Journal of
eISSN: 2373-4345


Research Article Volume 6 Issue 1
1Lecturer & Consultant of OMFS, Faculty of Oral & Dental Medicine, Al-Azhar University, Egypt
2Clinical Associate Professor of Oral & Maxillofacial Surgery, Al-Azhar University, Egypt
3Chairman Cleveland Dental Institute (CDI), USA
4Consultant Oral and Maxillofacial surgery, Ganzoury hospital, Egypt
Correspondence: Mustafa G Khallaf, Department of Oral and Maxillofacial Surgery, AL-Azhar University, Egypt, Tel 1000399888
Received: October 07, 2016 | Published: January 12, 2017
Citation: Khallaf MG, Hegab A, Elrawy HF, et al. Evaluation of the effect of the biodegradable membrane on the outcome of immediate implant placement in the esthetic zone. J Dent Health Oral Disord Ther. 2017;6(1):11-15. DOI: 10.15406/jdhodt.2017.06.00186
Purpose: This study aims to evaluate the effect of the biodegradable membrane on the esthetic outcome following immediate implant placement in extraction sockets in the maxillary esthetic zone.
Patients and methods: The patients were randomly enrolled to one of two equal groups.
Results: Fourteen patients (9 female and 5 male) were enrolled in the current study and divided randomly into two equal groups. The patients age range from 24 to 43 (mean 31.5). There was non-significant difference in both groups in relation to age and gender. Statistical analysis of the crestal bone loss at six months postoperatively showed significant increase in crestal bone resorption in group one than group two (P value=0.0001). Regarding the soft tissue evaluation; the analysis Statistical of the data of soft tissue height above the implant revealed that the soft tissue in group two was thicker than that in group one (P value=0.00007).
Conclusions: Enhanced functional and aesthetic outcome of Immediate Implant Placement in the Esthetic Zone can be obtained by usage of the Biodegradable Membrane. The collagen membrane was effective in improving the soft tissue profile.
Keywords: immediate implant placement, extraction socket morphology, biodegradable membrane, esthetic outcome
Dental implant was placed to restore the function of the teeth as well as satisfactory appearance. A great challenge with implant placement and tooth restoration in the aesthetic zone has been presented as a common issue in tooth replacement. The ability of the dental team to re establish normal form and architecture to hard and soft tissue has been concerned.1 Originally, it was considered that complete healing of extraction socket had occurred before implant placement as a prerequisite for osseointegration that is called delayed implant. Later it has been shown that combination of extraction and implant placement can successfully be performed as a one-stage operation.2,3 This combination of demands could complicates the task of the surgeon while a reduced treatment period can be accomplished by immediate placement of the implant. However it makes the patients more satisfied especially from the esthetic point of view.4 The soft-tissue surgery involved in the procedure often produces a compromised aesthetic results these were presented as (broken mucogingival border, the adjacent papillae are destroyed and sometimes results in a buccal concavity, mucosal perforation, disintegration of the implant subsequently long healing period of both hard and soft tissue).5 Achieving an esthetically pleasing restoration involves not only harmonizing the size, shape, position and color of each prosthetic tooth with the adjacent teeth; but establishing a stable peri-implant tissues compatibility with the surrounding gingiva and mucosa is also essential. So the aim of this study to avoid this by placement of biodegradable membrane that cover the implant and guide the soft tissue for healing progression.
Patients with teeth indicated for extraction in aesthetic zone were selected from those attended the outpatient clinic of Oral and Maxillofacial Surgery Department of Al-Azhar University Hospitals. Inclusion Criteria: General health satisfactory, Single-tooth replacement in the maxillary anterior segments, Non-adjacent implant sites and prosthetic restorations, Patient will not wear any kind of removable prosthesis over the treatment area, Availability of complete clinical records. While Exclusion Criteria includes: Uncontrolled diabetes, Immunodeficiency diseases, Heavy smokers, untreated periodontal disease.
Diagnosis and treatment planning
Diagnosis and treatment planning are key factors in achieving successful outcomes after placing and restoring implants placed immediately after tooth extraction. Following some or all of the following suggestions, depending on individual circumstances, should be considered when evaluating a patient for dental implants: thorough medical and dental histories, clinical photographs, study casts, periapical and panoramic radiographs as well as cone beam computed tomography (CBCT) of the proposed implant sites. The Soft Tissue Assessment was done using: Indirect Cast Technique and Peri-implant Probing.
Allocation
The patients were randomly enrolled to one of two equal groups.
Marginal bone level: The standardized radiographs were used by Kodak software program to calculate:
Statistical analyses, including descriptive statistics for all clinical and radiographic parameters, were performed during the entire follow-up period. Implant clinical measurements were calculated by averaging the readings of each implant parameter for each patient, because the within patient variation was much lower than among patient variation. Subsequently, the means and medians were calculated among the means per patient at each study time point. The comparison within the group among the different time points was performed with dependent Student t test (statistically significant at a level of a=0.05). The P value was set at <0.05 with the Bonferroni corrections for multiple comparisons. All the data were analyzed using dedicated statistical software.
Fourteen patients (9 female and 5 male) were enrolled in the current study and divided randomly into two equal groups. The patients age range from 24 to 43 (mean 31.5). There was non-significant difference in both groups in relation to age and gender. The analysis of the data of crestal bone resorption was done preoperative, immediately, one, three and six months postoperatively, the preoperatively measurements of the alveolar and immediate post operatively was compared with each other to assure that there was no loss during surgery. Statistical analysis of the crestal bone loss at six months postoperatively showed significant increase in crestal bone resorption in group one than group two (P value=0.0001) (Table 1) (Figures 1–5). Regarding the soft tissue evaluation; the analysis Statistical of the data of soft tissue height above the implant revealed that the soft tissue in group two was thicker than that in group one(P value=0.00007). While the Statistical analysis within group two revealed that there was a clinically significant difference between thin and thick biotype after using a membrane. In terms of; the patients with thin biotype have gained a thicker biotype after treatment. Comparing both groups, in the preoperative stage, there was insignificant difference between mean values of the soft tissue height between the two groups while in the post-operative stages group II showed statistically significant higher values than group I at 1, 3 and 6 months(P value=0.009501, 0.000194, 0.00007 respectively) (Table 2) (Figures 5–10).
Crestal bone resorption |
Group I (No=7) |
Group II (No=7) |
T Test |
P Value |
One month after |
1.64±0.38 |
1.00±0.41 |
3.05 |
0.0099 |
Three months after |
3.07±0.35 |
1.43±0.35 |
8.9 |
0.0001 |
Six months after |
3.14±0.24 |
1.57±0.35 |
9.83 |
0.0001 |
Table 1 Crestal bone resorption for the study groups
The mean difference is highly significant if P value > 0.01

Figure 1 Preoperative intraoral picture of patient with congenitally missed upper lateral incisors and retained deciduous canine teeth.

Figure 4 Intraoral picture of the elevated flap with exposure of the surgical site in the left side.
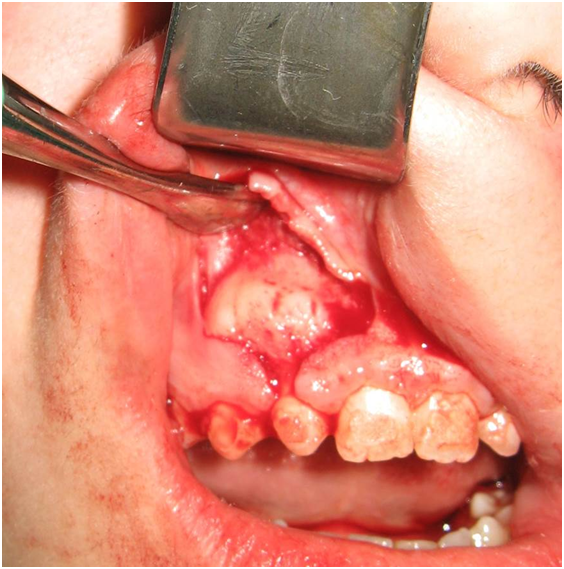
Figure 5 Intraoral picture of the elevated flap with exposure of the surgical site in the right side.
|
Mean±St Dev |
"T" |
Prob. |
|
Group I |
Group II |
|||
Pre |
2.53±0.61 |
2.14±0.75 |
1.057 |
0.155635 |
1 M |
2.86±0.56 |
3.93±0.89 |
2.709 |
0.009501 |
3 M |
2.71±0.57 |
4.36±0.69 |
4.867 |
0.000194 |
6 M |
2.50±0.58 |
4.29±0.64 |
5.499 |
0.00007 |
F |
0.589 |
13.626 |
||
Prob |
0.0628 |
0.00002 |
||
LSD |
0.638 |
0.823 |
|
|
Table 2 Soft tissue height for cases in both groups
The mean difference is highly significant if P value > 0.01
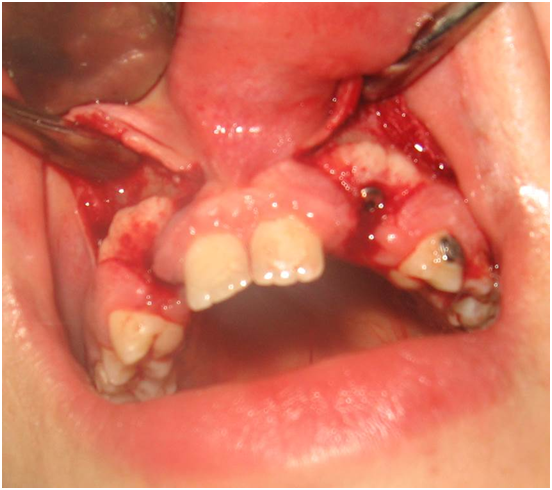
Figure 6 Intraoral picture of the elevated flap with exposure of the surgical site with extraction of the deciduous canine teeth and immediate implant insertion.

Figure 8 Intraoral picture after exposure of the dental implants showed improve the gingival biotype.
The gingival biotype should be assessed because such an assessment will partly determine the risk for postsurgical recession. The long-term stability of esthetic soft tissue around an implant restoration depends largely on the presence of adequate soft tissue volume in a vertical and buccolingual direction. An adequate volume of soft tissue provides a good emergence profile of the implant restoration and serves to mask the underlying metal implant, especially when combined with suitably apical placement.6 Two different periodontal biotypes have been described in relation to the morphology of the interdental papilla and the osseous architecture: The thin scalloped periodontium and the thick flat periodontium. A thick soft tissue biotype is a desirable characteristic that will positively affect the esthetic outcome of an implant-supported restoration because since it is more resistant to mechanical and surgical insults; it is less susceptible to mucosal recession and has more volume for prosthetic manipulation7 The choice for placement of collagen membrane in immediate implant increasing attention in esthetic zone to preserve the soft & hard tissues. This concept was based on the capability of the collagen membrane to guide the soft tissue during the healing period from the outer smooth surface moreover it holds the blood clot in high level from the inner rough surface.8 In present study the marginal bone loss was different between both groups. A mean of 0.8mm marginal bone loss was developed in group II which is coincided with Adell et al.9 However the study was not use periosteal flap which affect the crestal bone loss. A significantly higher bone to implant contact in presence of collagen membrane and holding the blood clot in high level may be good explanation for minimizing the crestal bone loss in group II.10 The clinical use of collagen membranes for peri-implant bone regeneration has resulted in better preservation of marginal bone level.11 Cases without membranes developed marginal bone loss mean of about 1.7mm which is not coincided with adell study.9 Consequently the difference between the two groups was attributed to presence of collagen membrane and it was obvious that the collagen membrane affect the crestal bone resorption around the implant. The soft tissue profile in group two was better than that in group one along the time. There was no change in group two in patients with thick soft tissue biotype while the change was observed with thin biotype after follow up periods as they gained thicker soft tissue while patients with thin biotype in group one developed a mucosal recession that may reflect the ability of the collagen matrix to enhance and promote the healing of soft tissue within limits. Different authors reported that there was no clinically significant difference in buccal gingival height around single implant before and after implant in patients with thick biotype which is coincided with this study.12 The role of collagen matrix (C.M) to augment the keratinized tissue around the implant increases the thickness of soft tissue six months after prosthesis by a mean of 2.6mm.13,14 A parallel result was obtained from the present study concerning the conversion of thin biotype to thick biotype. The gained amount of soft tissue was presented as 2 mm thickness in soft tissue, while the lake of soft tissue thickness in two cases may be attributed to the short term degradation of C.M with high enzymatic activity. Ins bite of that it preserved the soft tissue level. The papillae height was decreased with a mean of 0.52mm in patients without membrane, while in group two showed a mean of 0.45mm this was coincided with kan and conelini.15,16 This difference in the amount of papillae height reduction could be explained by the use of membrane that preserves the crestal bone and the covering soft tissue as well. Moreover the use of esthetic flap may play an additional role in preservation of the papillae along the time intervals.
Enhanced functional and aesthetic outcome of Immediate Implant Placement in the Esthetic Zone can be obtained by usage of the Biodegradable Membrane. The collagen membrane was effective in improving the soft tissue profile especially in patients with thin biotype and preserving the soft tissue profile in patients with thick biotype. Moreover the membrane was effective in decreasing the rate of crestal bone loss around the dental implant in patients with thin and thick soft tissue biotype.
None.
None.
The authors declare there is no conflict of interests.

©2017 Khallaf, et al. This is an open access article distributed under the terms of the, which permits unrestricted use, distribution, and build upon your work non-commercially.