroxetine (20mg/day), 42 patients (17.5%) were given the SSNRI venlafaxine (75mg/day), and 51 subjects (21.3%) took trazodone (Trittico) 150mg/day. A positive effect of the antidepressant on the symptoms of depression was observed in all study groups (Figure 1).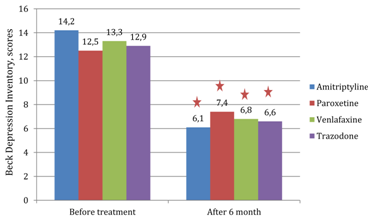
Figure 1 Depression levels (Beck Depression Inventory) before and after antidepressant therapy (at 6 months).
∅-p<0.01
The efficacy of antidepressant therapy in the prevention of migraine is shown in Figure 2. In patients with migraine and a depressive episode, all antidepressants (amitriptyline, paroxetine, venlafaxine, and trazodone) had a statistically significant positive effect (reduction in the number of days of headache per month). The greatest effect was observed in the groups of patients administered amitriptyline (the mean number of days of headache per month decreased from 24.2±2.7 to 9.7±1.7; p<0.001) or trazodone (Trittico) (the mean number of days of headache per month decreased from 23.5±2.4 to 11.6±1.9; p<0.001). There was also a statistically significant improvement in the paroxetine group: 20.7±2.4 days of headache per month prior to treatment and 14.4±1.8 days of headache per month after 6 months of therapy, р<0.01. However, the occurrence of days of headache after 6 months of therapy in paroxetine-treated patients was significantly higher than in the amitriptyline, venlafaxine, and trazodone groups. Therefore, antidepressants decrease the number of days of headache in patients with frequent episodic or chronic migraine and symptoms of depression.
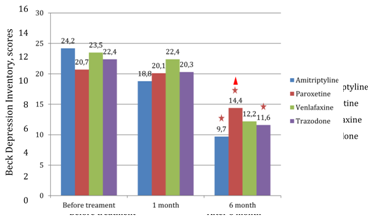
Figure 2 Effect of antidepressant therapy on the number of days of headache in patients with migraine.
∅ -p<0.01 (for differences between baseline and 6 months of treatment within a group).
Δ-p<0.01 (for differences between the numbers of days of headache after 6 months of treatment with different antidepressants).
Compliance with long-term treatment is an important aspect of antidepressant therapy. Most patients stop taking the drug within the first month, when adverse events are experienced while the antidepressant and analgesic effects are not yet properly felt (Figure 3). In particular, 25.2% of amitriptyline-treated patients discontinued their therapy within the first month. The main reasons to discontinue amitriptyline therapy were drowsiness and dry mouth, as well as a fear of taking psychoactive drugs. Paroxetine was discontinued during the first month by 20.4% of treated patients, mainly due to agitation and insomnia. In the venlafaxine group, 21.4% of subjects stopped taking the drug within the first month, mostly because of dyspepsia (nausea, diarrhoea). Only 11.8% of trazodone-treated patients discontinued the drug within the first month of treatment, in most cases as a result of drowsiness. Some patients refused therapy over the subsequent months despite being told of the need for long-term treatment. In the amitriptyline group, 17.5% of subjects discontinued their therapy, most commonly due to weight gain. Ongoing dyspepsia was the most common adverse event among patients who discontinued venlafaxine (19.1%). After the first month of therapy, trazodone (Trittico) and paroxetine were found to be well tolerated: the percentage of study subjects who had stopped taking the drug was 6.8% and 7.8%, respectively. The proportions of patients who decided to stop treatment with paroxetine or trazodone were significantly smaller than the proportions of withdrawals in the amitriptyline and venlafaxine groups (р<0.001).
Results of the reported longitudinal observational study, as well as the effect obtained with antidepressant therapy, not only with regard to the depression coexisting with migraine, but also the reduction in the number of days of headache, allow a conclusion that depression plays a key role in the progression from episodic to chronic migraine and that inclusion of antidepressant therapy in the management strategy for such patients is essential.
So what is the primary mechanism in the development of migraine–depression syndrome: is it an increasing frequency of migraine attacks and depressed mood as a response to the pain, or does a depression make the attacks more frequent? A study by Ashina Sb et al.,14 which included several thousand observations, demonstrated that depression preceded the progression to chronic migraine. What is the potential pathophysiological association between a depressive episode and an increase in the frequency of migraine attacks? According to the classical theory, the development of depression is associated with reduced levels of monoamines (serotonin, norepinephrine) in cerebral neurons.18 Function of serotonergic neurons in the periaqueductal gray is decreased, which is the main pathophysiological mechanism underlying the transformation of episodic to chronic migraine (central sensitization).19 This relationship is also demonstrated by the fact that cutaneous allodynia, a clinical correlate of central sensitization, is more frequently observed in patients with chronic migraine and depression than in individuals with chronic migraine without depression.20 Another theory that tries to explain the interrelationship between depression and the transformation to chronic migraine is the neurotrophic theory. In particular, the brain-derived neurotrophic factor (BDNF) gene polymorphism Val66Met is one of the best elucidated genetic polymorphisms responsible for the development of depression.21 Patients with depression carrying this polymorphism are more likely to suffer from chronic pain syndromes.22 It was demonstrated that the BDNF gene polymorphism is observed significantly more frequently in patients with migraine than in healthy individuals,23 and is also significantly more frequent in patients with chronic migraine than in those with episodic migraine.7
Based on the knowledge that depression is definitely a modifiable risk factor for chronic migraine15 and that it has some pathophysiological mechanisms in common with chronic migraine, screening for depression should be included in practical guidelines for the management of patients with headaches. Screening should be used both in patients with episodic migraine (primary prevention of chronic migraine) and in the follow-up of chronic migraine (secondary prevention of chronic migraine). All patients with clinically relevant depression must be administered an antidepressant at an adequate dose for a long time (6 months for a single depressive episode, 9 to 12 months for recurrent depression and dysthymia). An antidepressant should be administered even to patients in whom chronic migraine is effectively controlled by other preventive medications: topiramate, botulinum toxin type A, beta-blockers, etc., because the risk of recurring chronic headache in patients with active depression is high.
In patients with migraine combined with depression, antidepressants of several groups (TCA, SSRI, SSNRI, SRAI) are effective in decreasing the number of days of headache. The most pronounced effect was observed with the TCA amitriptyline, the smallest effect was obtained with the SSRI paroxetine. Intermediate results were achieved with the SSNRI venlafaxine and the SRAI trazodone. Trazodone (Trittico) is better tolerated compared with other antidepressants, particularly during the first few weeks of treatment.
This study had a number of limitations: the treatment assignment was not blind or placebo-controlled. Nevertheless, the obtained data reflect the real clinical use of antidepressants in the treatment of migraine.
The authors thank the subjects for their participation in this research study.
No conflict of interest. This research received no specific grant from any funding agency in the public, commercial, or not-for-profit sectors.

©2018 Azimova, et al. This is an open access article distributed under the terms of the, which permits unrestricted use, distribution, and build upon your work non-commercially.