Journal of
eISSN: 2373-6410


Case Report Volume 12 Issue 3
Department of Neurology, Doaba Hospital, India
Correspondence: Dr. Dhananjay Gupta, Department of Neurology, Doaba Hospital, Jalandhar, 144001, India , Tel 9711509505
Received: January 20, 2022 | Published: June 23, 2022
Citation: Gupta D. Isolated oculomotor palsy secondary to dyslipidemia. J Neurol Stroke. 2022;12(3):69-70. DOI: 10.15406/jnsk.2022.12.00503
Background: Oculomotor weakness is one of the common problems encountered in day-to-day practice. The most common causes include diabetes mellitus and posterior communicating artery aneurysm.
Objective: Dyslipidemia with hyper-triglyceridemia has not been previously reported as an independent cause of ischemic oculomotor palsy.
Materials and Methods: Here we report a case of pupil-sparing isolated oculomotor palsy which was found to be due to very high triglyceride levels.
Results: The patient was treated conservatively with hypo-lipidemic drugs and improved after treatment.
Keywords: Oculomotor palsy, hypertriglyceridemia, dyslipidemia, cranial nerve palsy
Keymessage: In cases of isolated oculomotor palsy, with no other apparent cause, it is worthwhile to check lipids and triglyceride levels and treat for the same.
Oculomotor nerve weakness is one of the common presentations in neuro-ophthalmology clinic. There are numerous causes of a third nerve weakness and pupillary involvement can help to differentiate benign causes like diabetes mellitus from malignant causes like Posterior communicating artery aneurysm.1–3 The most common cause of benign ischemic oculomotor palsy is uncontrolled diabetes.2 Dyslipidemia has been mentioned as an uncommon cause but there are very few cases reported in literature. We report a case of pupil-sparing complete oculomotor palsy which was found to be associated with very high triglyceride levels and improved after correction of triglyceride levels.
A 45-year-old lady, without previous co-morbidities presented with sudden onset drooping of left eyelid. She did not complain of fever, headache, weight loss or trauma. She had no previous history of migraine, other headache disorders or any head and neck surgery. On examination, patient had complete ptosis of the left lid, with eye in down and out position. Vertical eye movements and adduction in the left eye were restricted with preserved abduction (Figure 1). Bilateral pupillary reactions were normal. Rest of the neurological examination was normal. There was no weakness or ataxia of limbs. No involuntary movements of any body parts. Ophthalmoscopic examination was grossly normal.

Figure 1 5-gaze photograph of patient showing complete ptosis of left eyelid and restriction of left eye adduction, upgaze and downgaze, with relative preservation of abduction.
She was hemodynamically preserved with a blood pressure of 136/84 mmHg. She was overweight with BMI of 25.1 kg/m2. Investigations showed normal complete blood counts, normal blood sugar (106 mg%) and HbA1c levels of 5.5%. Liver, Kidney and Thyroid function were normal. Lipid profile revealed very high triglyceride levels (630 mg/dL) with borderline LDL (135 mg/dL) and normal HDL and VLDL levels. Magnetic resonance imaging (MRI) of brain was normal and angiogram ruled out any aneurysm. There was no evidence of any brainstem pathology, including stroke, demyelination or tumor on brain MRI. MRI of the orbit was normal with normal optic nerve scans. (Figure 2) A CT angiography of brain and neck vessels was done further, which was again normal. To further rule out any auto-immune cause, ANA-IF (anti-nuclear antibody, Immunofluorescence) and ANCA-panel (Anti-neutrophilic cytoplasmic antibody) were sent, which were negative.
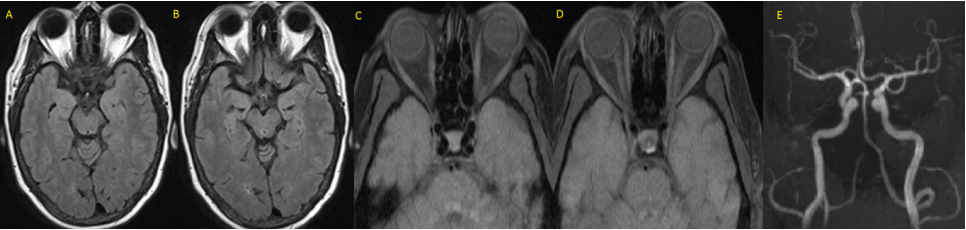
Figure 2 MRI brain (A,B axial cuts), MRI orbits (C,D) and MRI angiogram of brain (E) showing normal brain parenchyma, orbit and optic nerves. No aneurysms delineated in the angiogram.
The patient was managed conservatively with anti-inflammatory drugs and fibrates, followed by statins as per the Lipid Association of India guidelines for hypertriglyceridemia.4 On follow-up after six weeks, patient had significant improvement in ptosis and ocular movements. Her triglyceride levels reduced to 202 mg/dl.
In a population-based cohort study, the annual incidence of acquired oculomotor palsy was shown to be 4 per 100,000 population.1 The most common cause was presumed ischemic (42%) followed by trauma in 12% of patients. Diabetes mellitus and hypertension cause ischemic changes and are considered to be the most common systemic causes of acquired third nerve palsy.2 Hyperlipidemia is an important atherosclerotic risk factor and has been previously reported in Japanese and Korean cohorts of patients with oculomotor palsies.3,5 But none of these studies have reported hyperlipidemia or hyper-triglyceridmia as the independent cause.6 Hyper-triglyceridemia itself can be secondary to insulin resistance, diabetes mellitus, metabolic syndrome or other autoimmune and endocrinological diseases.
Our middle-aged, obese patient had a painless, pupil-sparing, complete oculomotor palsy without any vascular or atherosclerotic risk factors. Brainstem pathology and compressive lesions including brain aneurysms were ruled out by neuroimaging. Blood investigations revealed very high triglyceride levels, which improved after treatment with statins and fibrates. Secondary causes of hyper-triglyceridemia were excluded. In absence of any other identifiable cause and clinical improvement after hypo-lipidemic drug treatment, hypertriglyceridemia was the most probable cause in our patient. This case illustrates the need to suspect dyslipidemia and include testing for serum lipid levels in the routine work up for patients of oculomotor palsy.
None.
The author declares that there are no conflicts of interest.

©2022 Gupta. This is an open access article distributed under the terms of the, which permits unrestricted use, distribution, and build upon your work non-commercially.