Journal of
eISSN: 2373-6437


Mini Review Volume 6 Issue 4
Professor of Anesthesiology, Case Western Reserve University, Staff Anesthesiologist, UAE
Correspondence: D John Doyle, Professor of Anesthesiology, Case Western Reserve University, Staff Anesthesiologist, Department of General Anesthesiology, Cleveland Clinic Foundation, Chief, Department of General Anesthesiology, Anesthesiology Institute, Cleveland Clinic Abu Dhabi, UAE
Received: March 30, 2016 | Published: December 20, 2016
Citation: Doyle J (2016) Jet Ventilation for Otolaryngologic Procedures - A Mini-Review. J Anesth Crit Care Open Access 6(4): 00236. DOI: 10.15406/jaccoa.2016.06.00236
Jet ventilation is frequently used in the anesthetic management of Otolaryngologic procedures where the presence of an endotracheal tube would interfere with the surgery, as with some vocal cord lesions. (Where an endotracheal tube can be used, a narrow-bore microlaryngeal (MLT) tube (Figure 1) is often used; such a tube typically has an inner diameter of 5mm, compared to a conventional endotracheal tube with an inner diameter between 7 and 8.5mm). This mini-review presents the essential issues in using jet ventilation methods for otolaryngologic procedures where an endotracheal tube must be avoided.

Figure 1 A typical microlaryngeal (MLT) endotracheal tube (bottom) with a pediatric endotracheal tube (top) for comparison. Such a tube typically has an inner diameter of 5mm, compared to a conventional adult endotracheal tube with an inner diameter between 7 and 8.5mm. While the small diameter of the MLT endotracheal tube allows improved surgical access to the glottic structures, in some cases even narrow bore endotracheal tubes such as the MLT interfere with surgical access to the glottic structures, necessitating the use of a tubeless anesthetic technique such as jet ventilation. Image credit: http://www.howequipmentworks.com/wp-content/uploads/2015/01/mlt_paeds.jpg
Ventilation techniques
Two main techniques are available for jet ventilation for otolaryngologic procedures:1 use of a simple hand-held device and2 use of an automatic jet ventilator system. In both cases the usual gas delivered is 100% oxygen, but because of the Venturi effect resulting in the entrainment of room air, the oxygen concentration of the resulting mixture is less than 100%.
Simple hand-held jet ventilation devices: In the case of the hand-held device such as the unit shown in Figure 2 the operator starts operation with a driving pressure set to about around 20 psi1(in adults) and provides manually delivered jets of a little under one second duration delivered approximately 10 to 20 times a minute. In most cases the jet ventilation apparatus is attached to an anterior commissure laryngoscope or other type of otolaryngologic laryngoscope via a screw attachment (Figure 3) to provide supraglottic ventilation. The main means of determining that ventilation is adequate is to watch the chest rise with each delivered jet pulse. For safety reasons the driving pressure should be adjusted down to the minimum needed to achieve adequate chest excursions. Note that obese individuals require higher driving pressures to achieve adequate chest excursions as compared to lean patients.

Figure 2 The Manujet III (VBM Medizintechnik GmbH, Germany) is a portable and easily adjusted medical device that can be used for manual jet ventilation. A color-coded gauge shows the proving pressure in bar and psi units. The gas driving pressure can be adjusted between 0 and 3.5 bar (0 to 50 psi). Note that 50 psi of driving pressure is in the range of 3500cm H2O and so can readily produce barotrauma (e.g., a pneumothorax) if not used with caution. Most of the time a driving pressure in the range of 20 psi or less is used. Image Credit: https://www.medizintechnik24.com

Figure 3 An anterior commissure laryngoscope for use in otolaryngologic procedures. Such laryngoscopes are commonly used in conjunction with a hand-held jet ventilator such as that shown in Figure 2, but in some cases jet ventilation can be avoided by using a narrow bore endotracheal tubes such as the MLT endotracheal tube (Figure 1). Image Credit: http://www.teleflexsurgicalcatalog.com/surgical/pilling/products/4007
Automatic jet ventilation systems: In the case of an automatic jet ventilator system, a commercial product such as that provided by the Acutronic company may be used to provide infraglottic ventilation (Figure 4). This is usually achieved in conjunction with an infraglottic ventilation catheter (Figure 5). Table 1 lists a set of ventilation parameters that are commonly used with such a unit. Note that the ventilation rates for infraglottic automatic jet ventilation systems are usually much higher (in the range of 100 per minute and upwards) than for the supraglottic manual jet ventilation systems shown in Figure 2 (which typically operate in the range of 10 to 20 breaths per minute).

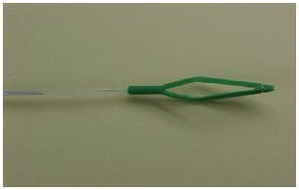
Figure 5 The Hunsaker Mon-Jet infraglottic ventilation catheter. Image Credit: https://www.aagbi.org. Note that an instructional video demonstrating the use of the Hunsaker Mon-Jet infraglottic ventilation catheter can be seen online at https://www.youtube.com/watch?v=51Y9O-xr7Dg
Anesthetic technique
After the induction of general anesthesia with propofol and muscle relaxation achieved with a paralytic such as rocuronium, anesthesia is maintained using a total intravenous (TIVA) technique such as a propofol infusion delivered at an initial rate of 100mcg/kg/min in conjunction with a remifentanil infusion delivered at an initial rate of 0.1mcg/kg/min. These infusions are then adjusted based on the factors such as the hemodynamics and the depth of anesthesia as guided by clinical findings and (commonly, but not always) by electroencephalographic (EEG) analysis.
In some centers it is common to add 1mg of remifentanil to 500mg (50ml) of propofol and treat the combination as “superpropofol”, delivering it in a single syringe at an initial rate of 100mcg/kg/min of propofol. When 100mcg/kg/min of propofol is delivered in this scheme, the resulting rate of remifentanil infusion is then 0.2mcg/kg/min. This latter arrangement has the advantage that only a single syringe pump is needed, but has the disadvantage that the two infusions cannot be independently adjusted.
Complications
Most complications associated with the use of jet ventilation are due to use of a high pressure of the delivered gas source. In particular, barotrauma leading to pneumothorax, pneumomediastinum, or other problems can result from the high pressures used, which can run as high as 50psi (=3500cm H2O pressure). This is particularly true if gas trapping due to inadequate expiratory pathway takes place.
Take-home points
Driving pressure (DP) |
1.0 bar |
Pause pressure (PP) |
20 mbar |
Peak inspiratory pressure (PIP) |
35 mbar |
Inspiratory time |
50% |
Frequency (respiratory rate) |
100/min |
Oxygen concentration (FiO2) |
100% |
Table 1 Typical settings used with the Acutronic Monsoon III jet ventilator
(https://www.acutronic-medical.ch/products/monsoon-iii.html).
Insertion of jet ventilator catheters (https://www.youtube.com/watch?v=_FXP-MADWYs). |
Jet oxygenation (https://www.youtube.com/watch?v=QR7ek7VBNiQ). |
Hunsaker Mon-Jet Ventilation catheter for Microlaryngoscopy (https://www.youtube.com/watch?v=51Y9O-xr7Dg). |
Table 2 Helpful instructional videos on jet ventilation
None.
The authors declare there are no conflicts of interest.
None.

©2016 Doyle. This is an open access article distributed under the terms of the, which permits unrestricted use, distribution, and build upon your work non-commercially.