International Journal of
eISSN: 2381-1803


Mini Review Volume 16 Issue 1
1Shikoku Division of Integrative Medicine Japan (IMJ), Tokushima, Japan
2Tokushima University / Medical Research, Tokushima, Japan
3Shikoku Music therapy Association, Tokushima, Japan
Correspondence: Hiroshi BANDO, Tokushima University / Medical Research, Nakashowa 1-61, Tokushima 770-0943, Japan
Received: January 12, 2023 | Published: January 30, 2023
Citation: Bando H, Yoshioka A, Bando M, et al. Clinical effect of sound sleep support sound player “Lullaby reverberation;” for sleep quality. Int J Complement Alt Med. 2023;16(1):32-35 DOI: 10.15406/ijcam.2023.16.00628
Clinical effectiveness of sedative music on sleep quality was investigated. Subjects were 14 females aged 40s to 70s, and methods included listening to music during going to sleep using by sound sleep support sound player “Lullaby reverberation (Komoriuta-no-Hibiki)”, which was evaluated by Pittsburgh Sleep Quality Index (PSQI) in 0,4,8 weeks. Thirteen cases showed decreased points of PQSI. Time to sleep and sleep duration were almost the same. The relationship figure for PSQI and time until sleeping showed general tendency of left and horizontal/lower directional arrows. These results suggest positive beneficial effect of music for sleep quality evaluated by PSQI.
Keywords: sound sleep support sound player, Lullaby reverberation, Pittsburgh sleep quality index PSQI, music therapy, integrative medicine japan, IMJ
For decades, Complementary and Alternative Medicine (CAM) and also Integrative Medicine (IM) have become important fields in actual medical practice.1 Authors and collaborators continued various research on CAM and IM associated with the management of Integrative medicine Japan (IMJ), Shikoku Island division, Japan.2,3 Some areas have been especially included such as low carbohydrate diet (LCD), rehabilitation medicine, art therapy, music therapy and others.4,5 In CAM and IM, pharmacological and non-pharmacological treatments have been in focus. In the latter, several therapeutic kinds have well-known, including music therapy, aromatherapy and related treatments.6
Sleep disturbance has been common and important problem for lots of people. For its practical treatment, non-pharmacological interventions such as music therapy have been known as promising method to address sleep disturbance. A systematic review was conducted for examining the efficacy of music interventions on sleep problems.7 Consequently, mixed evidence was shown for effect of music interventions. They included relaxing music choice and personalizing music selection from each preference.
Sleep would be vital for human well-being and persisting health. In contrast, sleep disturbance is comorbid to various physiological and psychological disorders.8 From several studies, music has some power to improve sleep quality, but it includes equivocal results of several parameters. The clinical response differs for each person, because the sensitivity is different for music, art and so on. For therapeutic purpose, music can be classified into two categories. The sedative music is usually characterized for its smooth melody and slower tempo.9,10 In contrast, rhythmic music has faster tempo, rhythmic pattern and louder volume and loudness.11
For improving sleep quality, some reports were observed concerning non-pharmacological interventions.12 As to primary outcome, the total score of Pittsburgh Sleep Quality Index (PSQI) was applied before and after musical interventions. PSQI is known for its validity, and significant improvement was found by PSQI score. Thus, some interventions of listening to music and sleep hygiene showed efficacy for sleep quality. Similarly, authors have conducted the research for clinical effect of music on sleep. General situation and some perspectives will be described in this article.
The subjects for this study were 14 females, whose age was from forties to seventies. The average age was 61.6 +/- 12.0 years (mean+/-SD). The detail situation showed that 2 person in their 40s, 4 in 50s, 4 in 60s, and 4 in 70s. Subjects were asked for volunteer condition associated with some fundamental points. They can lead a regular life, and can listen to the music during going to bed, or do not have small children to take care at home. They are medical and welfare staffs from hospitals and related our medical associations. The condition of listening to music every night satisfies the conditions such as being able to afford it.
The music apparatus was a sound sleep support sound player “Komoriuta-no-Hibiki” which means Komoriuta (=lullaby) + no (=of) + Hibiki (= sound, reverberation, echo) (Figure 1). It was produced by collaboration of Avex Co. Ltd, Japan13 and Ide sound Institute.14 Its shape is cubic with about 8.5cm in size. It is an instrumental player with more than 65 various kinds of music totally 6 hours. They include popular music, classic music, sound of water, waves, wind, and so on. Especially, lullaby music contains several well-known piano-playing, such as the works of Shubert, Schumann, Fauré, Ravel and Granados. The quality of sound would be supreme for sleeping music.

Figure 1 General view of novel music instrument.
It is the sound sleep support sound player “Komoriuta-no-Hibiki”
The protocol was to continue listening to sound of lullaby every night for 8 weeks. They were asked to answer the questionnaire of sleep condition for 0 week, 4week and 8week. For sleep evaluation, the Pittsburgh sleep quality index (PSQI) has been known. We used Japanese version of PSQI as PSAI-J for this study. PSQI has mainly 8 aspects for sleep problems (Table 1).15 When evaluating sleep conditions, several items are answered. They include sleeping time, awaking time, time to sleep (min), sleeping duration (hours), and 8 main questions. For each question, the answer is evaluated as point 0, 1, 2, 3, where 0 means no symptom or problem at all, and 3 means severe degree of symptom. When sleep problem is evaluated, each numerical value will be summed up.
1) |
Sleep quality |
2) |
Sleep latency |
3) |
Sleep duration |
4) |
Habitual sleep efficiency |
5) |
Sleep disturbances |
6) |
Use of sleeping medication |
7) |
Daytime dysfunction |
8) |
PSQI global score |
Table 1 Main items in PSQI
Subjects were evaluated by PSQI-J for 0, 4, 8 weeks. For 14 cases, time to sleep was checked and compared (Table 2). Among them, 2 subjects (cases a and m) showed remarkably prolonged time, but others showed almost no changes. As to sleep duration, the average sleep time was 6.4hr and 6.3 hr, in 0 and 8 week, respectively, suggesting no remarkable changes.
|
Age |
Case |
Age |
Time to Sleep (Min) |
Sleep Duration (Hr) |
|||
|
|
|
years |
0 week |
4 week |
8 week |
0 week |
8 week |
|
40s |
a |
42 |
10 |
40 |
60 |
7 |
6 |
|
|
b |
46 |
30 |
30 |
40 |
6 |
5 |
|
50s |
c |
51 |
10 |
10 |
10 |
6.5 |
6.2 |
|
d |
52 |
20 |
15 |
10 |
5 |
5.5 |
|
|
e |
55 |
10 |
10 |
10 |
6.5 |
6.5 |
|
|
|
f |
57 |
60 |
60 |
60 |
8.5 |
9 |
|
60s |
g |
60 |
30 |
30 |
20 |
5 |
6 |
|
h |
63 |
20 |
20 |
15 |
6 |
6.5 |
|
|
i |
64 |
10 |
10 |
10 |
7 |
7 |
|
|
|
j |
65 |
20 |
30 |
15 |
5 |
5 |
|
70s |
k |
75 |
5 |
10 |
10 |
6.5 |
6 |
|
l |
76 |
10 |
20 |
10 |
6.5 |
6.5 |
|
|
m |
78 |
30 |
30 |
60 |
6 |
6 |
|
|
|
n |
79 |
40 |
20 |
20 |
7.5 |
7 |
|
Average |
61.6 |
21.8 |
23.9 |
25.0 |
6.4 |
6.3 |
|
|
Stand.Dev. |
12.0 |
15.1 |
14.2 |
20.6 |
1.0 |
1.0 |
|
Table 2 Applicants and results related to sleep
The total points of PSQI-J questionnaire for 0-week and 8-week were calculated and also compared. Then, two numerical values on 0 and 8weeks were expressed by using arrows. Concerning the arrow, starting point/ending point of the arrow represents the values for weeks 0 /8, respectively. Using this method, the results of 14 cases in 40s, 50s, 60s and 70s were described in 4 groups of Figure 2. Regarding each point, less numerical value means less or no symptom of sleep problem in each case. Among 14 cases, only 1 case in 40s showed increased point, while 13 cases showed decreased point from 0 to 8 weeks. Consequently, almost all subjects have shown decreased sleep problems for 8 weeks during current intervention protocol of music listening for sleep.

Figure 2 Changes in Points for PSQI-J for 4 age groups.
Cases (n=14) were categorized into 4 age groups (40s, 50s, 60s and 70s), which is shown in x-axis. Total points for PSQI-J in 0 and 8 weeks were calculated and compared, which is shown in y-axis. The point of 0/8 weeks was represented by the arrow, where starting/ending point means the numerical number of 0/8 weeks, respectively.
The relationship between Points for PSQI-J and time period until sleeping for 0-8 weeks was investigated (Figure 3). It means x-axis for value of PSQI-J (pts), and y-axis for time until sleeping (min). Each case has two data of 0 week and 8 weeks. Those numerical values were shown by using the arrow. The starting and ending points of the arrow means the data of 0 week and 8 weeks, respectively. For x-axis, 13 cases in 14 cases showed left-directional arrows, indicating decreased value of PSQI-J. For y-axis, 2/14 cases showed remarkable increase, 2/14 cases showed a little increase, and 10/14 showed stable or rather decrease. This result indicates that about 70% of subjects showed decreased time until sleeping.
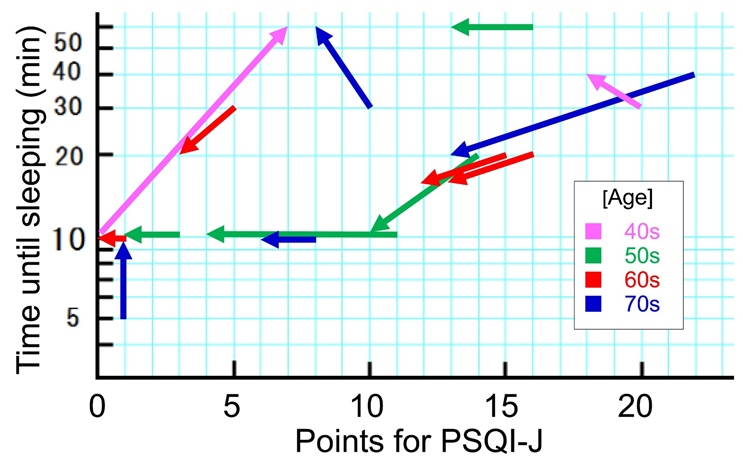
Figure 3 Relationship between Points for PSQI-J and time until sleeping during 0-8 weeks.
This figure has the analysis of the changes in 0 week and 8 weeks. It has x-axis and y-axis, which represents points for PSQI-J, and time until sleeping, respectively. Two points of 0 week and 8 weeks are changed into the expression of each arrow. The starting and ending points means the numerical values of 0 week and 8 weeks, respectively.
After Pittsburgh Sleep Quality Index (PSAI) was originally developed, the Japanese version of PSQI (PSQI-J) was presented.15. It has main 8 items to be evaluated, which are indicated for Table 1. Using PSQI-J, detail investigation was conducted for several diseases such as primary insomnia, major depression, generalized anxiety disorder, schizophrenia groups, and so on. As to various sleep disturbance, PSQI has been highly evaluated for its usefulness and validity. It is indeed that PSQI would clarify sleep problems, but it would be time-consuming due to large number of questions. Mutual relationship among PSQI, Athens insomnia scale (AIS) and Epworth sleepiness scale (ESS) was investigated as simple alternative questionnaires.16 For patients with chronic liver disease (CLD)(n=117), sleep disturbance was diagnosed as 33.3% in AIS, 31.6% in QSQI and 7.7% in ESS. No correlation was observed between PSQI and ESS scores. On the other hand, AIS scores and PSQI scores showed significant correlation (p<0.001, r=0.689).
Concerning relationship with music and sleep quality, various research was found. The subjects were applicants without sleep disturbance, and the method was random-effects meta-analysis method.17 Five data bases were analyzed and evaluated by GRADE (Grading of Recommendations Assessment, Development and Evaluation). As a result, 22 studies with 1514 cases were reviewed, and intervention of music for three weeks contributed the improvement of sleep quality. Improving sleep quality was investigated by the existence of music.18 Using Pittsburgh Sleep Quality Index (PSQI) questionnaire, 6 literatures were reviewed in comparison with audiobooks and passive controls. Generally, music amount or dosages tended to contribute the improvement of sleep disturbance. In a study, poor sleepers with PSQI >5pts showed healthier sleep with PSQI <5 points after receiving regular music intervention for 3weeks. The average improvement of PSQI revealed -1.15 pts per week, which suggests significant clinical efficacy of music for treating mild sleep disturbance.
Concerning the effect of music on sleep quality, the research was conducted for nurse students in Turkish university.19 The protocol included two groups, where one is listening to music 1 hour at most, another group is usual daily life without music listening. The results showed that PSQI mean scores in the experimental group were significantly lower than those in in the control group. For 70 pregnant women, effect of music before sleep was investigate.20 The groups were music group and control group and listening music for 30min each other day for 2weeks. The comparison was conducted for Pittsburgh Sleep Quality Index - 1week (PSQI-1 week) and Prenatal Comfort Scale (PCS). The results showed that significant difference for mean scores of PSQI-1 week was found between the two groups for PSQI-1 week. In contrast, no significant difference was observed for PCS scores.
In current study, we performed an intervention for listening to music using a small music player when going to sleep. For characteristic aspect, it contains a variety of sedative music for beneficial effect on sound sleep.21 The subjects were 14 women in their 40s to 70s with stable lifestyles who are staff members of medical institutions and medical societies. The results obtained suggested an overall trend for the efficacy of music on comfortable sleep.
Firstly, 13 out of 14 patients showed a decrease in PSQI-J total points over 8 weeks. This result indicated a reduction in sleep-related symptoms and problems.22 It was suggested that listening to music during sleep may bring a positive effect. When these 13 subjects were examined for the time period to sleep, 10 cases showed the same or slightly shorter. On the other hand, 3 cases showed longer, in which actual time was 5 to 10 min, 30 to 40 min, and 30 to 60 min, respectively. From these general situations, this intervention did not seem to affect time period to sleep.
Among 14 subjects, case a in her 40s showed a different reaction than the others. In other words, the response was completely opposite to those of the other 13 subjects. It showed the PSQI-J scores ranging from 0 to 7, and the time to sleep ranging from 10 to 60minutes. What has brought the results obtained? Probable answer was clearly recognized in the background of this case. She is a staff member of our research group, and also actually a semi-professional pianist. In normal subjects, listening to music during sleep is usually expected to act as a sleeping or lullaby. However, in her case, it would be the other way around. Since she is a music expert, she could not sleep because she concentrated on the detail music performance, tone color, and interpretation while listening to it.23 From mentioned above, such mechanism may bring more awake and stimulate her consciousness.
An impressive study was found, where better sleep quality was compared in older adults from 5 RCTs.24 Mean difference (MD) of PSQI points with significant difference was as follows: -1.96 pts between listening to music vs no listening group; -2.35 pts between sedative music vs rhythm-centered music; -2.61 pts for longer listening longer period more than 4 weeks, respectively. These data suggest clinical effectiveness of music on sleep quality, and further research with detail condition would be expected.25
Certain limitation exists in this study. The subjects were 14 females in 40s to 70s, which was not so many cases. The protocol and their actual listening and answering the questionnaires would be satisfactory. The evaluated content was the answer of PSQI, which was rather subjective feeling than numerical digital measurement.26 Consequently, further research in this area will be required.
In summary, clinical effectiveness of sedative music on sleep quality was investigated. A Sound sleep support sound player was applied to female subjects, and the study was conducted satisfactory. As a result, almost subjects showed improved sleep condition by PSQI. This report becomes hopefully a useful reference and research on music therapy will be expected to develop in the future.
None.
We declare there are no conflicts of interest.
None.

©2023 Bando, et al. This is an open access article distributed under the terms of the, which permits unrestricted use, distribution, and build upon your work non-commercially.