Journal of
eISSN: 2373-6410


Case Report Volume 5 Issue 3
Department of Neurosurgery, Cedars Sinai Medical center, USA
Correspondence: Paula Eboli, Department of Neurosurgery, Cedars Sinai Medical center, USA
Received: October 18, 2016 | Published: November 28, 2016
Citation: Eboli P, KNezhad M, Austin M, Schlick KH, Alexander MJ (2016) First Reported Case of Mechanical Thrombectomy for Acute Ischemic Strokein an Individual with a Total Artificial Heart. J Neurol Stroke 5(3): 00181. DOI: DOI: 10.15406/jnsk.2016.05.00181
Background: With the results of recent thrombectomy trials, endovascular therapy (EVT) is standard of care in appropriately selected patients with acute ischemic stroke (AIS). We report the first case of mechanical thrombectomy for a patient supported by a total artificial heart (TAH) with AIS.
Clinical presentation: A 37 year old male patient with ischemic cardiomyopathy was found to have right gaze preference, left facial droop, and global aphasia 9 days following implantation of a TAH. Prior to ictus, antithrombotic regimen included daily aspirin and heparin infusion at therapeutic levels. Acute imaging revealed a 6 mm left M2 thrombus with associated perfusion mismatch seen in the left MCA territory along with a smaller matched perfusion defect seen in the right MCA territory.
Intervention: Following confirmation of lesion amenable to mechanical thrombectomy, patient underwent successful TICI 3 revascularization of the left MCA territory with a Solitaire stent retriever. Repeat perfusion imaging revealed resolved left MCA territory mismatch with persistent right MCA matched defect. His speech improved to an expressive aphasia following revascularization.
Conclusion: EVT has been proven to be safe and efficacious for AIS. Prior reports have demonstrated benefit for patients with concurrent mechanical circulatory support devices; however, our report is the first case demonstrating efficacy with a TAH device. Presence of mechanical circulatory support devices should not exclude EVT in individuals with AIS.
Mechanical circulatory support provides an important therapeutic intervention for those with critically depressed cardiac function. Although these devices provide a critical bridge-to-transplant along with destination therapy, ischemic stroke remains a devastating and unfortunate risk associated with these devices.Prior series have reported incidence of ischemic stroke as high as 17%, at times occurring in the perioperative period.1–3
Current management strategies aimed at preventing ischemic strokes focus on systemic anticoagulation. When an ischemic stroke does occur, these individuals are usually not candidates for intravenous thrombolytic therapy due to these factors, allowing a potential reversible ischemic event to progress to tissue infraction. Fortunately, mechanical thrombectomy does remain a viable treatment option, in select patients.4–8 Prior reports have reported individual cases of successful mechanical thrombectomy in individuals with left ventricular devices, but no such intervention has been reported with concurrent total artificial heart implantation.9,10 We report the first such case of successful mechanical thrombectomy for acute ischemic stroke in an individual with a total artificial heart.
A 39 year old gentleman with history of ischemic cardiomyopathy was transferred to our tertiary care academic medical center following presentation at an outside hospital for worsening dyspnea and chest pain. He was found to have severe 3 vessel cardiac disease and thought to be an unacceptably high risk for surgical revascularization. He was initially supported with an intra-aortic balloon pump and subsequently underwent implantation with a 70cc Syncardia Total Artificial Heart. Post-operative antithrombotic regimen included continuous heparin infusion and aspirin 81 mg daily. On post-implantation day 9 he was noted to be less responsive than his baseline, globally aphasic, with left facial droop and right gaze preference. Urgent neurologic examination demonstrated an NIHSS score of 11 for decreased mental status, gaze preference, and speech difficulties.
A non-contrast head CT did not demonstrate hemorrhage; however, intravenous rt-PA was held as PTT was elevated at 63 seconds. Further head imaging revealed a 6 mm filling defect in the left M2 branch and a smaller right M3 occlusion (Figure 1). CT Perfusion done at the time demonstrated a moderate left posterior frontoparietal area of perfusion mismatch along with a smaller right frontal area of perfusion mismatch (Figure 2).
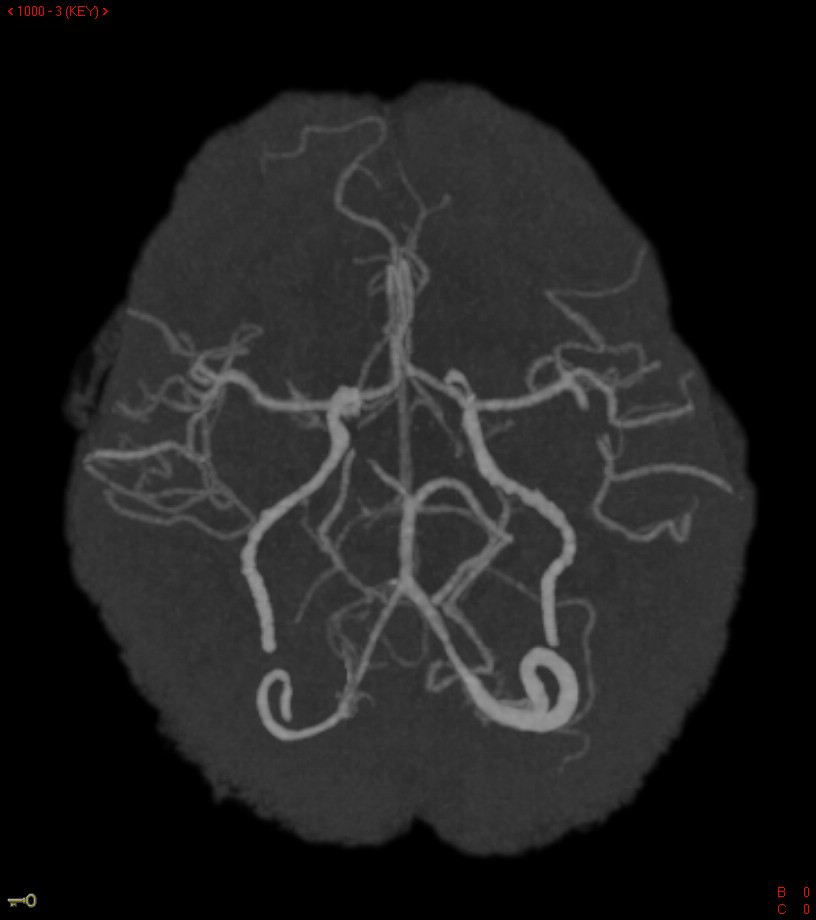
Figure 1 Reconstructed images of CT angiogram demonstrating filling defect seen in the left M2 branch of the middle cerebral artery.
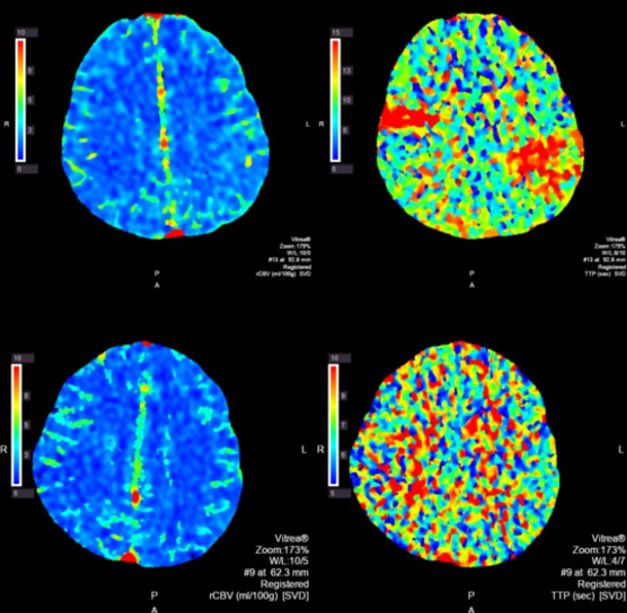
Figure 2 CT perfusion images. Top panel was done at onset of symptoms demonstrating elevated left frontoparietal elevated time to peak with relatively preserve cerebral blood flow. A smaller right MCA perfusion deficit can be seen as well. Following thrombectomy this perfusion deficit has now resolved, as seen in the bottom panel.
The patient was then taken urgently to the interventional radiology suite for mechanical thrombectomy of the left M2 thrombus. Using a 4mm x 15mm Solitaire stent-retriever TICI 3 flow was established after one pass (Figure 3). Thrombus on gross appearance appeared fibrinous. Microsopic evaluation of the thrombus showed a fibrin blood clot composed of multiple overlapping layers of fibrin admixed withplatelets, rare pools of red blood cells, and neutrophils, as can be seen in thrombus formed within 72 hours (Figure 4).
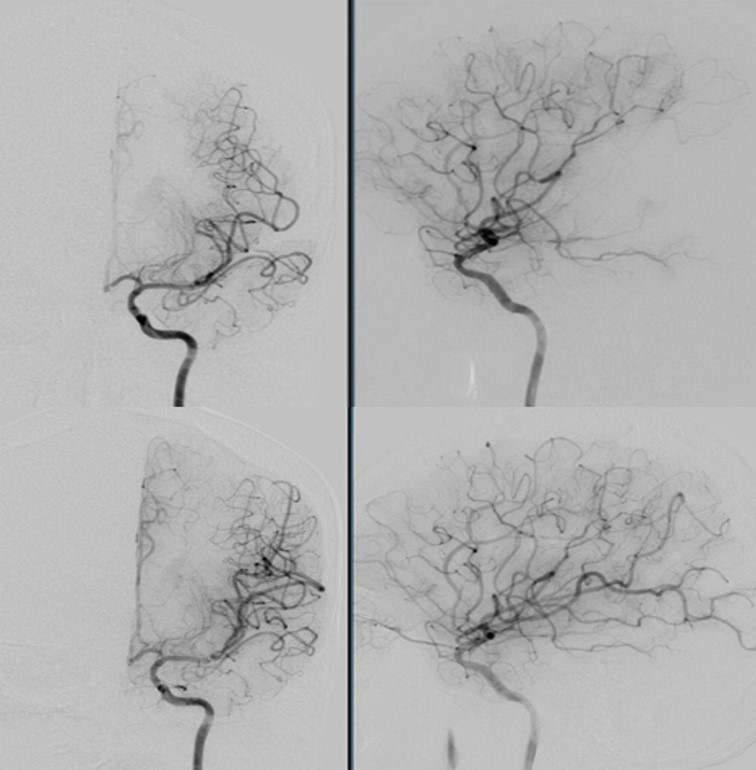
Figure 3 Cerebral angiogram in the AP and lateral views prior to mechanical thrombectomy with Solitaire stent-retriever system (top panel). Subsequent TICI 3 flow seen in the same territory following clot retrieval (bottom panel).
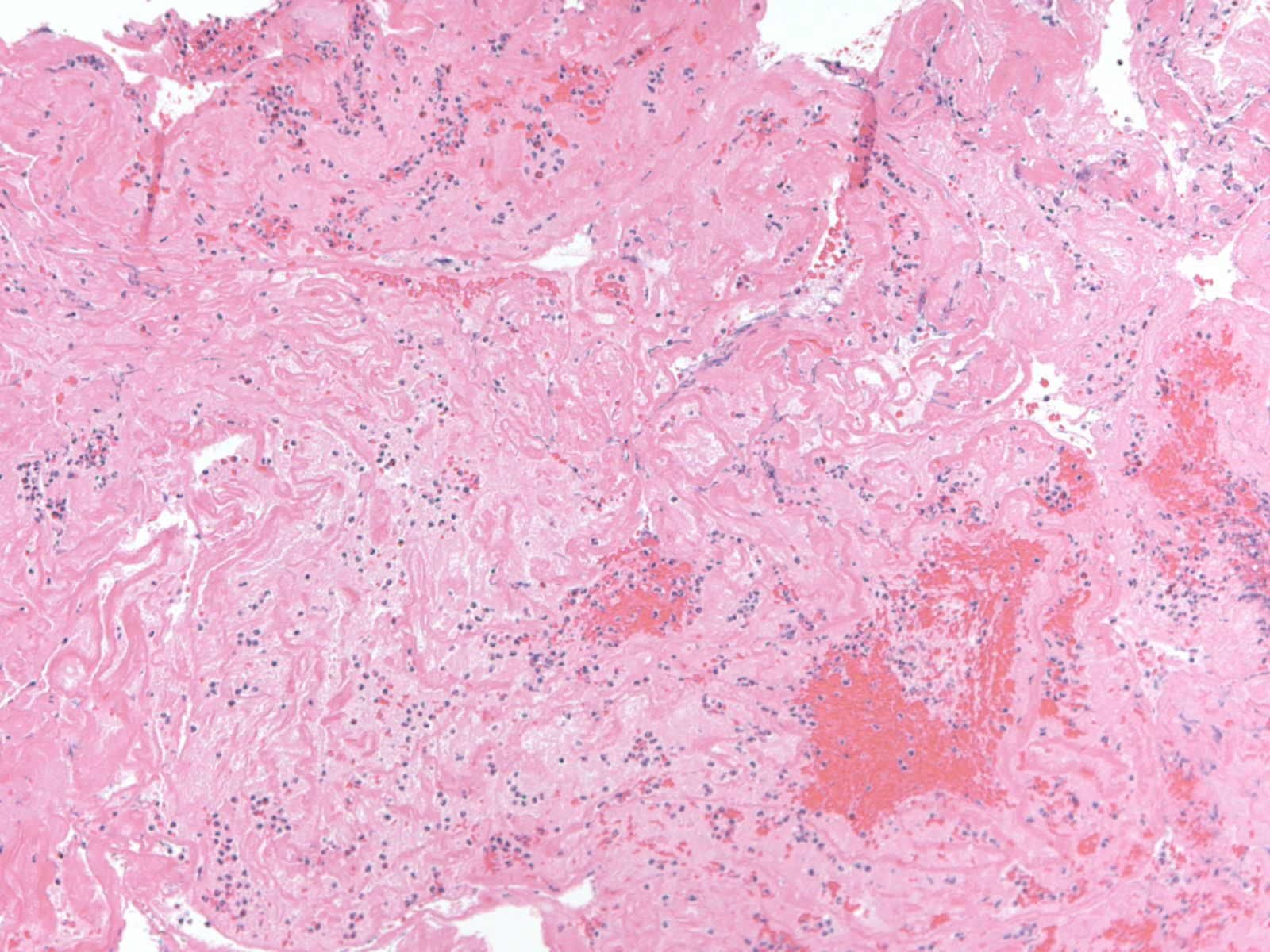
Figure 4 100x view of H&E section of aspirated thrombus. There are overlapping layers of fibrin admixed with platelets and rare pools of red blood cells admixed with neutrophils seen on this section.
Post-procedural the patient was noted to have improved somewhat with a largely expressive aphasia, continued gaze preference, and facial droop. Transcranial Doppler microeboli monitoring done post-thrombectomy day 0 revealed multiplemicroembolicsignals during 1 hour of monitoring. A repeat CT Perfusion study done on post-thrombectomy day 1 revealed resolution of left MCA territory mismatch. Unfortunately, on post-intervention day 2 the patient developed a dense left hemiplegia. CT perfusion study demonstrated a large right MCA territory matched defect. The patient was supported medically following this event with care subsequently withdrawn.
Advances in healthcare have given patients with a once dire diagnosis, such as end-stage heart failure, the opportunity to live less debilitated and more independently with the assistance of mechanical circulation devices. However, due to known acquired hypercoagulability, and other yet to be elucidated factors, these patient are at increased risk for embolic ischemic stroke.11 Current treatment paradigms rely on antiplatelet agents in conjunction with systemic anticoagulation to decrease the risk of an embolic event. However, these same treatments preclude many of these patients from intravenous thrombolytics. Thus leaving mechanical thrombectomy as the only viable treatment of acute treatment of ischemic stroke in these patients.
To our knowledge, this is the first reported case that demonstrates a technically successful mechanical thrombectomy done in a patient with a total artificial heart. The patient’s continued embolization noted on transcranial doppler and new subsequent stroke demonstrate the poor precision of our embolism prophylaxis regimens. Further studies should be pursued in developing antithrombotic management protocols in this patient population. In the interim, mechanical thrombectomy should be pursued during an acute cerebral ischemic event in the mechanical circulatory support population.
None.
The authors disclose no conflicts of interest.

©2016 Eboli, et al. This is an open access article distributed under the terms of the, which permits unrestricted use, distribution, and build upon your work non-commercially.