Mini Review Volume 7 Issue 6
Basilar Artery Ischemic Syndromes- A Brief Discussion of Current Concepts
Sucharita Ray
Regret for the inconvenience: we are taking measures to prevent fraudulent form submissions by extractors and page crawlers. Please type the correct Captcha word to see email ID.

Department of Neurology, All India Institute of Medical Sciences, India
Correspondence: Sucharita Ray, Stroke fellow, Department of Neurology, All India Institute of Medical Sciences, New Delhi, India, Tel +919968968757; +919711248676
Received: March 22, 2017 | Published: November 10, 2017
Citation: Ray S (2017) Basilar Artery Ischemic Syndromes- A Brief Discussion of Current Concepts. J Neurol Stroke 7(6): 00261. DOI: 10.15406/jnsk.2017.07.00261
Download PDF
Abstract
Ischemic involvement of the basilar artery is characterized by a set of distinct symptoms characteristic of involvement of the perfused regions supplied by the basilar artery and its branches. This review discusses some of the classical concepts of basilar artery occlusion syndromes, with special emphasis on top of basilar syndrome and discuss some current concepts regarding the same.
Keywords: top of basilar, somnolence, mesencephalic artery syndrome, cogan's rule, collier sign, thrombolysis, endovascular management
Introduction
Occlusion of the basilar artery are a type of posterior circulation syndromes that present with a distinct spectrum of neurological findings affecting the visual, behavioral and oculomotor abnormalities without prominent motor dysfunction.1 Segarra coined the term 'mesencephalic artery syndrome' and used the term 'somnolent mutism' to describe it.2 Overall, occlusion of the basilar artery comprises 1% to 4% of all ischemic strokes.3 But symptoms of top of basilar are a distinct subdivision of the former and need to be properly categorized.
Top of basilar syndrome typically occurs with thromboembolic occlusions of the distal third or tip of the basilar artery. However, often clinical symptoms may result due to occlusions of more proximal segments of the basilar artery and its braches especially the posterior cerebral artery. In this review we consider the clinical characteristics of basilar artery occlusion, in particularly, the top of basilar syndrome and discuss the common clinical characteristics, imaging findings, and management strategies of the same.
The risk factors for developing the condition are hypertension, diabetes mellitus, obesity, hyperhomocystinemia and excessive alcohol intake.4 The classical top of basilar syndrome involves areas of posterior hemispheres due to posterior cerebral artery infarctions and the rostral brainstem supplied by the basilar artery. Although the clinical characteristics are quite variable depending on the pattern of involvement, it is practical to consider the clinical manifestations separately for the sake of simplicity.
Symptoms of Posterior cerebral artery territory
- Unilateral infarctions
- Visual deficits: A homonymous hemianopia can occur due to a lesion anywhere along the visual radiation. Occasionally, patients with lesions limited to calcarine cortex may be able to retain some partial vision and identify colors, nature or size of an object within the 'blind field'. Optokinetic nystagmus is preserved (Cogan's rule). Scintillations may occur at the edge of the hemianopic field either during presentation or during clearing of the symptoms. Patients may also report perseveration of visual images presented to them either in the center of visual fields or when presented repeatedly towards the hemianopic side. Awareness of deficits is the rule, in contrast to lesions of the middle cerebral artery.
- Behavioral defects: Several behavioral manifestations like anomic aphasia, alexia without agraphia, temporary Korsakoff-like amnestic syndrome,or visual agnosia may accompany left occipital infarctions. Right occipital infarctions have been associated with the Charcot-Wilbrand syndrome of defective revisualization and absence of visual dreaming and aprosopagnosia which is classically associated with bilateral infarctions.1
- Bilateral infarctions: Cortical blindness is the most severe visual defect caused by bilateral occipital infarctions. Balint syndrome can occur due to infarct of bilateral posterior cerebral arteries and consist of asimultagnosia, optic apraxia, apraxia of gaze and metamorphosia. Memory deficits, agitated delirium and a temporary Korsakoff-like syndrome may also occur that usually lasts few hours but may extend for upto 6 months. In fact, patients with bilateral infarctions of posterior cerebral arteries often mimic delirium tremens due to their agitated and hyperactive behavior.
- Motor and sensory defects: Sensory loss is more than motor deficits in patients with posterior cerebral artery territory infarctions. Somatosensory deafferentation with severe loss of touch, position and proprioception with appreciation of pain may also occur. Testing of motor power in outstretched hands with severe sensory loss exhibits levitation in contrast to downward drift due to predominant sensory deafferentation over pyramidal weakness. Lesions of the ventroposterior-lateral nucleus of the thalamus cause pure sensory stroke without any significant objectively demonstrable loss of perception. In contrast, patients with lesions limited to the lateral thalamus usually do not have severe deafferentation.
In contrast to the sensory deficits, motor paralysis is uncommon with occlusion of the posterior cerebral artery and patients usually retain their ability to make fine distal movements in limbs the absence of hyperreflexia, clonus or bilateral Babinski signs. Occasional involvement of the cerebral peduncles may cause hemiplegia in addition to the usual hemianopia and hemisensory loss.
- Symptoms of Rostral brainstem: Involvement of the rostral brainstem causes symptoms affecting both visual as well as behavioral systems.
- Visual abnormalities: There is abolition of voluntary or reflex vertical gaze (as tested by oculocephalic and caloric maneuvers and Bell phenomenon). Isolated paralysis of upward or downward gaze occurs less frequently. In addition, hyperconvergence or convergence spasm maybe seen on attempting conjugate lateral or vertical gaze. Convergence retraction nystagmus can be elicited by asking the patient to fix on an optokinetic stimulus moving upward. A pseudosixth sign consisting of failure of ocular abduction maybe seen with eyes resting in a hyperconvergent fashion. This phenomenon is so named because it does not occur due to the dysfunction of the sixth nerve Unilateral or bilateral Collier sign (elevation and retraction of the upper eyelids) may accompany sudden darting or lightning like oscillations of the eyes. Skew deviation of eyes may reflect lesions of the middle cerebellar peduncle and medulla. Internuclear ophthalmoplegia can occur rarely subsequent to involvement of midbrain tegmentum ventral to the aqueduct.
Pupils may remain small and show transient light response or maybe positioned eccentrically (corectopia iridis) and often, this shift is also seen transiently.
- Behavioral abnormalities: Rostral medial reticular formation due to occlusion of the mesencephalic artery can cause sleepiness, apathy and lack of attention to the environment. These findings, famously called somnolent mutism by Segarra needs to be contrasted with the coma vigil of patients with bilateral cerebral lesions. Vivid and well-formed hallucinations may occur without visual field defects but are usually rare in patients with high brainstem infarctions. When they do occur, they are realistic, involving familiar people and surroundings and may last several minutes. These have been famously called peduncular hallucinosis by van Bogaert and characteristically represent lesions of the midbrain and not the cerebral peduncles, as is suspected.
- Symptomatic progression of symptoms: Top of basilar syndrome represents a distinct subset of posterior circulation syndrome which can present with a prolonged latency between first prodromal symptoms and typical clinical characteristics to develop. Herald hemiparesis can also occur as a transient, lateralized motor weakness that may precede the onset of stroke.
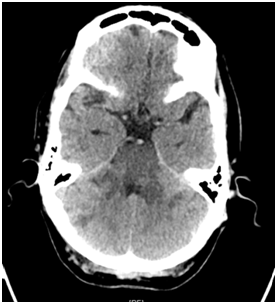
- Radiology: The pattern of infarcts follows the level of involvement of the unpaired basilar artery and its branches. Sixteen patients with demonstrated top of the basilar syndrome found infarcts distributed between the thalamus, midbrain, pons, cerebellum, and occipital lobe. Bilateral thalami were seen to be involved in seven cases. CT evidene of a hyperdense basilar artery usually demonstrates a filling defect on angiography confirming the site of occlusion5 (Figures 1a, 1b & 2).
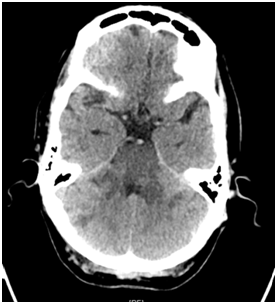
Figure 1a Hypodensity in the brainstem and adjoining superior cerebellar peduncle, with dense basilar sign.

Figure 1b Hypodensity in the brainstem, bilateral cerebellar hemispheres, evidence of obstructive hydrocephalus, suggestive of basilar artery thrombosis.

Figure 2 CT Angiography showing nonvisualization of the basilar artery and posterior cerebral artery.
Management strategies and clinical outcome of basilar artery occlusion
Management of top of basilar artery syndrome is similar to the strategy for managing vascular occlusions of the vertebrobasilar systems. Earlier, high rates of mortality of around 80% were encountered with conventional treatment for posterior circulation territories.6 Spontaneous recanalization of the occluded artery can occur in upto 61.5%, concordant with an embolic origin of the syndrome.7 Compared with basilar occlusion, basilar embolism has a relatively low mortality and the outcome is frequently excellent.8 However, mortality rates are high in patients who undergo conventional treatment with antiplatelet agents, require mechanical ventilation or present with ocular palsies or obtnded sensorium.4,9
Timelines for thrombolysis have not been well defined for vertebrobasilar system as they have been described for anterior circulation. Efficacy of delayed intra-arterial thrombolysis have been described in basilar artery occlusion even upto 12 hours after symptom onset.9 A similar study using intraarterial urokinase in 24 patients with symptomatic basilar thrombosis has found better neurologic outcomes in patients who had collateral filling of the basilar artery. Distal clot location was the single best predictor of survival after basilar thrombosis and intraarterial Thrombolysis.10 Endovascular thrombectomy has further improved patient outcomes with similar rates of recanalization of posterior circulation strokes as compared to the anterior circulation.11 One of the largest series on basilar artery occlusion has shown mortality rates of 41% with present management strategies which is a remarkable improvement from previous rates of mortality. Age, absent or minimal recanalization and presence of symptomatic intracranial hemorrhage were independently associated with fatal outcome.12
Conclusion
The review discusses some of the classical as well as contemporary lines of thought on the management of ischemic basilar artery syndromes. The condition requires judicious identification of the clinical signs and aggressive management strategies to counter the otherwise uncertain guidelines on best medical care. Therapeutic decisions must be individualized to circumvent the otherwise poor outcome and improve clinical prognosis in this rare and dreaded subgroup of posterior circulation ischemic syndromes.
Acknowledgments
Funding
Conflicts of interest
The author has no declarations or conflict of interest. There are no financial disclosures to be made.
References
- Caplan LR. Top of the basilar syndrome. Neurology. 1980;30(1):72˗79.
- Segarra JM. Cerebral Vascular Disease and Behavior: The Syndrome of the Mesencephalic Artery (Basilar Artery Bifurcation). Arch Neurol. 1970;22(5):408˗418.
- Demel SL, Broderick JP. Basilar Occlusion Syndromes. The Neurohospitalist. 2015;5(3):142˗150.
- Suthar PP, Rana PJ, Mehta C, et al. Top of Basilar Artery Syndrome. J Clin Diagn Res JCDR. 2015; 9(7):TJ01.
- Barkhof F, Valk J. “Top of the basilar” syndrome: a comparison of clinical and MR findings. Neuroradiology. 1988;30(4):293˗298.
- Schonewille W, Algra A, Serena J, et al. Outcome in patients with basilar artery occlusion treated conventionally. J Neurol Neurosurg Psychiatry. 2005;76(9):1238˗1241.
- Sato M, Tanaka S, Kohama A. “Top of the basilar” syndrome: clinico-radiological evaluation. Neuroradiology. 1987;29(4):354˗359.
- Schwarz S, Egelhof T, Schwab S, et al. Basilar artery embolism. Clinical syndrome and neuroradiologic patterns in patients without permanent occlusion of the basilar artery. Neurology. 1997;49(5):1346˗1352.
- Wijdicks EFM, Scott JP. Outcome in Patients With Acute Basilar Artery Occlusion Requiring Mechanical Ventilation. Stroke. 1996;27(8):1301˗1303.
- Cross DT, Moran CJ, Akins PT, et al. Relationship between clot location and outcome after basilar artery thrombolysis. AJNR Am J Neuroradiol . 1997;18(7):1221˗1228.
- Smith WS, Sung G, Starkman S, et al. Safety and efficacy of mechanical embolectomy in acute ischemic stroke: results of the MERCI trial. Stroke. 2005;36(7):1432˗1438.
- Sairanen T, Strbian D, Soinne L, et al. Intravenous thrombolysis of basilar artery occlusion: predictors of recanalization and outcome. Stroke. 2011;42(8):2175˗2179.

©2017 Ray. This is an open access article distributed under the terms of the,
which
permits unrestricted use, distribution, and build upon your work non-commercially.