Journal of
eISSN: 2373-6410


Case Report Volume 12 Issue 6
1Department of pediatric Hemato-oncology and Bone marrow Transplant, St. Johns medical college, India
2Department of Neurosurgery, St. Johns medical college, India
3Department of pathology, St. Johns medical college, NIMHANS, India
4Department of radiology, St. Johns medical college, India
Correspondence: Dr. Sibhi Ganapathy MS, Mch, DNB, MNAMS, FAGE, Assistant Professor, Department of Neurosurgery, St. John’s Medical College & Hospital, Bangalore, India
Received: November 01, 2022 | Published: November 15, 2022
Citation: Jyothi M, Ganapathy S, Nivetha K, et al. Dysembryoplastic neuroepithelial tumour - a reversible cause of neuroregression in children. J Neurol Stroke. 2022;12(6):184-186 DOI: 10.15406/jnsk.2022.12.00524
Dysembryoplastic Neuroepithelial Tumour (DNET) is a rare brain tumour commonly involving the temporal lobe and presenting with intractable seizures. However, neuroregression as a presenting feature of DNET is uncommon. We report a case of a 12-year-old boy with DNET arising from the parietal lobe presenting with intractable seizures & neuroregression. The child was subjected to neurosurgical resection of the lesion following which he made a full recovery. A review after surgery showed his epilepsy under control with good progress in scholastic, social adaptive and motor skills.
This is the third report in literature of DNET surgery producing epilepsy control and reversing milestone regression. This demonstrates Epilepsy Surgery as a powerful tool in combatting neuro-regression secondary to lesional epilepsy.
Keywords: Neuroregression, brain tumors, childhood epilepsy, epilepsy surgery, DNET
Dysembryoplastic Neuroepithelial Tumour (DNET) is a rare brain tumour commonly involving the temporal lobe and presenting with intractable seizures. However, neuroregression as a presenting feature of DNET is uncommon. We report a case of a 12-year-old boy with DNET arising from the parietal lobe presenting with intractable seizures & neuroregression.
A twelve-year old boy from Nepal presented with complaints of seizures since 4 years of age followed by cognitive decline and slowing of movements since 7 years of age. Born of non-consanguineous parentage, he had no significant perinatal events and was well till 4 years of age. He developed complex partial seizures (CPS) at 4 years of age at a frequency of 1-2 episodes per year. Seizure semiology and frequency evolved over the next few years. By 12 years of age, the most predominant seizure type was focal onset - generalised tonic clonic seizures (GTCS) with occasional absences and myoclonic jerks. Also, the seizure frequency had increased to 5-6 episodes per day. For these symptoms, he received multiple Anti Epileptic Drugs (AEDS) but with no response. No imaging or electrophysiologic studies were performed.
His scholastic performance was good until 7 years of age after which there was regression in cognitive, language, social and motor milestones. Neuroregression manifested as inability to comprehend and execute multi-step commands, perform simple mathematical calculations, write simple sentences, read primary school books, draw basic shapes, play age-appropriate board games or engage in play with peers which he was previously capable of. By 12 years of age, he had difficulty in initiation of speech and slowing of speech. Receptive and expressive language skills was compatible with an age of 5 years. Also present was a delay in initiation of gross and fine motor movements associated with slowing of movements. He was incapable of running, skipping and cycling, all of which he could previously perform with ease. On examination, he was found to have bradykinesia with normal power, tone and reflexes. Rest of the systemic examination was unremarkable. Based on these findings, a possibility of neuroregression secondary to grey matter involvement was considered.
MRI study at admission revealed an ill-defined, irregular, heterogenous, nonenhancing, predominantly cortical-based bubbly appearing cystic lesion involving the right posterior parietal lobe with no perilesional edema – findings that were compatible with a diagnosis of DNET – Type 2 (Figure 1-7).1
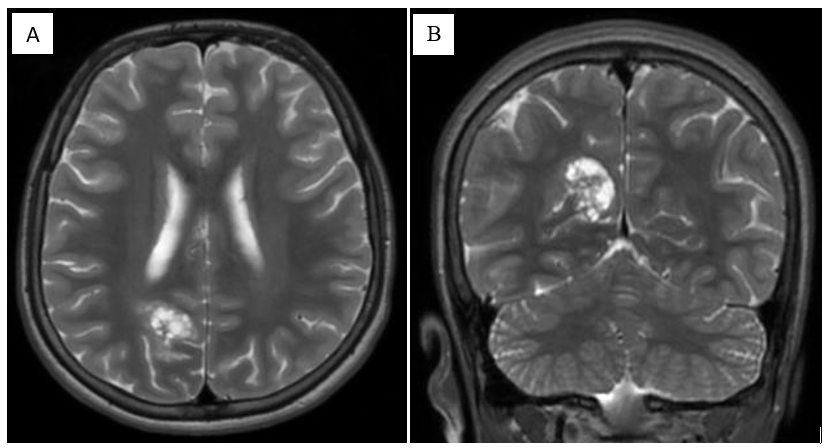
Figure 1 (A) Axial and (B) Coronal spin-echo T2-weighted MR images. MRI revealed an ill-defined, cortical-based lesion in the right medial posterior parietal lobe, which appears hyperintense with some thin internal septations. The lesion shows typical "bubbly appearance".
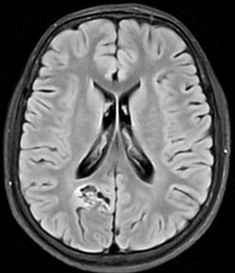
Figure 2 Axial fluid-attenuated inversion recovery (FLAIR) MR images. Lesion appears hypointense with respect to normal white matter and isointense to intraventricular CSF, with some hyperintense internal septa. A well-defined hyperintense rim separating the tumor from the surrounding normal brain is visible (arrow). This is referred to as the FLAIR hyperintense ring sign.
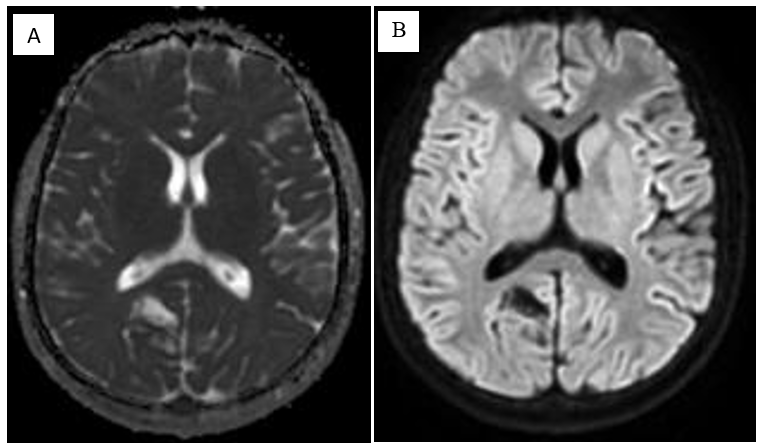
Figure 3 (A) Apparent diffusion coefficient (ADC) map and (B) Diffusion weighted images obtained through the level of lesion show high ADC values inside the lesion and low diffusion on DWI.
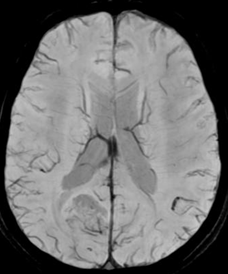
Figure 4 Axial susceptibility-weighted MR image (MIP) obtained through the level of lesion. No abnormal vessels or abnormal signal intensity are seen, suggesting the absence of calcium or blood degradation products.
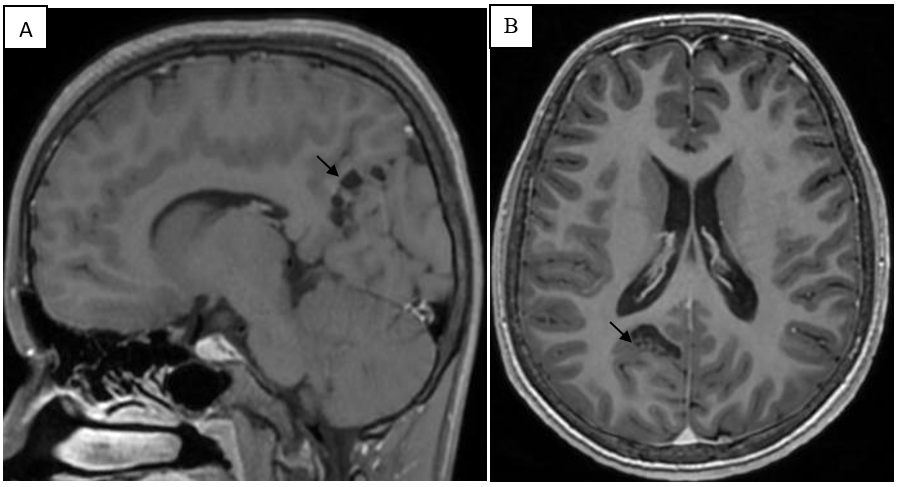
Figure 5 (A) Sagittal and (B) axial spin-echo T1-weighted MR image obtained after intravenous injection of gadolinium contrast .The lesion appears hypointense at T1-weighted imaging and has some thin septations inside it (arrow). No enhancement is noted.
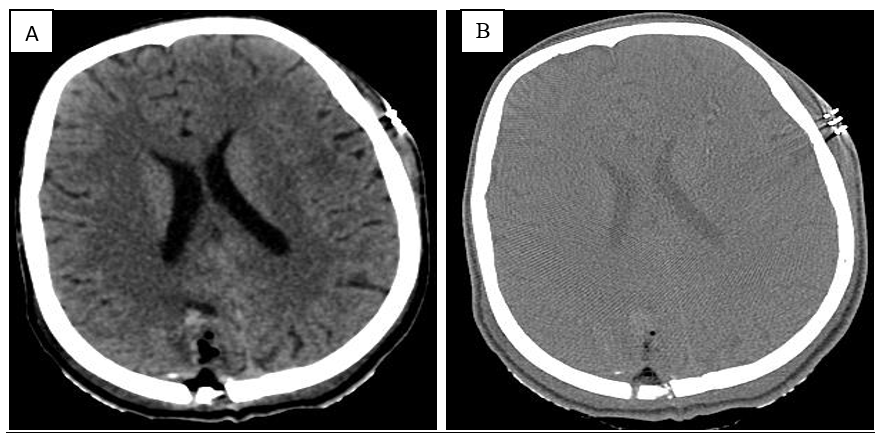
Figure 6 A) Brain window B) Bone window: Craniotomy defect noted in right parietal bone in the parasagittal region. Near complete resection of cystic mass noted. Post operative changes showing air foci and few hemorrhagic foci and minimal pneumocephalus are noted in the region of operated tumour bed.
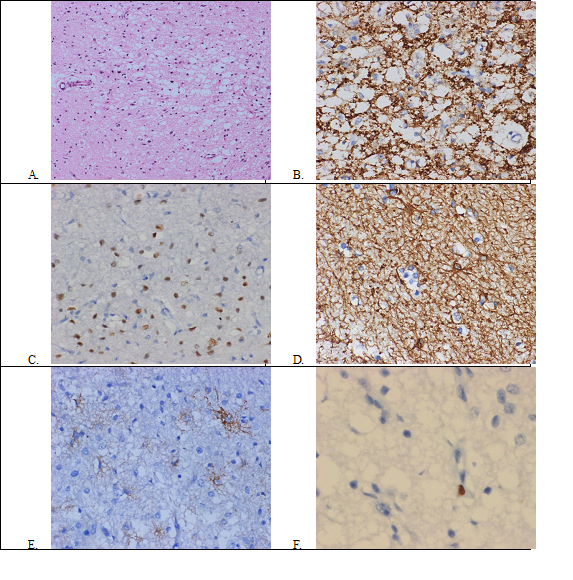
Figure 7 Histology of the tumour: A) Hematoxylin-eosin staining (20x) shows oligodendrocyte-like cells arranged in clusters embedded in a mucoid-like matrix B) Synaptophysin staining (20x) highlights neuropil C) OLIG2 staining (20x) shows nuclear positivity in the tumour cells D) Glial fibrillary acidic protein (GFAP) staining (20x) highlights stellate astrocytes around the tumour cells e) CD34 staining (20x) shows ramified glial elements in the background f) MIB1 immunolabelling (40x) highlights an occasional tumour cell.
The child underwent neuro-navigation guided right parieto-occipital minicraniotomy. The tumor was accessed through a miniscule 2cm corticectomy and followed deep almost upto the occipital horn of the lateral ventricle. The tumour was soft to firm in consistency but suckable with moderate vascularity. The solid component was interspersed with cystic spaces. Complete excision of tumour was achieved, after which the child was extubated on table without incident. Tissue biopsy revealed multinodular low – grade glioneural tumour composed of oligodendroglial like cells with small round nucleus and clear cytoplasm separated by thin capillary branching vasculature. Nodules were mostly located in cortical ribbons. No distinctive glioneural element, ganglioid cells or calcification was noted. Immunohistochemistry was positive for S-100, Olig 2, GFAP & Synaptophysin with MIBI labelling index being <1%.
Post-operatively the child had 3 episodes of seizures over the first 2 weeks. Thereafter, a dramatic response was seen with reversal of milestone regression and complete freedom from seizures. Now, I year post-op, he goes to school and is making steady progress academically, able to walk, run and talk at a normal pace, able to assist parents in domestic activities as well as take part in sport and extracurricular activities.
DNET, first described by Daumas & Duport in 1988, is a rare low grade brain tumour comprising 1.2% of all neuroepithelial tumours of childhood.2,3 Classified as neuronal and mixed neuronal-glial tumour, it is one of the most common ‘epileptogenic brain tumours’ apart from ganglioglioma, angiocentric glioma, isomorphic diffuse glioma and papillary glio-neuronal tumor.4
The mean age at presentation of DNET is 9.4 years with slight male preponderance in children. 100% present of cases present with seizures, usually pharmaco-resistant, with duration of seizures ranging from 4 months to 7 years.5 Seizure semiology can be varied and mixed with CPS (85%) being the most common type of seizure.5 Neuroregression is an uncommon feature of DNET with about 7 cases in literature so far and is often reversible following tumour resection.6,7 Other brain tumours which can present with neuroregression include low grade gliomas (2.3%) and brain tumours of infancy (35%).8,9 Surgical resection of DNET can lead to improvement in developmental milestones and reversal of regression.
Typical radiologic findings in DNET include cortically based, T1-hypointense, T2-hyperintense lesion cystic SOL with multiple internal septations (Soap – bubble appearance) in the temporal cortex (65%) or frontal lobe (30%). Other supratentorial locations like occipital lobe and parietal lobe as in our case report are rare. It typically does not exhibit mass effect or vasogenic edema.3,10
Typical histopathologic findings include Oligodendroglial-like cells (OLCs) arranged along the ramifying capillaries (perpendicular to the cortical surface) separated by the mucinous matrix in which focal microcystic change and floating neurons are seen. IHC shows GFAP + Astrocytes and synaptophysin positive neurons. Differential diagnoses include Oligoastrocytoma, pilocytic astrocytoma, oligodendroglioma, ganglioglioma.3
DNET is surgically curable without need for adjuvant chemoradiotherapy. Surgical options include lesionectomy, extended lesionectomy, partial lobectomy.5 Surgical resection of DNET can achieve freedom from seizures in 86% children and improvement in seizure control in over 98 % of children. Post-operative complications such as cognitive decline, neurological deficits and seizures are usually transient and seen in 12 % cases. Total gross resection of the lesion is the only factor predicting long-term seizure freedom. However, even with partial resection, long-term seizure free rates exceed 50 %.
Recurrence is not uncommon (17%) following gross total resection.11 Malignant transformation of DNET is a rare occurrence and risk factors for malignant progression of DNET lesions include complex-type histologic features, extratemporal location, subtotal resection, adjuvant radiotherapy, contrast enhancement and high Ki-67 labeling index.10,12
Developmental regression in the setting of intractable seizures should raise the suspicion of epileptogenic tumours such as DNET. Typical radiologic and histologic findings aid the diagnosis of this rare entity. Surgical resection forms the mainstay of therapy and can achieve excellent results in terms of seizure control as well as reversal of developmental regression.
None.
None.
The author declares no conflicts of interest.

©2022 Jyothi, et al. This is an open access article distributed under the terms of the, which permits unrestricted use, distribution, and build upon your work non-commercially.