Journal of
eISSN: 2373-6410


Research Article Volume 2 Issue 3
1Department of Neurosurgery, Assiut University, Egypt
2Department of Radiotherapy and Nuclear Medicine, Assiut University, Egypt
3Department of Radiology, Faculty of Medicine, Assiut University, Egypt
Correspondence: Hassan MH, MD, Faculty of medicine, Department of Neurosurgery, Assiut University Hospital, Assiut, Egypt, Tel 201003416033
Received: December 17, 2014 | Published: June 9, 2015
Citation: Hassan MH, Roshdy AE, Mohammad T, et al. The additive value of radionuclide shuntogram to computed tomography in evaluation of CSF shunts. J Neurol Stroke. 2015;2(3):55-59. DOI: 10.15406/jnsk.2015.02.00055
Background: Placement of cerebrospinal fluid diversions or shunts, is a common neurosurgical procedure indicated for a wide spectrum of conditions impeding the normal flow of cerebrospinal fluid (CSF). The most common systems employed are ventriculoperitoneal, ventriculoatrial and lumboperitoneal shunts. Management of patients with surgically treated hydrocephalus may be challenging, as the clinical presentation of a malfunctioning shunt is often nonspecific, especially in young children. Moreover, conventional radiological examinations, such as shunt series, cerebral ultrasound or CT scans, are sometimes equivocal in diagnosing cases of shunt malfunction, also in determining the site of obstruction. Thus, numerous procedures have been proposed to ascertain shunt function, and localize site of obstruction. Injection of contrast media and radionuclide directly into the shunt device into the lateral ventricles is one of the most common techniques employed, to assist in evaluating shunt function.
Patients and methods: A prospective study of 20 patients with suspected shunt malfunction. Their age, sex distribution, clinical presentations, and causes of hydrocephalus were recorded. We evaluated shunt function using CT brain and Radionuclide shuntogram. Shunt malfunction was evaluated by using CT-Brain only, Shuntogram only, and by combining both techniques. We evaluated these techniques regarding their results, dividing them into positive and negative cases, and establishing true and false results by following clinical progression and operative findings. After calculating sensitivity, specificity, predictive values and accuracy of the individual techniques, we determined the added value of combining shuntogram to CT-Brain in diagnosing shunt malfunction.
Results: Patients were verified into 15 males (75%) and 5 females (25%), the average age was 5.8 years. In evaluation using CT brain only, the results were 19 true positive results (95%), one case with false positive result (5%) and no negative cases (100% sensitivity and 95% accuracy). In Radionuclide shuntogram, results were: 18 true positive studies (90%); one true negative study (5%), one false negative study (5%) and no false positive results (94.73% sensitivity and 95% accuracy). The combined results of CT brain and Radionuclide shuntogram were 18 true positive cases (where both tests showed positive obstruction), no negative cases, and 2 cases with conflicting results (100% sensitivity and 100% accuracy). The sites of true positive cases verified into 13 distal blocks (65%), 5 proximal blocks (25%) and one case with combined proximal and distal blocks (5%).
Conclusion: In adding shuntogram to CT-Brain, the sensitivity and accuracy for diagnosis of shunt obstruction increased. Its advantage over other methods lies in not only diagnosing shunt malfunction but also localizing and qualifying the malfunction, thus aiding the neurosurgeon in targeting the part of the shunt requiring revision. Because of its limitation (time and costs involved in shuntogram technique), it’s not used routinely in clinical practice. But, when used in selected cases, it can help avoid unnecessary surgical intervention.
Keywords:Ventriculoperitoneal or ventriculoatrial shunt malfunction, Radionuclide shuntogram
Ventriculoperitoneal shunt is the standard operation for hydrocephalus but can be followed by complications such as mechanical malfunction and infection. Shunt malfunction and occlusion are the most common shunt complications especially in the pediatric hydrocephalic population; accounts for approximately 50% of all shunt failures.1
Determining shunt malfunction and site of obstruction is one of the clinical problems facing neurosurgeons, as it’s not always straightforward. Although most patients with a malfunctioning shunt have the classic features of increased ICP (headache, vomiting, and papilledema), in 20% of the cases the clinical presentations are atypical. In these situations, symptoms of shunt malfunction may be difficult to interpret. Likewise, asymptomatic shunt obstruction can take place in children who has developed shunt independence. Furthermore, clinical evaluation of the child or reliance on the characteristics of valve pumping may be correct in only about 50% of cases.2
A variety of techniques have been described to evaluate cerebrospinal fluid shunt function, but there is still a lot of controversy as to which method is the most convenient and accurate. Shunt pumping is simple but will usually only detect near complete obstruction, and there is considerable inter-observer variation of interpretation. Also Shunt pumping has a positive predictive value of only 20%.3
Computed tomography (CT Brain) can confirm a malfunctioning shunt, but many patients with longstanding shunt have altered brain compliance and may not show dilatation of the ventricles at presentation.3 Features of shunt malfunction include ventriculomegaly, flattening of sulci, and periventricular white matter signal changes, but they are not always present with shunt dysfunction. Also, Ophthalmic signs caused by increased ICP but without radiological signs have been reported.4 Even in the post-operative settings, non-regression of ventricular size, as evaluated by computed tomography, is an anatomic evaluation and cannot measure shunt function directly.
The injection of radionucleotide into the reservoir of a shunt ("Shuntogram") has been recommended as an investigation of the patency of both the proximal and distal shunt catheters and the integrity of the valve mechanism assuming that the reservoir lies proximal to the shunt valve. The most precise and reliable evaluations of CSF flow have been obtained by radionuclide methods.5 Diagnostic accuracy can be greatly improved by shuntography, since both anatomical and functional information can be obtained.6
Shuntograms have been introduced to assess shunt patency when clinical and other neuroimaging studies cannot ascertain a shunt malfunction requiring surgical correction. Both iodinated contrast material and radiotracers have been used for this purpose. The latter are more popular and very small volumes are required to perform the procedure. Different types of radionuclides have been used: Iodine 131 (131I) serum albumin (RISA131) was introduced in 1959, technetium 99m (99mTC)-DTPA in 1966, and indium 111 (111IN)-DTPA in 1973. 99mTC- DTPA is the radionuclide of choice for shuntogram studies. It is injected into the shunt reservoir and followed along its passage through the shunt. Both proximal and distal shunt patency can be established, especially when clinical symptomatology and standard neuroimaging i.e. computed tomography (CT) have not been conclusive in suggesting a shunt malfunction.
However, Shuntograms have been reported to have false-negative rates ranging 2-36%.7 Also it has been observed that sensitivity was increased with CT and CSF shuntogram compared with CT alone.8
This study was conducted, over a period of 2 years, in the department of Neurosurgery, Assiut University Hospital, Assiut- Egypt. It included 20 patients who previously treated with CSF shunt procedures of various types (ventriculoperitoneal, ventriculoatrial) and was complaining of symptoms and signs suggestive of CSF shunt obstruction. They comprised 15 male and 5 female patients.
Full history and clinical examination were done for each patient. CT brain and radionuclide shuntograms were done to confirm the diagnosis of CSF shunt obstruction.
Technique of radionuclide shuntogram
The patients were placed in the supine position with the head turned away from the shunt site. The scalp overlying the valve is slightly shaved, the area sterilized using Betadine and a small sterile drape applied. The reservoir portion of the valve is punctured with a 25 gauge needle without distal compression. Return of cerebrospinal fluid (CSF) into the needle hub is considered an indication of a correct puncture and ventricular catheter patency. There is no attempt to actively withdraw any CSF. A syringe containing 1ml of 99mTC-DTPA (equivalent to 37 MBq), with an average volume of 0.5ml is then inserted into the needle hub and the radiotracer injected. The tracer was imaged by a gamma camera every 30s and the tracer followed along its path down the shunt. The patients were kept in the same position; the time of peritoneal spillage is recorded. If there was no peritoneal spill noted at 20 min, the patients were allowed to sit for 5 minutes and reimaged. This repositioning procedure may be repeated, then we observe whether peritoneal spillage occurred or not.
Interpretation
Shuntogram were either categorized as normal or abnormal. In normal shuntogram, spontaneous appearance of CSF occurs within the needle hub and peritoneal spillage within 20 min, otherwise it’s abnormal (positive shuntogram) i.e., shunt obstruction or malfunction.
Depending on the results, the designations of false negative, true negative, true positive or false positive were applied. In a false negative result, the shuntogram was reported as normal; but clinical symptoms persisted and shunt malfunction was identified during surgery. In true negative result, the symptoms subsided spontaneously or confirmed not to be shunt-related after normal shuntogram. True positive category was used if shuntogram demonstrated a shunt malfunction, and was confirmed by surgery and postoperative improvement occurred. False positive result was in a group of patients that demonstrated a positive (abnormal) shuntogram that improved spontaneously and surgery was never performed.
After obtaining the results, we calculated sensitivity, specificity, predictive values (positive and negative), and accuracy. We used the following formulas for these parameters:
Sensitivity = True Positives / (True Positives + False Negatives)
Specificity = True Negatives / (True Negatives + False Positives)
Positive Predictive value = True Positives / (True Positives + False Positives)
Negative Predictive value = True Negatives / (True Negatives + False Negatives)
Accuracy = (True Positives + True Negatives) / (All Positives + All Negatives)
Then we compared these parameters in using CT-Brain and Shuntogram separately, and when combining them. Thus, determining if any advantage obtained from this combination.
Age and Sex distribution
The study involved 20 patients, verified into 15 males (75%) and 5 females (25%) with ventricular shunt and presented with signs and symptoms of CSF shunt obstruction, and their ages ranged from 3 month to 16 years with a mean age of (5.8 years) see Figure 1.
Clinical presentations
The clinical symptoms were collected in Table 1 and clinical signs in Table 2.
Symptoms |
Number of cases |
% of cases |
Headache |
10 |
50 |
Vomiting |
10 |
50 |
Blurring of vision |
3 |
15 |
Increase head size |
7 |
35 |
Squint |
1 |
5 |
Disturbed conscious level |
1 |
5 |
Fits (new onset and recurrent) |
4 |
20 |
Fever |
3 |
15 |
Gait disturbance |
1 |
5 |
Irritability |
7 |
35 |
Abdominal distension |
1 |
5 |
Swelling at cranial wound |
1 |
5 |
Drowsiness |
3 |
15 |
Table 1 Clinical symptoms
Signs |
Number of cases |
% |
Increased head circumference |
5 |
20 |
Bulging anterior fontanel |
7 |
35 |
Sixth nerve palsy |
1 |
5 |
Papilledema |
8 |
40 |
Unable to depress reservoir |
13 |
65 |
Reservoir does not refill |
6 |
30 |
Decreased LOC (Level of Consciousness) |
3 |
15 |
Table 2 Clinical signs
Causes of Hydrocephalus (Table 3)
Type of hydrocephalus |
No. of cases |
% of cases |
Congenital |
||
Aqueductal stenosis |
10 |
50 |
Chiari type II |
3 |
15 |
Dandy walker cyst |
1 |
5 |
Acquired |
||
Tumor |
3 |
10 |
Post meningitic |
2 |
10 |
Post traumatic |
1 |
5 |
Total |
20 |
100 |
Table 3 Causes of Hydrocephalus in our cases
Investigations (Table 4)
Investigations |
CT-Brain only |
Radionuclide shuntogram only |
CT-Brain and Shuntogram |
Positive cases |
20 |
18 |
18 |
Negative cases |
0 |
2 |
0 |
True positive |
19 |
18 |
18 |
False positive |
1 |
0 |
0 |
True negative |
0 |
1 |
0 |
False negative |
0 |
1 |
0 |
Sensitivity |
100.00% |
94.73% |
100.00% |
Positive predictive value |
95.00% |
100.00% |
100.00% |
Specificity |
N/A |
100.00% |
N/A |
Negative predictive value |
N/A |
50.00% |
N/A |
Accuracy |
95.00% |
95.00% |
100.00% |
Table 4 Investigations used in the evaluation of shunt malfunction
CT-Brain: Using CT-Brain only, we evaluated the shunt function in our 20 cases, we found the ventricles to be dilated in all 20 cases, but obstructions were confirmed only in 19 cases, and one case proved to be a false positive (with relief of symptoms and negative shuntogram). Surgical revision was done for 19 cases and shunt obstruction was confirmed. We calculated Sensitivity (100%), positive predictive value (95%), and accuracy (95%). We couldn’t calculate the specificity and negative predictive values, since there were no negative cases in our study.
Radionuclide shuntogram: Using radionuclide shuntogram only, we evaluated the shunt function in all cases. We found that 18 of the cases showed positive (abnormal) shuntograms, while 2 cases gave negative (normal) shuntograms. One of which was a false result as the patient symptoms of shunt obstruction persisted and intraoperative findings revealed distal obstruction, and the clinical presentation improved after surgery. The other case proved to be true negative, as the clinical symptoms improved after few days and no surgical intervention was needed. Sensitivity was 94.73%, specificity 100%, accuracy 95%, positive predictive value 100% and negative predictive value of 50%.
CT-Brain combined with shuntogram: When evaluating Using both CT-Brain findings and radionuclide shuntogram, we identified the test as positive when both tools gave positive results and negative when both tests gave negative results. As a result, the combined tools, gave 18 positive cases, and all of them were true positive cases. Since we didn’t get any case with negative CT-Brain, no negative case was obtained. The remaining 2 cases showed positive CT-Brains and negative shuntograms. Sensitivity of both tools combined is 100%; positive predictive value 100% and accuracy of 100%. However, we could not calculate the specificity and negative predictive values, as there were no negative cases.
Site of obstruction
We performed surgery for 19 of the 20 cases and the site of obstruction were identified as shown in Table 5.
Site of obstruction |
Number of cases |
Proximal obstruction |
5 |
Distal obstruction |
13 |
Both Proximal and distal |
1 |
Table 5 Site of obstruction
Case Presentations
Case 1: Male patient, 16years old, Radionuclide shuntogram revealed localized peritoneal collection of radiotracer 99mTc DTPA denoting distal obstruction and CT brain showed dilated ventricles and dandy walker cyst with proximal shunt tubes within lateral ventricle and cyst, see Figure 2.
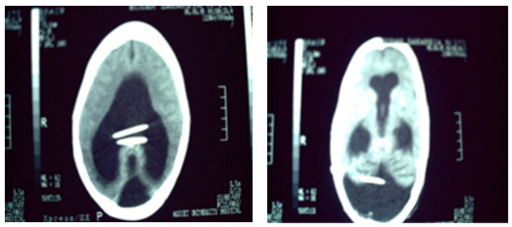
Figure 2 Case (1), Above: Radionuclide shuntogram with localized peritoneal collection of the radiotracer (99mTc DTPA), Below: CT brain showing dilated ventricles and dandy walker cyst with proximal shunt tubes within lateral ventricles and cyst.
Case 2: Male patient, 10 months old, Radionuclide shuntogram showed free peritoneal spilling of radiotracer denoting no distal obstruction but he had proximal obstruction as difficult CSF aspiration from reservoir occurred in spite of well visualized lateral ventricles, see Figure 3.
Our series included 20 patients, who were presented with symptoms and signs of shunt malfunction. They included 15 males (75%) and 5 females (25%), and their ages ranged from 3 month to 16 years with a mean age of (5.8 years). In our study, the most common cause of hydrocephalus was aqueductal stenosis (50% of cases). Clinically, all our patients presented with the general syndrome of increased intracranial pressure and the commonest signs were reservoir pumping test that revealed either resistance or delayed refilling (95%), papilledema (40%), bulged anterior fontanel (35%) and increased head circumference (25%).
After being investigated, we confirmed true 19 cases of shunt obstruction (all needed surgical interventions) and one case which its symptoms resolved spontaneously without surgery after few days. The sites of obstruction were 65% (13 cases) with distal obstruction, 25% (5 case) with proximal obstruction and 5% (1 case) with both proximal and distal obstructions.
We investigated the shunt malfunction using CT-Brain only, Radionuclide shuntogram only, and using both tools together.
Using CT-Brain only
CT scans showed abnormalities, suggestive of CSF shunt obstruction in 19 patients that required surgery (all true positive cases) and one false positive case. Surgical revision was done for 19 cases and shunt obstruction was confirmed.
Regarding the false positive case, it had a negative shuntogram and was followed up clinically for a few days, the symptoms resolved spontaneously, and no surgical intervention was done. The patient was followed in out-patient clinic and no recurrence of symptoms appeared. We couldn’t find any evidence that the patient’s symptoms were due to intermittent obstruction.
The CT-Brain sensitivity in our study (100%) was higher than that reported by Ouellette et al.8 in their retrospective series of 69 patients, evaluated for suspected cerebrospinal shunt obstruction, as CT scans showed abnormalities suggestive of CSF shunt obstruction in only 20 patients from 26 true obstructive cases, with a sensitivity of 77%.
Using Radionuclide shuntogram only
It was done for all cases and showed abnormality suggestive of CSF shunt obstruction in 18 cases (true positive cases) and was normal in 2 cases (one true negative and one false negative case).
Regarding the true negative case, it was the false positive case discussed above under CT-Brain. In the false negative case, the patient had a positive CT-Brain, and the clinical symptoms persisted after conservative management. Surgical exploration revealed distal obstruction and postoperative improvement occurred.
In our study, negative predictive value of 50% was lower than that reported by Ouellette et al.8 In their study, they found that CSF shuntograms showed abnormalities suggestive of CSF obstruction in 24 patients that required surgery (sensitivity 92%; negative predictive value 93%).
May et al.9 also studied results of shuntograms in 85 patients (46 true-positive results, 33 true-negative results, 2 false negative results, and 4 false-positive results) with 89% specificity and 93% accuracy.
The sensitivity, specificity, accuracy, positive and negative predictive values in our study were higher than that reported by Vassilyadi et al.7 who found in their study of 68 shuntograms that sensitivity of shuntograms is 62.9%, specificity 81.1%, accuracy 71.2%, positive predictive value 70.8% and negative predictive value 75%.
In our study of this group false negative results were one case (false negative rate of 50%), which was high compared to the other series discussed before, as they showed false negative rates of 11-16%.
Using CT-Brain and radionuclide shuntogram
In our study, we found that CT scans and shuntograms combined revealed abnormalities suggestive of CSF shunt obstruction in 18 cases (all true positive ones who required surgery), and no negative cases, leaving 2 cases of conflicting results between the 2 tools (CT-Brain was positive and shuntogram was negative).
In combining the shuntogram with CT-Brain, accuracy increased to 100% from 95% of either tool alone. Ouellette et al.8 showed increase in sensitivity to 96% when combining both tools.
No recorded complications occurred from the use of radionuclide shuntogram in our study, likewise other mentioned studies.
Despite the proven effectiveness of CSF shunts in treating hydrocephalus, complications related to shunt failure continue to occur with increasing frequency. The obstructed shunt system should be revised if it is symptomatic, even if the symptoms are subtle or atypical. Ventriculoperitoneal or ventriculoatrial shunt malfunction is a common problem that is occasionally difficult to be diagnosed and managed. Clinical presentation in patients with shunt malfunction is typically nonspecific such as fever, headache, nausea, vomiting and disturbed consciousness. These symptoms clearly overlap with typical infective syndromes, and brain imaging alone may fail to determine the origin of obstructive-like symptoms.
CT brain is simple, rapid, noninvasive and available at any time as a diagnostic tool especially in emergency cases, but prior CT scans were often needed for comparison and to confirm the diagnosis of CSF shunt obstruction. But it can only offer anatomical assessment. Also, sometimes dilated ventricles can happen without obstruction.
Radionuclide shuntogram is a simple, non invasive and easy to perform procedure that could assess CSF shunt anatomically and physiologically. Combined with CT brain, it will increase the accuracy to diagnose shunt obstruction. Its disadvantages are being a lengthy technique and more expensive than CT brain.
In our study, combining CT-Brain and Radionuclide shuntogram gave an accuracy and sensitivity of 100% in all the cases that was confirmed to be positive by both tools.
The limitations of our study, is the low number of our patients. As a result, we have no negative CT-Brain scan cases, so we can’t comment on the negative predictive value and specificity of using CT-Brain or the combined tools. The high false negative rate of 50% in our shuntogram cases is also a result of having only 2 negative cases (one true and one false case).
Although our results showed that adding shuntogram to CT-Brain increased the diagnostic accuracy to 100%, we still couldn’t recommend using shuntogram routinely in the clinical settings due to the time and expense involved in shuntograms. We recommend using the combined tools selectively in cases where there is doubt in the origin of the patient clinical symptoms.
We also recommend doing further study with a larger number, and also comparing different type of tracers used in shuntograms and their relations to the test accuracy.
None.
None.

©2015 Hassan, et al. This is an open access article distributed under the terms of the, which permits unrestricted use, distribution, and build upon your work non-commercially.