Journal of
eISSN: 2373-4345


Clinical Paper Volume 10 Issue 2
1Orthodontist, Private Practice, Dallas, Texas, USA
2Associate Clinical Professor, Tufts University, School of Dental Medicine, Former Faculty, Harvard School of Dental Medicine, Boston, MA, USA
Correspondence: Tom C Pagonis, Associate Clinical Professor, Tufts University School of Dental Medicine; former faculty, Harvard School of Dental Medicine, Boston, MA, USA
Received: April 08, 2019 | Published: April 16, 2019
Citation: Viazis AD, Pagonis TC. Orthodontitis: the distinct gingivitis around malpositioned teeth. J Dent Health Oral Disord Ther. 2019;10(2):171-177. DOI: 10.15406/jdhodt.2019.10.00479
Malpositioned teeth are subject to a unique set of periodontal circumstances including greater accumulations of bacterial plaque due to the difficulty of proper dental hygiene along with a specific bacterial flora which increases the severity of gingival inflammation, accelerate the progression of periodontal disease and serve as a contributing factor to major medical diseases. A reclassification of gingivitis into two conditions: one for straight teeth and one for malpositioned teeth is presented as a more efficient way to identify this differential in bacterial flora as well as achieve a more effective, conservative and nonsurgical treatment of malpositioned teeth.
Keywords: orthodontics, orthoeruption, orthodontosis, orthodontitis, gingival recession, gingivitis, periodontal disease
Periodontal disease is a multi-factorial inflammatory process that affects the supporting structures of teeth. Its pathogenesis is primarily caused by an ecosystem of bacterial species interacting with host tissue causing the direct destruction of the alveolar bone and the periodontal ligament. While the disease process is in part modulated by the host immune response and tissue structural factors, the key components in disease rest with the constituents of the bacterial flora within a dental biofilm.1 Periodontal pathogens produce localized damage in two different ways:
In addition, the possible relationship between periodontal disease and systemic disease is an important and ongoing research question. At least two decades of study have firmly established a correlation or association between periodontal disease and cardiovascular disease. Studies have identified periodontitis as a risk factor for chronic obstructive pulmonary disease, Alzheimer's disease and more recently psoriasis, colon cancer, and kidney disease.4−6 These rapid changes in research and understanding prompted a landmark 2017 consensus meeting of the European Federation of Periodontology and the American Academy of Periodontology which released the 2018 Classification of Periodontal and Peri-Implant Diseases and Conditions7 This new classification includes four major categories:
As we all know periodontitis or the progression from Category 1 to Category 2 is characterized by clinical histopathological, bacterial flora and molecular changes. Within 24 hours and at the initial stages of gingivitis, bacterial plaque results in vascular changes with intercellular gap formation and increased exudation of gingival crevicular fluid (GCF) in surrounding tissues. The infection quickly progresses with migration polymorphonuclear neutrophils (PMN), fibroblast degeneration, and collagen fiber breakdown by enzymatic collagenases. Within two to four weeks, there is a loss of connective tissue attachment which is accompanied by loss of alveolar bone and the apical migration of a gram- negative bacterial biofilm. It follows then that the primary goal of periodontal therapy is the reduction or elimination of bacterial plaque by patient dental hygiene and scaling by a dental hygienist.
Of interest is the subcategory "Gingivitis: Dental Biofilm-induced" under the first category or under Periodontal Health, Gingival Diseases and Conditions. Gingivitis that is dental biofilm or plaque induced causes the classic signs of localized tissue edema, erythema, bleeding but with no alveolar bone destruction. While early plaque in healthy individuals is dominated by gram- positive cocci and rods the progression towards gingivitis notes a maturing of the bacterial plaque and the emergence of higher proportions of gram- negative fusiform, rods and spirochetes. As the disease progresses from Category 1 (Periodontal Health, Gingival Diseases, and Conditions) to Category 2 (Periodontitis), gram -negative anaerobic bacteria are most responsible for causing tissue damage including Porphyromonas gingivalis, Eikenella corrodens, and Treponema denticola. This phenomenon illustrates the nature of chronic periodontitis as a polymicrobial disease resulting from the overgrowth of a limited number of bacterial species causing tissue destruction.1,4 The direct mechanism of tissue destruction for this profile of bacteria includes damage to crevicular epithelium, leukocyte impairment, degradation of immunoglobulins, degradation of fibrin, collagen and the activation of complement and bone resorption with the release of lipopolysaccharide (LPS) or endotoxin.8−10
Periodontal tissue differences between straight and malpositioned teeth
For malpositioned teeth, the periodontal considerations are magnified. Understanding the interrelation and impact of periodontal disease and orthodontic treatment is particularly important. In recent years, orthodontic treatment of the adult patient has substantially grown for a variety of reasons including the longevity of natural dentition, increased awareness of functional benefits of orthodontic treatment and increasing esthetic demands.11 This increased interest for the adult orthodontic patient requires special attention to their periodontal conditions. A large number of studies have been carried out to evaluate the interrelation of malocclusion, malpositioned teeth, and periodontal status. Whether it's the analysis of certain features of malocclusion in certain age groups or the periodontal impact of a malpositioned tooth compared to a properly positioned tooth, the periodontal impact of the disease is more severe. If left untreated the severity of crowding and malocclusion increases with age with a clinically notable increased severity of periodontal problems.12,13 Malpositioned teeth facilitate the accumulation of bacterial plaque by creating physical barriers to self-cleaning which directly contributes to gingival inflammation.14−16 The literature also confirms that the boney and soft tissue architecture created by malpositioned teeth contributes to the creation of unique bacterial flora. In 2000, Chung, Vanarsdall, and co-workers17 concluded that malpositioned anterior dentition in adults exhibited greater plaque accumulation, a greater number of periodontopathogens present in subgingival plaque with a significantly more common presence of Fusobacterium species, Capnocytophaga species, c rectus, and P micros when compared to non - malpositioned teeth. In addition, a study by Thornberg et al.18 examined levels of eight periodontal pathogens; Actinobacillus actinomycetemcomitans, Eikenella corrodens, Fusobacterium nucleatum, Porphyromonas gingivalis, Prevotella intermedia, Tannerella forsythia, Treponema denticola, and Campylobacter rectus on adolescents pre -operatively, peri - operatively and post-operatively. They concluded that orthodontic treatment had a positive effect post- treatment and protective for four of the pathogens, namely Eikenella corrodens, Fusobacterium nucleatum, Treponema denticola, and Campylobacter rectus. Also of note is that severity of crowding and malocclusion, if left untreated, increases with age with a clinically notable increased severity of periodontal problems.
The purpose of this paper is to present the fundamental differences in the periodontal presentation of malpositioned teeth when compared to straight teeth and propose Orthodontitis™ as the alternate and distinct term of gingival inflammation for malpositioned teeth. It seems fitting, particularly with the introduction of new periodontal diagnostic terms to review the authors' years of work towards this new diagnostic proposal. Understanding the differences between the unique clinical and microbiological presentation of gingival inflammation of malpositioned teeth one must appreciate the importance of creating specialized diagnostic terms related to both alveolar bone morphology and associated soft tissue characteristics. For nearly five years the authors have made the case and maintain that mainstream orthodontic treatment is based upon a flawed or even non - existent diagnostic process which leads to a flawed set of orthodontic classification terms. Moreover, there is an emerging and robust body of literature that continues to question and directly refutes the basis for conventional diagnostic classification of malocclusion. First introduced in 1899, Angle's classification of malocclusion1 in Class I ("ideal"/"normal"), II or III has remarkably endured and continues to be utilized as the main language of malocclusion. Angle's classification serves as the basis for orthodontic treatment planning for a large majority of orthodontic providers around the world, yet there is no evidence to suggest that this arbitrary "ideal" occlusion treatment goal provides significant health benefits or that it significantly improves oral function.2−4 In 2002, Rinchuse & Rinchuse stated that Angle's "normal" ("ideal)", is more accurately expressed as an extreme or a rare condition, affecting only 2 to 3% of the population. Furthermore, the authors of this 2002 study questioned the wisdom of forcing a stable, functional mandibular position to change in order to achieve a morphologic occlusion that conforms to an arbitrary ideal.5 In the Readers forum of a 2005 issue of the American Journal of Orthodontics and Dentofacial Orthopedics, it was stated that it is a false belief that one should always endeavor to establish "normal" Class I occlusion-a concept, referred to as a century old fixation that has been arbitrarily determined. Clinical experience suggests that it is valid to finish treatment to an acceptable esthetic, stable, and functional occlusion.6
Of note, a substantial number of educators question the use of Angle's system as he defined it. The results of an email survey revealed that about half of the respondents were dissatisfied with the Angle molar classification system and do not use the system in an academic setting. Many participants commented that molar classification was limited and should be avoided.7 The special section, "100 years of orthodontic history," published in the December 2015 issue of the American Journal of Orthodontics and Dentofacial Orthopedics, delineates the important events in the past 100 years of Orthodontics.8 The manuscript provides an important time-line and history of orthodontics but omits two critically important clinician-scientists, Kaare Reitan and Per Rygh who fundamentally contributed to the biology of tooth movement. The significance of this omission strongly suggests that orthodontics has been more technologically driven rather than biologically or scientifically.8,9
Angle's classification is not based on a verifiable biologically based constant or on observed and documented pathologic processes but relies on dental intercuspation or static occlusion which only takes place between 15 to 30 minutes per day. The logical and arguably unfortunate consequences of relying on arbitrary ideals rather than verifiable biologic constants in the diagnostic and classification process lead to a misdirected "one size fits all" orthodontic treatment. The need for a biologically based diagnosis which follows into a logical classification system is clear and compelling.
Development and significance of the viazis Classification
In 2014 the authors introduced a disease-based or biologically verifiable model of orthodontic diagnosis10 based on alveolar bone clinical morphology rather than subjective arbitrary "ideals". The disease-based term Orthodontosis™ was introduced and defined as the non-inflammatory deficiency of the alveolar bone in the axial plane caused by the displaced root(s) of the tooth, typically palatally or lingually. This term becomes more significant as the authors now hypothesize that Orthodontosis™ is the underlying precursor to the clinical manifestation of a cleft or, as defined, a split or separation of bone in craniofacial development.
The soft tissue consequence or resulting in excess soft tissue and chronic inflammation leads to the diagnostic term of Orthodontitis™. These terms serve as the basis of the cause or illness and disease in orthodontics. In 2017 the authors created the first set of classification terms which capture our disease - based model and identify Alveolar Hypoplasia and Alveolar Hyperplasia in both the maxilla and mandible.11 These observations led to the formulation and introduction of The Viazis Classification of Malocclusion. This orthodontic classification is appropriately based on the alveolar bone morphology and was proposed as the new system for orthodontic classification as the valid replacement of Angle's invalid thesis.
The Viazis Classification system is based on the morphology of alveolar bone and can be divided into two main categories of bone discrepancy: Alveolar Bone Hypoplasia and Alveolar Bone Hyperplasia. Each of these categories is based on the underlying diagnosis of Orthodontosis™10 for Hypoplasia and the introduction of Orthomegaly™ as the diagnostic component of Hyperplasia. These classifications identify the pre- treatment morphologic status of alveolar bone with the ultimate orthodontic goal of creating a natural dental arch morphology with proper and natural orientation of tooth roots and with a stable occlusion irrespective of an Angle molar classification. Both of these conditions demonstrate Orthodontitis™ which is the pathology expressed as gingivitis in the presence of malocclusion. Treatment of these two conditions also leads to treatment of the accompanying Orthodontitis™.10
The treatment of Alveolar Hypoplasia or Alveolar Hyperplasia results in the establishment of the natural dental arch similar or identical to what would have resulted from the perfect/natural eruption of straight teeth. The authors believe that this fundamental treatment goal is achieved through orthodontic mechanotherapy that is best described as the facilitation of natural eruption or Orthoeruption™.10 In the case of Alveolar Hypoplasia this process induces alveolar bone remodeling and development by moving roots toward their final naturally erupted position from the beginning of treatment. In the case of Alveolar Hyperplasia, (maxillary or mandibular) treatment follows a similar sequence of attaching brackets and wires to the teeth exhibiting clinical spacing and closing of these spaces with elastic power chains. The restoration of the alveolar bone toward the establishment of a patient -specific natural dental arch also treats associated soft tissue pathology or Orthodontitis ™ (around malpositioned teeth).
The authors believe that orthodontic mechanotherapy that is gently administered along the entire root surface on the pressure side is clinically expressed in a painless remodeling of the osteocytes from the osteoclastic activity. This is in stark contrast to tooth roots moving through the alveolar bone when heavier and arguably unnatural forces are used. On the tension side of tooth movement, the well - accepted phenomenon of periodontal ligament (PDL) stretching takes place and is accompanied by increased blood flow resulting in the deposition of newly formed osteoid bone from osteoblasts. This newly formed osteoid bone is subsequently mineralized to the osteocytes of alveolar bone. The end result represents alveolar bone remodeling towards attaining a natural arch form. This is all possible of course because the unique osteocyte network of lacuna canalicular which allows for all these similar activities to take place and alter its mass and even remodel its structure in response to mechanical forces. An obvious example of the interdependence between the tooth root and alveolar bone is the mere fact that when the roots are removed from the mouth (i.e., the edentulous patient or a previous extraction site) the alveolar bone network disappears. This takes place because of the absence of nourishment from the PDL. The unique bacterial flora around crowded or malpositioned teeth and the ease with which these teeth can now be moved to their correct position by uprighting their roots within a matter of 60 to 90 days with the patented methods of FASTBRACES® Technologies, makes obvious the need for the first ever division of the term gingivitis into two categories: one for straight teeth and one for malpositioned teeth. The authors recommend the continued use of the term gingivitis to describe the inflammation of the soft tissue/gingiva around straight teeth only and change it to the term Orthodontitis™ to describe the same around malpositioned teeth. This is a consequence of and consistent with the two distinct bacterial floras of each respective tooth and root alignment.17,18 The authors further suggest/propose that the uprighting of malpositioned roots with FASTBRACES® Technologies is just as important as dental scaling as the first or front line periodontal treatment strategy. This means that the primary dental instrument for gingivitis is a scaler whereas the primary dental instrument for Orthodontits™ is the bracket and wire of FASTBRACES® Technologies which facilitates the immediate root movement from the onset of treatment to their final upright position. This is then followed by the scaler 60 to 90 days later. The orthodontic treatment may then be completed for another few months in order to attain final occlusal adjustments.
According to the Viazis Classification, malpositioned teeth that were typically referred to as crowding should now be referred to as alveolar bone hypoplasia. It's remarkable that orthodontic diagnosis has ignored the unique periodontal architecture of malpositioned teeth for over a century by merely referring to malpositioned teeth with terms like "crowding". It is the distinctive alveolar bone morphology (Figure 1) typically labial to the lingually displaced roots of anterior teeth that results in insufficient labial alveolar bone and associated soft tissue, edema, and erythema.

Figure 1 Malpostioned mandibular anterior teeth are characterized by their lingually displaced roots which results in insufficient labial alveolar bone and associated soft tissue, edema and erythema. Note the distinct cleft labial to the mandibular left lateral incisor.
Case examples and objectives of treatment
The following case examples of malpositioned anterior teeth and severe localized gingival recession illustrates both the importance of biologically- based orthodontic diagnosis and the importance of specialized periodontal attention while showcasing the advanced capabilities of the patented systems of FASTBRACES® Technologies. The objectives of the following cases are threefold:
The first case example (Figure 1) illustrates the severe malpositioned mandibular anterior teeth. These malpositioned mandibular anterior teeth are characterized by their lingually displaced roots resulting in insufficient labial alveolar bone and associated soft tissue, edema, and erythema. Note the distinct cleft labial to the mandibular left lateral incisor. The accompanying graphic representation (Figure 2) illustrates the clinical objectives of uprighting (i.e. red arrows) roots to reverse Orthodontosis ™ and eliminate Orthodontitis™.

Figure 2 Graphic illustration of severely malpositioned mandibular anterior teeth and clinical objectives of uprighting (i.e. red arrows) roots to reverse Orthodontosis™ and eliminate Orthodontitis™.
The second case (Figure 3) displays moderately malpositioned mandibular anterior teeth and essentially illustrates the method and apparatus for the restoration of alveolar bone morphology. The patient presented to a FASTBRACES® provider's private practice with a chief complaint of unfavorable esthetic appearance as it relates to moderate alveolar bone hypoplasia or Orthodontosis™ labial to the lingually displaced mandibular incisors roots. This results in a deficiency of alveolar bone labial to the central incisor that demonstrates the gingival recession. The treatment objectives, in this case, are to restore the morphology of alveolar bone around the malpositioned teeth which in turn will allow for new bone to cover the recession.

Figure 3 Before Maxillary and Mandibular Orthodontosis™ and Orthodontitis™ of anterior teeth with localized severe gingival recession, (Courtesy of Dr. Patrick Assal, Lausanne Switzerland).
The patient received scaling and root planing followed by the application of brackets on the four maxillary anterior teeth for patient comfort (Figures 4). A subsequent appointment specifically addresses the application of brackets on the lingually inclined teeth while avoiding bracket application on labially inclined teeth (Figure 5). As the roots of previously lingually inclined teeth upright, brackets are placed on all teeth at a subsequent appointment (Figure 6). Clinical results along with photographs comparing pre and post treatment show dramatic periodontal and esthetic improvement, particularly with alveolar bone development and the reversal of recession (Figure 7). Treatment results are impressive as uprighting of the malpositioned roots creates remodeling of alveolar bone to accommodate the boney support of the properly aligned tooth. Post-treatment results also show a stable occlusion with proper overjet and overbite relations.

Figure 4 After scaling of teeth and application of four brackets on the maxillary anterior teeth for patient comfort, (Courtesy of Dr. Patrick Assal, Lausanne Switzerland).

Figure 5 Brackets are placed on lingually inclined teeth to facilitate alveolar bone formation by creating healthy soft tissue and the elimination of cleft formation previously associated with Orthodontosis™. Note that brackets are not placed on labially positioned teeth, (Courtesy of Dr. Patrick Assal, Lausanne Switzerland).
The third case highlights the method and apparatus for the treatment of Orthodontitis ™ and showcases treatment progress of uprighting the mandibular left lateral incisor. Note the straightening of the wire reflects and corroborates the uprighting root movement, the appearance of healthy soft tissue and the elimination of cleft formation previously associated with Orthodontosis™
The successful completion of this case highlights the clinical benefits of orthodontic intervention including improved alveolar bone architecture with the reversal of gingival recession, proper root alignment, improved function, and improved esthetics. This case also showcases the capabilities of FASTBRACES ® Technologies as a safe, effective and complete treatment non-extraction both for the periodontally compromised patient and among a diverse set of clinical presentations (Figure 8).23−28

Figure 6 Bracket placement on all teeth as previously lingually inclined roots are urighted, (Courtesy of Dr. Patrick Assal, Lausanne Switzerland).

Figure 7 After resolution of Maxillary and Mandibular Orthodontosis™
and Orthodontosis™ with improved alveolar bone and gingival architecture,
(Courtesy of Dr. Patrick Assal, Lausanne Switzerland).
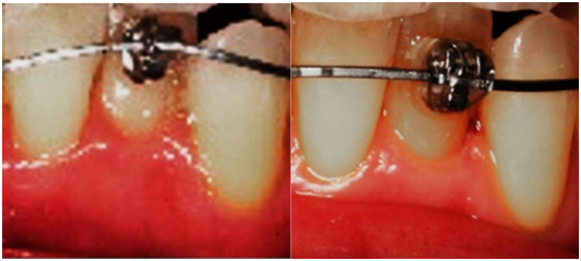
Figure 8 Treatment progress of uprighting the mandibular left lateral incisor in about 60 days. Note the straightening of the wire reflects and corroborates the uprighting root movement, the elimination of cleft formation previously associated with Orthodontosis™ and the elimination of Orthodontitis™. The teeth may not be completely aligned but gingival inflammation has been eliminated before strict orthodontic and esthetic treatment goals have been fulfilled.
Orthodontic treatment of malpositioned teeth can no longer be considered a cosmetic procedure and is more in line with an adjunctive periodontal treatment to restore the alveolar bone architecture, eliminate the unique soft tissue inflammation and to eliminate a unique pathogenic bacterial flora. Malocclusion including the prevalence of malpositioned and thus periodontally compromised teeth is one of the most important oral problems in the world population. The orthodontic and periodontal diagnostic combination has and should be common practice for the dental clinician especially with the increased interest in the orthodontic treatment of the adult patient. The therapeutic benefits of orthodontic treatment as part of a periodontal rehabilitation program include improved dental hygiene ultimately leading to greater removal of bacterial plaque thereby reducing gingival infection and Orthodontitis ™. This is followed by the establishment of a balanced occlusion with the proper overbite and overjet of 1 to 3 mm.
These case examples corroborate other research findings23 and confirm the diagnostic and therapeutic interrelation of orthodontics and periodontal disease. While many factors contribute to the onset and progression of periodontal disease, the main etiological factor remains the bacterial microflora of plaque. For the adult patient with concomitant periodontal disease and malpositioned teeth, including anterior crowding, incisor proclination or mandibular tipping, the clinician must appreciate the following
Based upon the definitions of Orthodontosis™ and Orthodontitis™, orthodontic treatment even for the periodontally compromised patient should be directed towards mimicking and continuing the light forces of natural eruption stimulating bone remodeling around displaced roots. This eliminates the need for extraction therapy and in the case of this periodontally involved patient; it stimulates favorable bone remodeling creating a foundation for attached gingiva and decreased recession. The alveolar bone reacts to a tooth erupting in its correct place in the arch. Furthermore, this mechanically assisted continuation of the eruption has been defined as Orthoeruption™ (19) and allows for the uprighting of displaced roots into a straight position as if the teeth erupted in that position. Much like the remodeling of alveolar bone to accommodate teeth during the natural eruption, orthodontically induced eruption or Orthoeruption™ stimulates the continued remodeling of alveolar bone to accommodate the roots towards their final naturally erupted position. Therefore, Orthoeruption™ results in the alveolar bone remodeling and restoration of the dental arch to its appropriate natural size and shape as per the patented methods of FASTBRACES ® Technologies.
By definition natural eruption is root movement which is followed by alveolar bone growth. The new bone around the final position of the naturally erupted root demonstrates the alveolar bone growth that occurred during the eruption. If not, the root would find itself outside the alveolar bone housing. So a de facto consequence of root movement in the natural eruption is the alveolar bone growth around the new position. Much like the remodeling of alveolar bone to accommodate teeth during the natural eruption, orthodontically induced eruption or Orthoeruption™ stimulates the continued remodeling of alveolar bone to accommodate the roots towards their final naturally erupted position.
Malpositioned teeth are subject to a unique set of periodontal circumstances including greater accumulations of bacterial plaque due to the difficulty of proper dental hygiene along with a specific bacterial flora which increases the severity of gingival inflammation; accelerate the progression of periodontal disease and serves as contributing factor major medical diseases. Successful orthodontic treatment for this patient type not only addresses the esthetic and functional problems of malpositioned teeth but can have a favorable therapeutic effect on a patient's periodontal status. Simply stated orthodontic clinicians are looking at the wrong item – or looking at "crowding". The questions should be, what caused this and how can we restore normal alveolar bone architecture or what nature has done in the first place. As the periodontist focuses on the periodontium so should the orthodontic clinician. If the treatment for crowded teeth requires additional alveolar bone creation and if the spacing of teeth suggests the need for alveolar bone reduction, then why not look at the bone in the first place? The FASTBRACES® Technologies system of braces facilitates the continuation of the eruption as it allows for immediate root movement of teeth which induces alveolar bone remodeling and development in a matter of 60 to 90 days. This allows for the improvement of periodontal disease prior to the completion of strict orthodontic treatment objectives. From both a clinician's and patient's perspective this means electively continuing the orthodontic treatment after the periodontal therapeutic objectives have been fulfilled. The improvement of periodontal disease takes place at the onset of orthodontic tooth movement. Utilizing this flexibility of orthodontic treatment by resolving associated periodontal problems first allows for more favorable dental cleanings and ongoing dental hygiene maintenance. The authors believe and propose the reclassification of gingivitis into two conditions: gingivitis for straight teeth and Orthodontitis™ for malpositioned teeth as a more efficient way to identify the differential in bacterial flora as well as achieve a more effective, conservative and nonsurgical periodontal treatment of localized gingival recession. In the case of malpositioned anterior teeth, the resolution of periodontal disease should be the prerequisite to completion of orthodontic treatment.
The authors wish to acknowledge the contribution of Fastbraces® providers who provided the cases referenced in this paper.

©2019 Viazis, et al. This is an open access article distributed under the terms of the, which permits unrestricted use, distribution, and build upon your work non-commercially.