Journal of
eISSN: 2373-6410


Case Report Volume 4 Issue 6
1Fundaci
2Philippine Heart Center, Philippines
Correspondence: Carlos Andres Clavijo Prado MD, Fundación Universitaria Ciencias de la Salud- Hospital San José, Cra 18, Bogota, Colombia, Tel 573218174635
Received: April 08, 2016 | Published: June 28, 2016
Citation: Prado CAC, Reina LFH, Adarna LG (2016) Septic Embolism: The Importance of an Adequate Clinical Approach: A Case Report, Bogota,Colombia. J Neurol Stroke 4(6): 00159. DOI: 10.15406/jnsk.2016.04.00159
Neurological complications of infectious endocarditis have a high prevalence globally and its clinical presentation remains a clinical challenge.
A previously healthy 36-year old male presented at the emergency room with persistent fever and headache. The patient was referred to Neurology section after initial diagnostics and treatment. They detected abnormal skin lesions and cardiac murmur. Based on the presentation and abnormal physical examination findings, their impression was an embolic process with infectious etiology prompting medical treatment. Patient was concomitantly referred to Cardiology section and infective endocarditis was confirmed by echocardiogram. Cranial Magnetic Resonance Imaging (MRI) confirmed an ischemic embolic process. Successful surgical treatment followed.
This highlights the importance of good clinical history and physical examination as the cornerstone of diagnosis, even for the clinically challenging cases. Good clinical approach and appropriate use of imaging technology greatly benefited the patient by allowing early diagnosis and treatment hence prevention of further complications.
Keywords:Infectious endocarditis, Cerebrovascular complications, Septic embolism, Magnetic Resonance Imaging (MRI)
MRI, Magnetic Resonance Imaging; CVAs, Cerebrovascular Accident; HIV, Human Immunodeficiency Virus; ELISA, Enzyme Linked Immunosorbent Assay; VDRL, Venereal Disease Research Laboratory; CT, Computerized Tomography; MOCA; Montreal Cognitive Assessment; FLAIR, Fluid Attenuated Inversion Recovery; ADC, Apparent Diffusion Coefficient; BP, Blood Pressure; mm Hg, millimeters of Mercury; CR, Cardiac Rate; BPM, Beats per minute; RR, Respiratory Rate; CPM, Cycles per minute
Infective endocarditis has a high mortality rate, reaching 20% worldwide. This rate is substantially different to the Colombian national mortality rate of 16.3%.1,2 This clinical condition has been established most often in the young with a mean age of 36.3 years. Eighty-four (84%) percent of the patients exhibit systemic infectious processes, with a 35% rate of misdiagnosis. The most common symptoms are fever (88%), chills (47.8%), anorexia (43.4%), dyspnea (39.1%), headache (31.5%), and arthralgia-myalgia (30.4%).2
Ischemic brain lesions of embolic origin are the most frequent neurological complications and up to 72% of these patients have minimal clinical neurological manifestations.2 This statistic exceeds that reported in the literature wherein this kind of presentation reaches only 49%. Most of these cases are incidental findings during the search for infection, which are mostly seen in patients with valvular vegetation confirmed by echocardiography. There is greater involvement of the mitral valve and followed by the aortic valve.3
In the world series, there is a high correlation between the size of the vegetation and neurological complications, resulting to cerebrovascular attacks (CVAs). It could be ischemic at 77% or hemorrhagic at 13%.3-6
Cardiac surgery within 3-60 days is indicated to reduce the risk of new embolism. However, if the patient has life-threatening conditions such as intractable heart failure or uncontrollable sepsis, surgery should be done as soon as possible. When surgery was performed after the occurrence of the adverse event, the mortality rate reaches as high as 80%, compared to 10% when surgery was done prior to complications.7 There are other risk factors listed in literature that worsens outcome in Infective Endocarditis patients with neurologic complications, and these include kidney failure, diabetes mellitus, mycotic aneurysm and infection caused by staphylococcus sp. Thus early surgery (within 2 weeks) should be considered in these subset of patients. However, in cases of hemorrhagic CVA, surgery must be done after 30 days due to the increased mortality rate if early surgery will be performed.1,7,8
The neurologic evaluation must be based on good clinical history and complete physical examination to arrive at the best diagnosis and give way to adequate and necessary clinic-radiological correlation.9
The patient is a 36-year old male from Bogota, Colombia, an electrician, without significant epidemiological or exposure history who presented with clinical symptoms evolving for three weeks characterized by fatigue, weakness, fever of 38-39 degrees Celsius with morning predominance associated with diaphoresis, chills, non-productive cough and episodic headache which worsened during the last week. Headache was described as needle like pain with moderate intensity, lasting for 2 hours with maximum intensity at around 30 minutes without signs of intracranial hypertension. He also reported recently an appearance of petechiae in the anterior and posterior region of the thorax, hemorrhagic splinter lesions in the nailbeds and choluria.
The patient was initially assessed by emergency medicine service. Tropical diseases were ruled out. Several examinations such as Blood Culture, dengue titer, leptospiral test, HIV ELISA and VDRL serology were all negative. A Central Nervous System infection was entertained and a cranial CT scan was requested, which was interpreted as normal. The initial plan was to do a lumbar puncture.
He was referred to the Neurology for evaluation and management. On general physical examination, vital signs were as follows, BP 120/50 mm Hg, CR of 88 BPM, RR of 22 CPM, febrile at 38 degrees Celsius. Petechiae in the anterior and posterior thorax and splinter hemorrhages in the nailbeds were appreciated. There was no jugular vein distention; lung examination revealed no rales, nor wheezes. A systolic murmur at the mitral position consistent with mitral regurgitation was noted. The rest of the physical examination were normal. Neurologic examination only showed slight alteration in immediate and procedural memory as documented in his test performance of Montreal Cognitive Assessment (MOCA) test.
Hence their impression was an embolic process secondary to infective endocarditis prompting them to start intravenous antibiotics as per institutional protocol. A transesophageal echocardiogram was requested and a concomitant referral to Cardiology service was done.
Although the initial CT scan done was initially reported as normal, neurology service reviewed the images and found a small hypodense cortico- subcortical area in the left parietal lobe (Figure 1A & 1B). Due to this finding, a cranial MRI was done which showed multiple areas of diffusion restriction which did not follow a vascular territory, whether supra or infra tentorial (Figure 2).
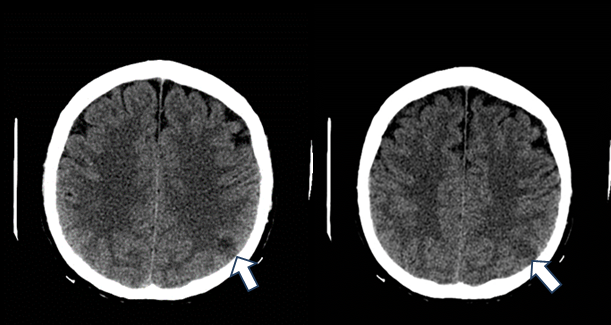
Figure 1 Simple axial tomography shows a hypodense lesion in the cortical and subcortical layer of the left parietal area.
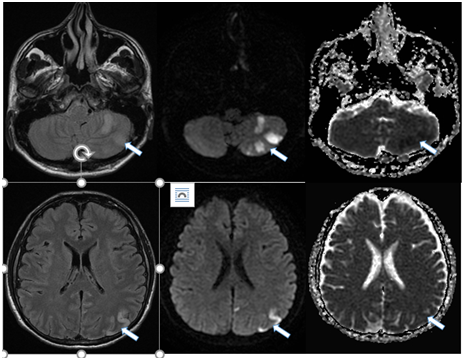
Figure 2 A,B,C Axial images. FLAIR Diffusion and ADC. Restriction zones in the left cerebellar area; D,E,F. Flair diffusion and ADC respectively. Restriction zones in the left parietal distribution.
A transesophageal echocardiogram was performed which revealed multiple vegetation attached to the posterior leaflet of the mitral valve measuring 12mm x 18mm in its largest diameter, causing severe mitral regurgitation (Figure 3). The suspected diagnosis of septic embolism with secondary stroke due to infective endocarditis was confirmed.
During his course of medical treatment, the patient developed heart failure. Our patient has confirmed infective endocarditis complicating with septic embolism and heart failure but without contraindications to surgery; he then underwent mechanical prosthetic valve replacement. Intraoperatively, there was an atrial septal defect which was corrected as well. The patient tolerated the surgery well and did not develop new neurological complications.
The rest of the hospital stay was unremarkable without deterioration of his functional class. Neurologic examination showed no development of new neurological sequelae. Blood cultures obtained at the end of his hospitalization were all negative. He was discharged stable.
With this case report, we wanted to demonstrate the importance of the clinical approach from the perspective of good medical practice entrenched in semiotics in order to establish accurate diagnosis of a disease process. Although there are scenarios where technology plays vital roles, it should not dictate the fate of the patients.
The combined work of neurology, emergency medicine and other specialties in addition with the rational use of technology greatly benefited the patient.
The diagnosis of infective endocarditis appears, apparently easy, but it is challenging since it presents with unclear clinical manifestations and 35% of affected patients are blood culture negative.2
This reaffirms once again the importance of good medical history and physical examination, which allows us to arrive at an appropriate diagnosis, to choose an adequate diagnostic procedure and to provide better patient therapeutic opportunities. In our case, cerebral magnetic resonance was very useful, although the initial indication was not clear. The findings in T2, FLAIR and ADC sequences became the cornerstone for supporting the final diagnosis, which was based on a good history and examination.
A clinical suspicion achieved after an appropriate medical history and physical examination accompanied by a thorough neurological examination allows early diagnosis of septic cerebral thrombosis. However, the new radiation techniques rendered great help; allowing timely intervention with medical treatment and planning for early valve replacement. This strategy reduced occurrence of possible complications such as new septic embolic and multiple-organ failure as documented in the literature.
Septic cortical thrombosis represents one of the most common neurological complications. There are reports that as high as 72% of these patients present with minimal clinical manifestations. This statistic exceeds that reported in the literature wherein this kind of presentation reaches 49%.3 There are varied findings in the literature with regards to the characteristics of the vegetation that makes it prone to embolization. A size of greater than 1cm or 1.5cm and even 3cm in some studies, mobile vegetation, left sided valve involvement (mitral, especially anterior mitral valve >aortic), and endocarditis caused by Staphylococcus aureus, Enterococcus bacteria (HACEK group), fungal infection and Streptococcus bovis are some of the red flags for embolism.3-5,8,10,11 In one study, Staphylococcus aureus as the pathologic agent is the most important risk factor.3 Patients are also at higher risk for embolism before the initiation of antimicrobial therapy.10 Although the risk of embolism still remains high even with one week of antimicrobial treatment if the vegetation size is ≥3cm.3 Our patient has risk factors for embolism since he had mobile, multiple and large vegetation measuring 12mm x 18mm in its largest diameter which were attached to the mitral valve. As noted in the literature, he also presented with embolism prior to initiation of antimicrobial therapy. The pathologic agent in his case was not documented since he was blood culture negative.
Epidemiological data of this pathology in our local setting is not very far from that described in the literature, with a mortality rate of 20% worldwide and 16.3% national mortality rate in Colombia.1,2
Considering the inherent consequences of the vascular territory that are detrimental to the quality of life of these patients, technology should only confirm our hypothesis and should not replace the clinician but should only be an ally to confirm our hypothesis.
None.
There is no conflict of interest among the authors in relation to the article.

©2016 Prado, et al. This is an open access article distributed under the terms of the, which permits unrestricted use, distribution, and build upon your work non-commercially.