International Journal of
eISSN: 2381-1803


Research Article Volume 15 Issue 1
1 Department of Anesthesiology, Hospital Universitari Dexeus, Spain
2 Medical Director Energimed, Dexeus Woman’s Health, Spain
3 Department of Gastroenterology, Hospital Universitari Dexeus, Spain
4 Department of Surgeon, Hospital Universitari Dexeus, Spain
Correspondence: Carvajal R Gilda, Department of Anesthesiology, Hospital Universitari Dexeus, Spain
Received: March 13, 2021 | Published: January 10, 2022
Citation: Gilda CR, Giralt I, Espinet E, et al. Inflammatory duodenal pseudostenosis acupuncture treatment. Int J Complement Alt Med. 2022;15(1):5-7. DOI: 10.15406/ijcam.2022.15.00583
We report the case of 31years old male patient, who as result of surgical extirpation of Gastrointestinal Stroma Tumor (GIST) in duodenum, a large number of different complication were present. The most patient life threatening one was inflammatory duodenal Pseudostenosis, because the patient was emaciated, western medicine did not offer an effective treatment. 10 acupuncture sessions were scheduled and both local points (segmental) and distal points was used.
The patient had a very satisfactory evolution in the first 4 sessions, the normal GI peristalsis function appeared again, nausea, vomiting and the fullness sensation disappeared as well. So, Acupuncture could be part of the therapeutic arsenal as a complementary treatment in this type of patients.
Acupuncture is beneficial as a complementary therapy for the management of chemotherapy induce nauseas,1 postoperative nauseas and vomiting,2 peptic ulcer disease3 and postoperative ileo4 as well as others functional disorders,5,6 including irritable bowel syndrome7 constipation8 and diarrhea.9 The effects of acupuncture occur through regulation of gastrointestinal (GI) motility, protection of the stomach mucosa and decrease in visceral sensitivity.11,12 For example acupuncture ST 36 Zuzanli a classic acupoint, may improve upper and lower abdominal symptoms and restore impaired gastric slow waves, which are induced rectal distension by vagal pathway.12 Moreover, electro acupuncture (EA) in the foot Yang Ming meridian may enhance motility and improve gastric mucosal blood flow by regulating the concentration of motilin and somastostatin in sinus ventriculis and bulbus medullae.13 GI motility maintains healthy digestive function through the contraction and expansion of smooth muscle in different section of GI tract; the characteristic motility pattern in the interdigestive period is referred to as an interdigestive migrating contraction. Acupuncture may have regulatory effect on GI motility.
Case description
We present a 31-year-old man (Body mass index BMI=35, 14Kg/m2) sedentary, no smoking, who received surgery on May 2015, for a Gastro Intestinal Stroma Tumor (GIST) in the duodenum 3rd portion. After that, he presented several complications (pancreatic pseudocyst, hematoma), and required other surgical interventions, and treatments in Intensive Care with blood transfusion.
After the Intensive Care and during his recovery in the hospital, he presented continuous nauseas and vomiting, as well as belching and epigastric pain. Fibro gastroscopy was performed on several occasions under anesthetist sedation, with the diagnosis of INFLAMMATORY DUODENAL PSEUDOSTENOSIS which was partially rectified with the endoscopy tube.
After this intervention the doctors decided to maintain an expectant management. Acupuncture treatment was proposed, and the treatment started in November the 30th 2015 after the patient signed the informed consent.
At the beginning of the treatment, the patient was week and with weight loosed, approximately 50Kg (initial weight 105Kg BMI 32,8); he was depressed, and he presented vomiting up to 6 times per day, constant belching, and gastric fullness sensation. He had to sleep semi-seated (45o). The tongue was pale and pulse empty. Interestingly, temperature below the scar was less than the above.
Diagnosis
According to Syndromes in Chinese Medicine the patient suffered a Qi deficiency of Spleen, a Blood Deficiency and a Liver Qi Stagnation.
Acupuncture treatment
We started the acupuncture treatment with 2 sessions per week, for 2weeks.
After that 1 session per week for 5weeks and later 1 session every 15days for 3 sessions.
Finally, a session monthly during 2months.
Every session lasted 30minutes.
The points we have been using are
Around the abdominal scar: Ren Mai 15,12,4, SP 21, Lv 13 and 14, St 22 and 25 Figure 2.
Distal: St 36,37,40,41 and 44, Sp 6, LI 4, Lv 3, PC 6, GB 13, Ren Mai 17.
Back Shu points: BL 20,21 y 23.
The patient had a very satisfactory evolution in the first 4 sessions, the normal GI peristalsis function appeared again, nausea, vomiting and the fullness sensation disappeared as well. Gradually, He could be eating with good tolerance of food, progressively gained weigh until 78Kg (March 2016). His mood is improving and he regained strength and endurance. He returned to his job in April 2016 and He returned to his normal nutritional status BMI 24,44
In the present report, the patient exhibited a large improvement in GI motility after the acupuncture treatment. Acupuncture promotes gastric peristalsis in subjects with low initial gastric motility, because it has a regulatory effect on the gastrointestinal motility.14 Acupuncture has a neuromodulation effect in the gut.15 Some Acupuncture points in the limbs promote gastric motility via supra-spinal reflex by activation of the sympathetic nerve fibers.16,17 Acupuncture may be helpful in retouring GI barrier injury by regulating the neuro-endocrine-immune system and antagonizing the inflammatory response (Figure 3).18
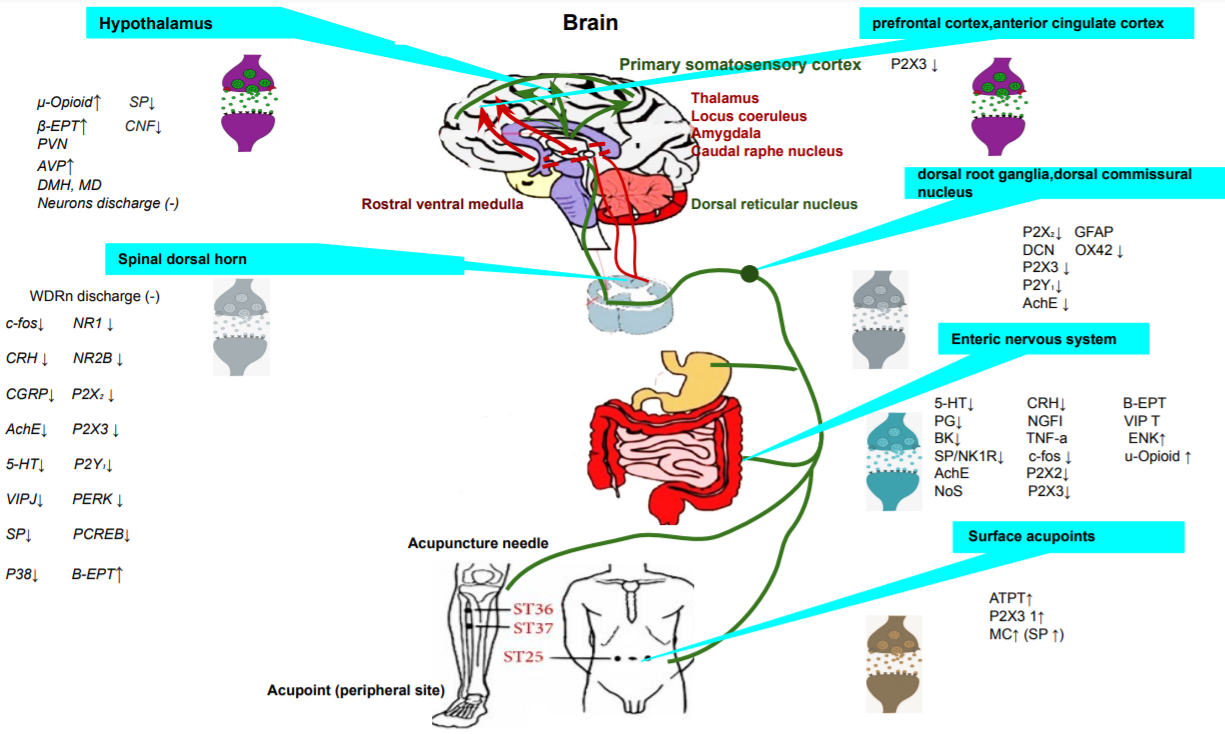
Figure 3 Ascending and descending pathways of the endogenous pain modulation system mediating visceral pain sensation in the brain-gut axis.
AVP, arginine vasopressin; CNF, corticotropin releasing factor; GFAP, glial fibrillary acidic protein; WDR, wide dynamic range neurons; BK, bradykinin; PG, prostaglandins; β-EP, β-endorphin; (−), inhibition of cell discharge; NTS, nucleus of the solitary tract; TNF-α, tumor necrosis.
We present a case report where Acupuncture has been used as an adjunctive treatment for GI dysfunction diseases, however the underlying mechanisms have not been clearly understood. We discuss the regulation GI function through the acupuncture from the perspectives of GI motility, the GI barrier, visceral sensitivity, attenuated inflammatory response (reduction of TNF-α and IL-β levels).19 According a classical acupuncture theory, some acupoints are important to regulate reflex visceral function, the most important are: ST 36, PC6, ST 37, RM 12 and ST 25.
In this regulatory effect both sympathetic and parasympathetic nervous systems are involved to active gut’s motor and secretory fibers.
With the experience limited to only one case but DUE to the highly positive results in a very serious case We can conclude that Acupuncture could be part of the therapeutic arsenal as a complementary treatment in this type of patients.
This is a case report from my private clinic thus ethical approval was not required.
None.
Author declares there are no conflicts of interest.
None.

©2022 Gilda, et al. This is an open access article distributed under the terms of the, which permits unrestricted use, distribution, and build upon your work non-commercially.