Journal of
eISSN: 2373-4345


Research Article Volume 14 Issue 4
1Orthodontist, Private Practice, USA
2Clinical Associate Professor, Tufts University, School of Dental Medicine, Former Faculty, Harvard School of Dental Medicine, Boston, MA, USA
Correspondence: Tom C. Pagonis, DDS, MS, Clinical Associate Professor, Tufts University, School of Dental Medicine, Boston, MA, USA
Received: November 23, 2023 | Published: December 6, 2023
Citation: Viazis AD, Pagonis TC. Prediction of orthodontic treatment duration based on the alveolar bone formula. J Dent Health Oral Disord Ther. 2023;14(4):142-149. DOI: 10.15406/jdhodt.2023.14.00607
Orthodontic treatment duration remains a challenge to predict, often relying on clinical experience and scientifically unestablished or arbitrary norms. This article presents a biologically based approach, focusing on alveolar bone morphology, and introduces novel concepts of cupping depth, probing width, probing height, probing overbite and probing distance measurements as predictive parameters for orthodontic treatment duration.
A comprehensive treatment protocol, integrating these measurements into the newly proposed Alveolar Bone Formula (ABF), is outlined. This innovative approach signifies a shift towards a more personalized and effective orthodontic treatment planning process.
Keywords: Orthodontics, cupping depth, probing width, probing height, probing distance, Fastbraces, orthodontic treatment time
Orthodontic treatment is designed to correct malocclusions, align teeth, and enhance oral health and aesthetics.1–3 The duration of orthodontic treatment varies based on factors such as individual case complexities, orthodontic system choice, alignment with patient expectations, patient age, and treatment techniques.4–11
However, accurately estimating treatment duration remains a challenge in orthodontics. Current predictions rely heavily on clinical experience and established norms, which may prioritize achieving a Class I occlusion without a scientific foundation.12 While some factors offer general guidance, precision and personalization are lacking for accurate assessments. Despite advances in understanding tooth movement biomechanics and alveolar bone remodeling, the routine use of alveolar bone measurements and remodeling rates as predictive parameters for treatment duration remains unexplored. Pretreatment assessment of alveolar bone architecture is a critical step in this direction.
Understanding each patient's alveolar bone dynamics can lead to more precise predictions of treatment duration and outcomes. This article introduces an innovative approach by incorporating alveolar bone measurements as predictive parameters for orthodontic treatment duration. These measurements serve as proxies for understanding the amount of alveolar bone remodeling required to achieve successful orthodontic outcomes. The rate of alveolar bone remodeling, regardless of the dimension (i.e., axial/horizontal, coronal, and sagittal), further enables precise prediction of orthodontic treatment times. These novel measurements, like cupping depth, are assessed in millimeters (mm) using a periodontal probe, providing diagnostic insights into alveolar bone deficiency or hyperplasia and potential for restoration.
This article will further explore the rationale behind this innovative approach and the transformative impact of novel parameters in orthodontic practice, including:
The introduction of the Alveolar Bone Formula (ABF), a comprehensive instrument that synthesizes these measurements, plays a pivotal role in enhancing the precision of treatment planning, particularly in predicting accurate treatment time durations.
Orthodontic treatment relies significantly on the intricate process of alveolar bone remodeling, which shows great potential as a predictive parameter for determining precise treatment durations. This process involves two fundamental aspects: alveolar bone resorption and restoration. According to the pressure-tension theory in orthodontic tooth movement, compression on the periodontal ligament side triggers alveolar bone resorption, while tension on the opposing side stimulates bone formation.
Orthodontic tooth movement is an intricate process involving a cascade of cellular and biochemical events driven by osteoclasts, osteoblasts, prostaglandins, neuropeptides, and cytokines. These elements collectively work to reposition teeth within the alveolar architecture during treatment.14 This dynamic process governs orthodontic therapy, where interactions between teeth, the periodontal ligament (PDL), and the alveolar bone follow biomechanical principles.
The rate of alveolar bone remodeling during orthodontic tooth movement can vary depending on several factors, including the magnitude of force applied, the patient's age, genetics, and the specific location within the oral cavity.15,16 On average, bone formation and conversely bone resorption during orthodontic tooth movement is estimated to occur at a rate of approximately 0.5 to 1.5 millimeters per month.16–18 However, it's important to note that this rate is a general guideline and can vary among individuals and even within various stages of therapy.
To address these complexities, the authors propose novel pretreatment alveolar bone diagnostic parameters. These parameters collectively encompass various clinical presentations of alveolar bone conditions, including hypoplasia associated with misaligned teeth, open bites, hyperplasia related to dental spacing, overbites, under bites and excessive overjet. Depending on the clinical diagnosis, these parameters correlate with the extent of bone development or resorption required during orthodontic treatment, providing quantitative assessments of alveolar bone conditions and their impact on treatment duration.
A comprehensive assessment is crucial before commencing orthodontic treatment, encompassing not only the evaluation of malocclusions but also a detailed examination of alveolar bone conditions. This involves measurements of cupping depth, probing width, probing height, and probing distance, providing a comprehensive understanding of the patient's orthodontic needs. These innovative concepts herald a new era of precision and personalization in orthodontics. They offer crucial insights into treatment planning and duration estimation, significantly elevating the standards of orthodontic care.
Cupping depth (CpD)
Cupping depth, measured in millimeters using a periodontal probe aligned parallel to the occlusal surface, serves as a valuable indicator of alveolar bone deficiency and potential for restoration (Figure 1). The integration of cupping and pocket depth measurements provides clinicians with a powerful diagnostic tool for assessing overall periodontal health and establishing diagnostic associations with axial (horizontal) alveolar bone loss. This innovative protocol enhances clinicians' ability to evaluate the axial dimension of alveolar bone loss.
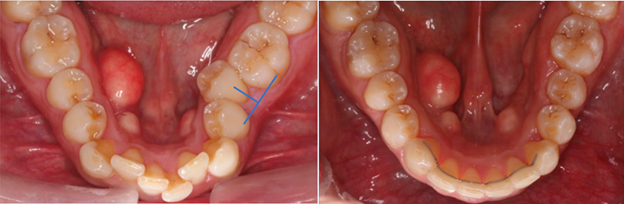
Figure 1 Pretreatment diagnosis of moderate cupping-tooth #20 and post orthodontic treatment showing alveolar bone restored.
In practical terms, a greater cupping measurement signifies a higher degree of volumetric bone deficiency. Unlike periodontal pocket depths, where increased depths usually indicate greater disease severity, larger cupping depth measurements correlate with a higher potential for restoring alveolar bone volume to natural or normal levels.
To measure cupping depth, the periodontal probe is aligned parallel to the incisal or occlusal plane, determining the distance between the facial or buccal surface of the misaligned tooth at its most prominent facial convexity and the adjacent tooth's corresponding surface. This objective measurement quantitatively evaluates alveolar bone deficiency, providing valuable insights into the extent of cupping in the misaligned tooth, guiding orthodontic interventions for achieving normalized alveolar bone architecture concurrent with the alignment of misaligned teeth.
Probing width (PbW)
Probing width is a critical metric when addressing cases involving interdental spacing or alveolar bone hyperplasia. Measured in millimeters (mm), probing width plays a pivotal role in predicting orthodontic treatment duration by quantifying the extent of necessary bone reduction to decrease the hyperplasia and achieve the desired dental arch form (Figure 2).
These measurements can be easily obtained using a periodontal probe and measuring the collective extent of interdental spacing, making them practical and valuable tools for predicating treatment duration. By incorporating probing width into their assessments, orthodontic practitioners enhance the precision and personalization of orthodontic care.
The probing width measurement will be 0 (zero) at the the end of orthodontic treatment. This means that not only do we have zero spaces left but that the alveolar bone had been reduced to the extent needed to eliminate its hyperplasia.
This will be achieved by changing the elastic power chains on the Fastbraces® Turbo® XtraTM brackets every ten (10) days. It is estimated that the alveolar bone will be reduced at a rate of 0.5 mm every 10 days via resorption remodeling from the constant and consistent pressure of the power chains (that are replaced with new ones every 10 days) until the probing width becomes zero at which point a lacing wire will be applied to stabilize the result and allow for the periodontal ligament (PDL) around the teeth to adjust accordingly.
Probing height (PbH)
Probing height, a critical parameter expressed in millimeters (mm), is particularly relevant in cases involving alveolar bone hypoplasia associated with anterior open bites (Figure 3). This metric evaluates the greatest interincisal height at occlusal rest, providing insights into the vertical dimension of the alveolar bone and its correlation with tooth alignment. Essentially, it quantifies the necessary alveolar bone apposition to close the anterior open bite.
In instances of an anterior open bite, probing height measurement becomes indispensable, offering guidance on the required alveolar bone remodeling to achieve a normal occlusion, typically characterized by a 2 mm lateral incisor overlap (overbite). This parameter illuminates vertical tooth movement and its correlation with alveolar bone alterations, aiding in predicting treatment time.
Probing height reduction is facilitated through the use of orthodontic elastics in the canine area and interproximal enamelplasty (IPE), resulting in a 2 mm upper lateral incisor overlap over the lower incisor.
Similar to probing width measurements, orthodontic practitioners can easily obtain probing height measurements using a periodontal probe. These measurements, when integrated into treatment planning, contribute to greater precision and personalization of orthodontic care. Assess the greatest interincisal height at occlusal rest, especially in cases involving alveolar bone hypoplasia associated with anterior open bites. Measure using a periodontal probe to determine the vertical dimension of the alveolar bone and its relationship to tooth alignment. This measurement quantifies the amount of alveolar bone apposition needed to close the anterior open bite. When dealing with alveolar bone hypoplasia associated with an anterior open bite, probing height measurements provide quantitative data for the treatment plan. Orthodontic interventions are designed to achieve a normal occlusion, typically characterized by a 2 mm overbite. Probing height measurements guide alveolar bone alterations to accomplish this goal.
Probing the overbite
Overbite is defined as the vertical overlap of the upper incisors over the lower ones, ideally falling within the range of 1-4mm, with categorizations as moderate (5-7mm) or severe (exceeding 8mm).
Addressing an overbite is a straightforward process with FASTBRACES® Technologies, especially when the lower canines remain visible upon anterior biting (Figure 4). However, if the lower canines are not visible, indicating an "over closed" bite, more extensive interventions such as bite blocks or even jaw surgery may be necessary.

Figure 4 Before and after correction of an Overbite Case.
This measurement illustrates the alveolar bone remodeling achieved during treatment.
To precisely measure the overbite, a periodontal probe is employed by placing it parallel to the upper and lower central incisors and visually assessing and measuring their overlap during the patient's repeated opening and closing motions.
The excess overbite beyond the ideal 2mm overlap of the upper lateral incisors over the lowers is measured with the Probing Height (PbH) measurement mentioned before minus the 2mm of normal overlap. For instance, if the upper incisors overlap the lowers by 8mm, the (PbH) measurement of the overbite is 6mm.
Probing distance (PbD)
This measurement is crucial when confronted with alveolar bone discrepancies leading to excessive or deficient overjet/underbite relationships. Probing distance, an innovative parameter, plays a pivotal role in predicting orthodontic treatment duration by providing quantitative insights into alveolar bone remodeling. This measurement focuses on the degree of overjet and underbite, representing the horizontal relationship of the upper and lower incisors (Figure 5).
Measured in millimeters (mm), probing distance's direction aligns with the current measurements of overjet, where a positive measurement number indicates a normal overjet, and a negative number signifies an underbite. It acts as a proxy measurement for assessing the amount of alveolar bone remodeling required to achieve a normal overjet or correct an underbite, serving as a precise predictor of treatment duration (Figure 6).

Figure 6 A & B Before and after underbite case. The probing distance here is mildly negative (2mm) while the cupping depth distance of the upper right lateral incisor is severe. This means that the alveolar bone remodeling and subsequent growth anteriorly in the upper incisor area is more than enough to overcome the negative probing distance and results in a positive overbite /overjet relation in a nonextraction, nonsurgical manner. No interproximal reduction (IPR) was needed here in the mandibular arch as the volumetric change in the alveolar bone growth in the maxillary incisor premaxilla area and especially around the maxillary right lateral, help correct the anterior crossbites/underbite. This may not be the case in moderately negative underbites and IPR will be needed. In severe underbites (severe negative probing distance) jaw surgery may be needed.
A typical overjet falls within the range of 1-3mm, possibly extending to 4mm in certain cases of bimaxillary protrusion dental arches. However, an underbite with the same measurements in millimeters represents the upper limit for non-extraction and nonsurgical treatment. While moderate and severe overjets can be significantly improved through nonsurgical methods, it is crucial to assess whether the patient has severe mandibular retrognathia and/or hyperplasia (dental spacing) for optimal treatment planning.
To perform probing distance measurement, employ a standard periodontal probe oriented parallel to the occlusal surface. This measurement direction aligns with the existing measurements of overjet. A positive measurement number, typically ranging from 1-3 mm, indicates a normal overjet. In contrast, a negative number signals an underbite.
Orthodontic interventions aim to establish a normal occlusion, typically characterized by a 2 mm overjet. The severity of an underbite is categorized as minor with 1-2 teeth involved, moderate with 3-5, and severe with 6 or more, potentially requiring surgical intervention. Probing distance measurements play a pivotal role in guiding alveolar bone alterations to achieve the desired overbite, quantifying the extent of remodeling necessary for proper alignment.
Probing distance, in this context, serves as a proxy measurement to assess the amount of alveolar bone remodeling necessary to achieve a normal overjet or correct an underbite, ultimately contributing to precise predictions of orthodontic treatment duration.
A significant aspect of these novel parameters is the classification into subcategories, based on clinical measurements which represent a proxy of alveolar bone remodeling required for successful orthodontic outcomes. When discussing the subcategories of mild, moderate, severe, very severe, extremely severe, and exceptionally severe, it's essential to recognize that these subcategories are applicable to all orthodontic parameters, including cupping depth, probing width, probing height, probing overbite, and probing distance (Table 1). Importantly, the measurements corresponding to these subcategories are consistent across all parameters, emphasizing that bone remodeling rates remain uniform, regardless of the dimension of remodeling (i.e., axial/horizontal, coronal, and sagittal). This process and subsequent classification provide predicable and personalized estimation of orthodontic treatment times when using FASTBRACES® Technologies and when the patient is seen in the office every 15 days for braces adjustments.
The assimilation of new metrics in this groundbreaking approach introduces a novel equation denoted as the Alveolar Bone Formula (ABF). This formula, designed to capture the fundamental architecture of alveolar bone, is represented as:
Here, CpD signifies the deepest cupping depth measurement, PbW represents the most substantial probing width in one arch, and either PbD which signifies overjet/underbite or PbH which signifies openbite /overbite is chosen based on the scenario on which measurement is larger. For additional clarification, after choosing the larger of PbD or PbH the formula can be viewed as follows:
In this formula ABM represents a measurement in millimeters which corresponds to the treatment durations shown in Table 1.
|
Subcategory |
Alveolar bone measurement (mm) - ABM |
Estimated treatment time (days) |
|
Mild |
0 to 4 mm |
About 100 days |
|
Moderate |
5-7 mm |
100-150 days |
|
Severe |
8-10 mm |
150-200 days |
|
Very Severe |
11-15 mm |
200-250 days |
|
Extremely Severe |
16-20 mm |
250-300 days |
|
Exceptionally Severe |
Over 20 mm |
Over 300 days |
Applicable to Cupping Depth, Probing Width, Probing Height and Probing Distance
Table 1 Subcategories, measurements, and estimated treatment time
This formula, encapsulating the key parameters of cupping depth, probing width, probing distance and probing height, is designed to quantify the extent of alveolar bone remodeling required for successful orthodontic outcomes. The integration of these parameters into the ABE emphasizes their uniformity across all dimensions of remodeling (axial/horizontal, coronal, and sagittal), reinforcing the predictability and personalization of orthodontic treatment times.
In summary, the subcategories, measurements, and estimated treatment times presented in Table 1 apply universally to these novel parameters and they provide valuable insights into orthodontic treatment planning and duration estimation, enhancing the overall quality of orthodontic care and patient outcomes.
Seven adult patients, seen by seven different clinicians presented for orthodontic treatment with open bites associated with alveolar bone hypoplasia (Figures 7, 8) and interdental spacing associated with alveolar bone hyperplasia (Figures 9, 10) along with cases of excessive overjet, overbite and underbite (Figures 11–13). These cases were successfully treated with the patented systems of FASTBRACES® Technologies.
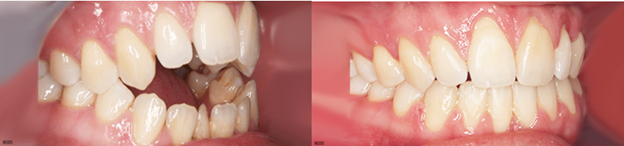
Figure 7 Treatment duration of 152 Days (within the range of 150-200 days). Before and after correction of an Openbite Case. Probing Height Measurement: This measurement, taken from the incisal edge of the right maxillary and mandibular lateral incisors, illustrates the alveolar bone remodeling achieved during treatment. The pretreatment ABM validated treatment duration in this case:
(0mm CpD + 1mm PbW + 8mm PbH = 9mm ABM).

Figure 8 Treatment duration of 129 Days. Before and after correction of an Openbite Case. Probing Height Measurement: This measurement, taken from the incisal edge of the right maxillary and mandibular lateral incisors, illustrates the alveolar bone remodeling achieved during treatment. The pretreatment ABM validated treatment duration in this case:
(0mm CpD + 0mm PbW + 5mm PbH = 5mm ABM).

Figure 9 Treatment duration of 113 Days (within the range of 100-150 days). Before and after correction of Interdental spacing. Probing Width Measurement: This measurement, taken between the maxillary central incisors, illustrates the closure of dental spacing achieved during treatment. The pretreatment ABM validated treatment duration in this case:
(0mm CpD + 5mm PbW (maxilla) + 2mm PbH = 7mm ABM).

Figure 10 Treatment duration of 89 Days (within 100 days). Before and after correction of Interdental spacing. Probing Width Measurement: This measurement, taken between the maxillary central incisors, illustrates the closure of dental spacing achieved during treatment. The pretreatment ABM validated treatment duration in this case:
(0mm CpD + 3mm PbW + Max (0mm PbD or 0mm PbH) = 3mm ABM).

Figure 11 Treatment duration of 169 Days (within range of 150-200). Before and after correction of excessive overjet. The pretreatment ABM validated treatment duration in this case:
(0mm CpD + 2mm PbW + 7mm PbH = 9mm ABM).

Figure 12 Treatment duration of 126 Days (within the range of 100-150 days). Before and after correction of excessive overbite. The pretreatment ABM validated treatment duration in this case:
(2mm CpD + 0mm PbW + 5mm PbH overbite = 7mm ABM). The cupping depth (CpD) in this example was taken from the lower incisors. The labially positioned teeth (canines) do not play a role in the ABM.

Figure 13 Treatment duration of 256 Days (just a few days above range of 200-250 days). Before and after correction of underbite. The pretreatment ABM validated treatment duration in this case:
(8mm CpD upper lateral + 0mm PbW + 3mm PbH underbite = 11mm ABM).
By implementing this treatment protocol, orthodontic practitioners can utilize cupping depth, probing width, probing height and probing distance measurements to enhance the quality of orthodontic care. These measurements when entered into the Alveolar Bone Formula (ABF) help align treatment goals with alveolar bone restoration, ensuring the achievement of stable occlusions and morphologic appearances. Ultimately, this approach leads to more accurate predictions of treatment durations and improved treatment outcomes for patients.
Orthodontic diagnosis and treatment planning traditionally focused on correcting malocclusions and tooth alignment based on arbitrary treatment goals. However, a paradigm shift toward a biologically based diagnostic approach now prioritizes the pretreatment clinical morphology of the alveolar bone. This approach emphasizes the restoration of alveolar hard tissue for proper alignment and occlusion, considering the patient's unique dentition and genetic morphologic appearance, rather than subjective ideals.
For over a century, orthodontics overlooked the unique anatomy and physiology of misaligned teeth, leading to arbitrary standards and unpredictable treatment durations. It is noteworthy to mention that the authors of this article have consistently asserted, in conjunction with accompanying publications, that orthodontic diagnosis and treatment planning should be grounded in the morphological aspects of the alveolar bone.19–29 In 2017, our approach to diagnosing misaligned teeth shifted, towards focusing on the pretreatment clinical morphology of the alveolar bone and accompanying orientation of tooth roots as biologically based constants which is a logical element in the diagnostic process.24
In this context, measurements like cupping depth, probing width, probing height and probing distance serve as pivotal pretreatment metrics. The Alveolar Bone Formula (ABF) plays a transformative role, fostering a deeper understanding of the interplay between these parameters and enabling precise treatment planning. The ABF aligns seamlessly with the utilization of FASTBRACES® Technologies, facilitating comprehensive evaluation of all dimensions of alveolar bone morphology for a biologically based orthodontic diagnosis and treatment planning.
Alveolar bone discrepancies, such as Maxillary or Mandibular Alveolar Hypoplasia and Maxillary or Mandibular Alveolar Hyperplasia, play a crucial role in this diagnosis, closely related to assessing alveolar bone architecture and predicting necessary remodeling for precise treatment duration estimates. Incorporating quantitative analysis of alveolar bone deficiencies aligns orthodontics with restorative dentistry and endodontics principles, emphasizing the importance of achieving proper tooth alignment and restoring surrounding hard tissues.
A proposed biologically based orthodontic diagnostic approach centers on the clinical morphology of alveolar bone, emphasizing the restoration of alveolar hard tissue. This considers natural dentition and individual genetic morphologic appearance, diverging from subjective ideals. The orthodontic diagnosis, grounded in alveolar bone biology, aims to improve morphology, advocating a non-extraction approach. Correcting alveolar bone from the start without altering molar relations is crucial for optimal oral health and facial aesthetics. Integrating novel alveolar bone metrics, alongside innovations like the FASTBRACES® system, enhances clinicians' ability to predict orthodontic treatment time.
Historically, orthodontics has faced criticism for lagging behind restorative dentistry in terms of addressing hard tissue restoration.13 Traditional orthodontic approaches, often involving tooth extraction and overlooking alveolar bone deficiencies, leading to unpredictable and often unreasonable treatment time duration have been carefully scrutinized.
Accurately assessing alveolar bone remodeling is a pivotal aspect of orthodontic treatment planning. Integrating alveolar bone measurements and tissue dynamics can potentially revolutionize orthodontic practice, leading to more efficient and effective care, ultimately benefiting both patients and practitioners.
The introduction of cupping depth, probing width, probing height and probing distance, integrated into the Alveolar Bone Formula (ABF), offers valuable quantitative insights. The ABF encapsulates these key measurements, emphasizing their role in determining the extent of bone remodeling required for predicting accurate orthodontic treatment times.
In understanding the treatment times calculated by the Alveolar Bone Formula, it is essential to recognize the inherent variability within clinical scenarios. Factors like individual case complexities, the chosen orthodontic system, alignment with patient expectations, patient age, and clinician skill all contribute to the observed broad ranges. Future refinements to the Alveolar Bone Formula (ABF) exists, aiming to incorporate and account for the nuanced variables that influence treatment times. This comprehensive approach enhances patient expectations and overall satisfaction by fostering a deeper understanding of the interplay between these parameters and contributing to the predictability and personalization of treatment durations.
There were no external sources of funding for this study.
The authors would like to thank the FASTBRACES® Dentist Providers that contributed the case data shown herein.
The authors deny any conflict of interest for the acceptance of these concepts.

©2023 Viazis, et al. This is an open access article distributed under the terms of the, which permits unrestricted use, distribution, and build upon your work non-commercially.