Journal of
eISSN: 2373-6410


Case Report Volume 1 Issue 5
Department of Surgery, McMaster University, Canada
Correspondence: Ahmed Al Jishi, Department of Surgery, Division of Neurosurgery, McMaster University, Hamilton, Ontario, Canada, 237 Barton St E, Hamilton, ON L8L 2X2, Canada, Tel 1-905-521-2100, Fax 1-905-522-2615
Received: August 26, 2014 | Published: September 16, 2014
Citation: Al Jishi A, Yarascavitch B, Murty N. Management of inadvertent injury to superior sagittal sinus in parasagittal meningioma: technical note. J Neurol Stroke. 2014;1(5):165-167. DOI: 10.15406/jnsk.2014.01.00031
Background: Parasagittal meningioma is a common type of intracranial meningiomas. Surgical resection of such lesions can result in injury to superior sagittal sinus. In rare occasions, extended craniotomy might be required for uncontrollable hemorrhage from a lacerated venous wall.
Objective: In order to avoid extended craniotomy, we attempted a surgical technique that would provide more sustained control over the lacerated venous sinus.
Method: A 56 year old lady underwent surgical resection for parasagittal meningioma. The lateral wall of the superior sagittal sinus was preached while scraping the tumor capsule from the sinus wall. Owing to difficulty in controlling the bleeding site, a tack up falx-assisted tension suture was attempted with a mass of Gelfoam and Surgicel over the laceration.
Results: Adequate control for the venous sinus laceration.
Conclusion: The falx-assisted suturing technique is quick, easy to perform and efficient in maintaining a constant tamponade effect over the lacerated site. We highly recommend such technique prior to extending the craniotomy over an injured venous sinus.
Keywords:Parasagittal meningioma, Superior sagittal sinus injury
SSS, Superior Sagittal Sinus; VAE, Venous Air Embolism
Parasagittal meningioma is the most common intracranial meningioma.1Surgical resection is being conducted for large and symptomatic lesions. Evaluation of superior sagittal sinus (SSS) involvement preoperatively is essential as it would reflect on surgical preparation and need for exposing the sinus or not. The essence of avoiding SSS exposure in parasagittal meningiomas is probably preferred among different neurosurgical centers, especially if the SSS is completely spared from tumor invasion. Nonetheless, and under such condition, inadvertent injury can happen to the side wall of the sinus. In most occasions, the incident is controllable but it might be pernicious and the patient may be at risk of excessive blood loss or developing venous air embolism. In rare occasions, an extension of the craniotomy over the injured sinus might be required in order to repair the sinus. In order to overcome such obstacle, we recently encountered a laceration to the lateral sinus wall of the SSS. A novel surgical approach was performed that was efficient and allowed us to avoid extending the craniotomy over a lacerated venous sinus.
A 56 year old woman was brought to a peripheral emergency department after being discovered unresponsive. She had been complaining of headache associated with nausea, vomiting and lethargy for approximately one week. Her husband left her to get stronger analgesics due to her escalating headache and when he returned she was unconscious and not rousable.
Upon arrival to local emergency department, the patient had a GCS of 8 and was intubated for airway management. The patient then underwent an urgent CT head that demonstrated a large (6.2 x 4.7 cm) fight frontal heterogeneous lesion with areas of internal hemorrhage and mild edema with a resultant 13mm of leftward shift. The patient was resuscitated and transferred to our tertiary neurosurgical centre for further management.
On arrival to our intensive care unit, seizure activity was noted and the patient was loaded with phenytoin and hyperosmotic therapy was initiated. Sudden deterioration earlier was thought to be due to a post-ictal state. An urgent MRI was more in favor of parasagittal meningioma (Figure 1). Her exam improved to localizing on the right and eye opening. Owing to significant mass effect that contributed to drop in her neurological status, we opted to intervene surgically for the sake of decompression and control of her intracranial hypertension and obtaining samples for pathological diagnosis.

Figure 1 Cerebral MRI demonstrating large parasagittal meningioma. Note that the superior sagittal sinus is spared from tumor invasion.
Operative technique
The patient was brought to the operating room and positioned supine with a head tilt toward the right at 15 degrees and elevated to enhance venous drainage. Image guidance (BrainLab) was used to map the tumor margins, superior sagittal sinus, draining veins and sylvian fissure. Dexamethasone infusion dose of 10 mg and Mannitol 1g/kg infusion were given intraoperatively. As the SSS was not invaded by the tumor, we did not feel the need to cross the midline with our right frontal craniotomy exposure. A durotomy was done with a 2 cm free margin and the tumor was explored. Tumor was resected easily due to its gelatinous consistency. A microsurgical dissection was done to dissect tumor capsule off cortical brain surface. A complete tumor resection was performed.
As we were scrapping the tumor capsule from the lateral wall of the SSS, a laceration of the sinus had occurred in the anterior portion of the sinus. The bleeding site was controlled with multiple layers of Surgicel (Ethicon), Gelfoam (Pfizer) and cottonoids. The site of bleeding remained under control while we maintained pressure at the lacerated area. However, despite adequate packing the site would continue to bleed when manual pressure was removed. It was not prudent for us to do a primary closure due to the limited craniotomy exposure near the sinus. At this point, instead of extending the craniotomy, we planned to apply a tension suture over the lacerated site assisted by the adjacent falx cerebri. The bony edge was drilled with two small diagonal holes. A 2.0 silk suture was used to suture the falx cerebri to the cranium which acted as a sling to support the Surgicel and Gelfoam tamponade (Figure 2 and 3). The sinus bleeding ceased with this pressure maintained by the suture sling. We then were able to proceed and complete the operation without further sinus bleeding. The patient was returned to the intensive care unit post-operatively. Her recovery was unremarkable for any neurological changes. A follow up MRI had shown patent SSS with good venous blood flow.

Figure 2 Intraoperative view post tumor resection illustrating the superior sagittal sinus had been controlled with the aforementioned technique.
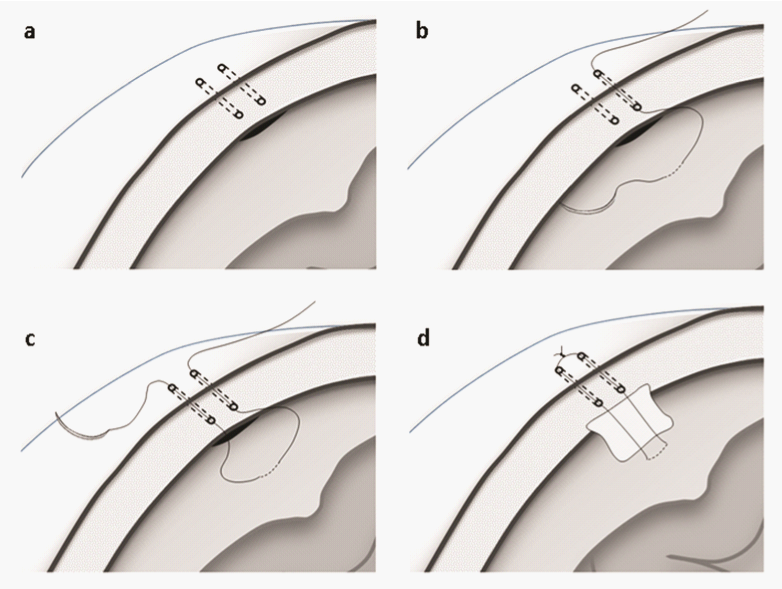
Figure 3 Two diagonal holes are made through the cranial bone over the lacerated sinus (a). A suture is passed through one hole and then through the falx cerebri (b,c). Gelfoam and Surgicel are positioned at lacerated sinus during these steps. After that, final suture tightening is made to maintain tamponed materials in place (d).
Surgical interventions for intracranial parasagittal meningiomas have become more popular in the last few decades. The development of microsurgical skills and image guidance technique have enabled the surgeons to approach such lesions with competence and predetermined goals of intervention. Recent literature has shown that complete resection provides better long term prognosis.2 However, surgical complications may arise from such approach, especially in dealing with meningiomas that are involving the dural venous sinuses.
Venous air embolism (VAE) is a one serious complication that can occur if a lacerated sinus is not managed properly,3-5 especially if the venous sinus was not fully exposed. Different definitions had been used for VAE which mainly varies between detection of micro air-bubbles in transesophageal echo to a drop in end-tidal CO2. As such, the incidence of VAE remains relatively uncertain and it is usually judged based on symptomatic cases. The sitting position, for instance, carries a risk for VAE ranging between 9.3% and 82.6%.6-10 The upper end of high risk was reported in posterior fossa surgery performed in the sitting position. The risk drops significantly in horizontal positions to a range between 1.4% and 12%.3,11,12
The patency of venous drainage across the SSS carries higher significance as compared to the rest of the cranial venous sinuses. Interference of the venous blood flow can lead to venous congestion to each cerebral hemisphere with secondary venous infarction. Hence, surgical intervention for meningiomas invading the SSS mandates restoration of the venous blood flow. The reported mortality and morbidity had reached 10% and 12.3%, respectively, in situations where venous reconstruction had not been performed.13 Nowadays, numerous surgical techniques have been implemented in reconstructing the venous sinuses with good clinical outcome.14-19 A graft is usually applied over the preached sinus. The graft can be from patient own saphenous vein or temporalis facia, or allograft material. Morbidity and mortality have become less with 8% and 3%, respectively, in some series.20 Nonetheless, spontaneous sinus thrombosis after grafting have been always a concern. Hence, patients can still be at risk for having delayed cerebral venous infarction. In addition, in some of these techniques, temporary clamping of the SSS is required while repairing the SSS. Some have considered it traumatizing to the sinus wall which can predispose to sinus thrombosis.
The gain from our aforementioned surgical technique is that it can be easily applied in managing small lacerations of the SSS upon resecting lesions in close proximity. It carries the advantage of avoiding craniotomy extension over that injured sinus, a step that can potentially lead to a larger laceration. It also provides a secure and perpetual tamponade over the lacerated sinus through efficient and uncomplicated manner. Surgeons can certainly avoid extra unnecessarily steps of harvesting a graft, clamping the venous sinus and further risk of SSS thrombosis. Hence, we highly recommend this technique prior to extending the craniotomy over the SSS. Nevertheless, surgeons should be attentive and take different perioperative precautions in order to avoid injury the superior sagittal sinus.
None.
None.

©2014 Al, et al. This is an open access article distributed under the terms of the, which permits unrestricted use, distribution, and build upon your work non-commercially.