International Journal of
eISSN: 2381-1803


Review Article Volume 6 Issue 2
1Department of Cardiology, Institute of Hospitalization and Care with Scientific Address, Italy
2CRESO, School of Osteopathic Centre for Research and Studies, Gorla Minore (VA), Italy
3CRESO, School of Osteopathic Centre for Research and Studies, Falconara Marittima (AN), Italy
4Department of Radiological, Sapienza University of Rome, Italy
5Center for Life Nano Science@Sapienza, Istituto Italiano di Tecnologia, Italy
Correspondence: Bordoni Bruno, Foundation Don Carlo Gnocchi IRCCS, Department of Cardiology, Institute of Hospitalization and Care with Scientific Address, S Maria Nascente, Via Capecelatro 66, Milan 20100, Italy, Tel 349.6300617
Received: March 21, 2017 | Published: March 31, 2017
Citation: Bordoni B, Marelli F, Morabito B, Sacconi B (2017) Proposal for a New Osteopathic Treatment Method for the Eustachian Tube. Int J Complement Alt Med 6(2): 00184. DOI: 10.15406/ijcam.2017.06.00184
The Eustachian tube (ET) plays an important role in the function of the middle ear, stimulating drainage and ventilation. The drainage of secretions from the middle ear is carried out by the mucociliary system of the tube (and the mucus membrane of the middle ear), the muscular system of the tube and the tension of the tubal lumen. The ET is normally closed by periluminal pressure which is greater than the outside pressure, while it is rhythmically opened by muscle activity to which it is directly or indirectly linked. There are six muscles recognised as having an active role in the functions of the tuba: tensor veli palatini; levator veli palatini; tensor tympani; salpingopharyngeus; lateral and medial pterygoids. Literature available on an osteopathic approach to treating the ET is lacking. The article reviews the literature on the osteopathic treatment of the Eustachian tube and proposes a new hypothesis of treatment for a non-pediatric population. This may lead to new scientific findings and improved results to the patient's overall health.
Keywords: osteopathic, eustachian tube, otitis media, pterygoid muscles, temporomandibular joint
The Eustachian tube (ET) plays an important role in the function of the middle ear, stimulating its drainage and ventilation. The drainage of secretions from the middle ear and occasionally of foreign material is carried out by the mucociliary system of the tube (and the mucous membrane of the middle ear), the muscular system of the tube and the tension of the lumen tube.1 The ET is normally closed by periluminal pressure that is greater than the outside, while it is opened rhythmically by muscle activity to which it is directly or indirectly linked.2
This mechanism allows the ET to prevent the reflux of material and nasopharyngeal area pathogens into the middle ear, allowing for a smooth passage of air from the nasopharynx to the middle ear.2,3 The tympanic membrane, in order to perform its function well, must vibrate properly when sound passes through it. The ET intervenes so that there is an optimum pressure in the middle ear, managing the pressure using the air which passes through it.4 The bolus of air that comes into the middle ear will be partially absorbed by the blood vessels and mucosa.5 The ET is nourished by the ascending pharyngeal and meningeal arteries while venous and lymphatic drainage is carried out by the pharyngeal and pterygoid plexus respectively and the retropharyngeal lymph nodes.1
The ET is located in the parapharyngeal space and is closely associated with the infratemporal fossa. It extends from the front wall of the middle ear to the side wall of the nasopharynx, passing along the posterior edge of the medial pterygoid plate; proceeding forward and downwards and medially, to form a 45 degree angle with respect to the sagittal plane, and at an angle of about 30 degrees to the horizontal plane.6
In children, the orientation of the sagittal plane is less, averaging at around 10 degrees.7 It consists of a posterolateral osseous portion and one fibro cartilaginous anteromedial portion, with a length of about 3.5 centimetres.1,8 The three dimensional structure of the internal lumen is covered with epithelial cells coated by a viscous fluid, and periluminous mucous tissue.1 Entering it, it opens posteriorly and slightly below the posteroinferior nasal concho.1 The innervation of the ET is very complex. The pharyngeal ostium is affected by a pharyngeal branch of the maxillary nerve, the spine from the cartilage branch area arising from the mandibular nerve, while the osseous portion of the bone is affected by the tympanic plexus arising from the glossopharyngeal nerve.1
The intermittent opening of the pharyngeal ostium in the nasopharynx cause peristaltic-like movements, which are probably due to the visco-elastic nature of the tubular structure of the cartilage.3,8 Yet, the opening of the ostium happens as a result of intervention strategies by the muscles, although we do not know the exact timing of the intervention and the precise actions of the muscles that interact with the tube. During swallowing or opening the mouth, the ostium of the nasopharyngeal tube opens, balancing the air pressure in the middle ear and clearing it.3,5,8,9 There are six muscles recognised as having an active role in the functions of the tube: tensor veli palatini; levator veli palatini; tensor tympani; salpingopharyngeus; lateral and medial pterygoids. The tensor muscle of the soft palate (TVP) dilates the ET lumen, but is also considered a masticatory muscle, as it is active during chewing, swallowing (acting on velopharyngeal movement) and phonation, orienting the tube inwards.2,3,10,11
The mandibular branch of the trigeminal nerve is responsible for innervation.10 The TVP consists of an external and medial portion, the first of which originates from the spine of the sphenoid bone, the navicular fossa, the tensor tympani muscle and the lateral edge of the sulcus sphenoid. The medial portion comes from the middle third of the posterior-medial cartilage wall of the tube; the two areas descend and converge on the pterygoid halumus forming a strong tendon that curves around this process and is inserted horizontally into the soft palate as palatine aponeurosis.10 The TVP works closely with the tensor tympani muscle (TT), sharing the same innervation drivers.10 Its lateral surface is in direct contact with the surface of the anterior superior pterygoid medial muscle.6 With age, its strength declines with a change in its force vector and reduction in its range of motion.12
The elevator of the soft palate (LVPM) has a cylindrical shape and runs below the tube, entering into the cartilaginous portion and forming a sling with fixed inserts between the petrous apex of the temporal bone and the midline of the soft palate; it sits posteriorly and medially to TPV, with anatomical continuity.2,6,8 Its actions on tube are not in agreement with literature (on the subject) where it can be found to have an opening and closing role.2,3,13 It is innervated by the vagus nerve.6 The tensor tympani (TT) is a thin muscle, located outside the middle ear and along the tube, and is anchored to the sphenoid bone and the osseous portion of the tube; its distal tendon inserts on the malleolus in the upper, middle ear, involving the stirrup and the stapedius muscle.4,10,14 Its contraction assists and is simultaneous with the TVP, pulling the malleolus to dampen eardrum vibrations while swallowing and during mastication14 There is a fascia link between the TT and the TVP.10 It is innervated by the mandibular branch of the trigeminal nerve.14 The salpingopharyngeal (SP) is part of the internal and longitudinal pharyngeal muscles, contributing to the swallowing mechanism and is innervated by a branch of the vagus nerve.14,15 When it contracts together with the other two internal longitudinal muscles (stylopharyngeus and palatopharyngeus), it shortens the pharynx and elevates the larynx. The SP is borne from the cartilaginous portion of the tube, thin and small in size, in order to fit deeply into the pharynx (with many anatomical variables), having a close relationship with the palatine tonsil.16 There is limited data in the literature on the exact function of the SP, but it is believed to contribute to the opening of the tube, albeit in a minor way.13,17
The external or lateral pterygoid muscle (LP) and medial or internal pterygoid muscle (PM) belong to the group of muscles involved in mastication and in the function of the middle ear. The LP is formed by two muscle bellies or heads, upper and lower. Within in literature there are two other portions, the pterygoideus proprius and the pterygospinous, and other variations.18 The upper belly originates in the infratemporal surface and the crest of the greater wing of the sphenoid bone, while the lower belly originates from the lateral surface of the lateral pterygoid plane; both portions are oriented horizontally and posterolaterally.6 The muscle heads are inserted in the pterygoid fovea muscle under the condylar process of the mandible, with the upper portion of the LP continuing and attaching to the articular disc of the temporomandibular joint.6
The PM is found below the LP. The PM is thinner and quadrilateral in shape, crossing through the lower area of the infratemporal fossa.6 The PM has two heads, one deep and one shallow. The first originates laterally to the palatine pyramidal process and the maxillary tuberosity, passing superficially to the lower head of the LP, while the second
and wider one rises from the medial surface of the lateral pterygoid plate and the pterygoid fossa between the two pterygoid plates, to pass more deeply in respect of the lower portion of the LP. Both portions of the PM descend posteriorly and laterally to attach to the back and bottom of the medial surface of the branch and angle of mandibola. The PM is innervated by the mandibular branch of the trigeminal nerve.
Even in the case of the PM anatomical variations in the muscle may occur.19 Both the LP and the PM are involved in the horizontal movement of the mandible; the LP moves the mandible on the opposite side of its contraction while the PM pulls the mandible forward.20 The PM belongs to the group of the elevator muscles of the mandible, while the LP is part of the group of muscles that depress the mandible.21
Another feature attributed to the two mastication muscles, is to allow the peristaltic movement of the tube, in synergy with the LVPM and TVP (levator veli palantini muscles), during the process of swallowing; the same active movement of the LP and PM, even in the absence of swallowing, allows the tube to open.8 It is likely, their intervention alters the shape of the tube, which becomes more convex, allowing the muscles that act directly on the tube to provide greater force.8 Another explanation for their usefulness, for the PM in particular, is that they may act as fulcrum, so that the musculature of the tube acts as a more efficient vector.22,23
When the ET does not function properly in a chronic situation, many problems and diseases may be encountered. If the aeration of the tube fails; chronic cholesteatoma infections of the middle ear, delays in language learning in children due to hearing loss, chronic perforation of the eardrum and tympanic atelectasis of the cavity may be discovered.8 Other issues which may come to light are tinnitus, dizziness, hearing impaired sensations and myoclonus.10,14 The complications of chronic otitis media can affect both at intra-cranial level (meningitis, brain abscesses, thrombosis, extradural abscess, otologic hydrocephalus, encephalitis), as well as at extra-cranial level (facial nerve paralysis, mastoiditis, sub-periosteal abscesses, labyrinthitis).24 In children, in particular, acute otitis media is recurrent due to greater horizontalisation with a smaller tube diameter, than in adults, and it becomes easier to reflux from the nasopharynx, or due to a different structure of the tube cartilage.3,9,10 What literature offers on the approach to the osteopathic ET is meagre; there are no studies involving large numbers of patients, treatment is aimed at children with recurring acute otitis media, and the techniques used are varied and not intrabuccal.25-28 There is an article from 2008 describing an intrabuccal technique, with a case report included in the text. The technique is linked to an osteopathic intrabuccal approach designed by osteopath CH Muncie DO.1
The technique consists of placing a gloved finger inside the open mouth, until it touches the lower portion of the rear pillar of the palatine tonsil.
Once the area has been identified, the operator's finger goes up the cephalad and slightly to the side up to the Rosenmuller fossa (the rhino-pharynx), to the rear of the tube opening; the operator applies a pumping motion.1. The technique is extremely uncomfortable for the paediatric patient and it is doubtful that the finger can reach the nasopharyngeal tube area. The variant of the 'Muncie' approach, also reported in the same article, is to place the finger on the palatine tonsil; performing circular movements.1. The goal is to free the opening tube orifice. Another non-intrabuccal osteopathic technique designed by the osteopath WO Galbreath DO, is to mobilise the mandibular branch of the paediatric patient on the side of the non-compliant tube, presenting with recurring otitis media.7 The operator applies gentle rhythmic traction to the inferiolateral, with the patient seated, for a maximum of 3-5 seconds per manipulation and for a total maximum of 30-60 seconds; the aim is to stimulate venous and lymphatic drainage.7
The proposal of a new treatment method for the Eustachian tube with an intrabuccal approach, for a non-pediatric population, is borne out of the need to stimulate new research in osteopathy suggesting a technique that mirrors recent anatomical knowledge as a common basis for a starting point. With this in mind, it might lead to new scientific findings and better results for the patient's overall health. From recent scientific data on muscle interference aimed at tubal function, we know that the pterygoid muscles act to work synergistically with the contractile areas of the ET. Their involvement must be enabled and activated during intrabuccal techniques designed to better the function of the tube. This approach should not only address the paediatric population, but adults. As well. The method proposed here is an intrabuccal technique with active movement of the mandible, while the patient is seated.
The patient should be seated during treatment, as it has been noted the tube functions best in this position.8 The operator uses a gloved finger to reach the palatine tonsil on the side displaying the tube dysfunction; while the patient actively moves the mandible forward and finally moves it horizontally on the opposite side Figure 1.
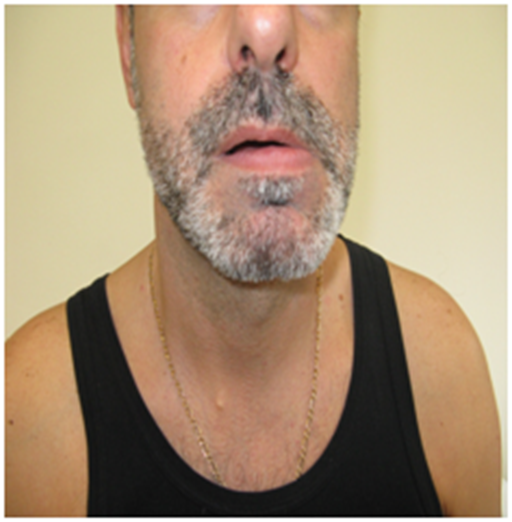
Figure 1 The patient actively moves the mandible forward and finally moves it horizontally on the opposite side.
The mouth is not fully open, but remains in a semi-open position, so that the intrabuccal finger is less uncomfortable to the person being treated and the transfer movement forward can be actively carried out on behalf of the patient and to the side of the mandible.
During the active movement of the patient, the operator's finger makes the circular movements, as for the modified 'Muncie' technique.1 Gentle finger pressure is applied for a few seconds, and then released from contact with the palatine tonsil, allowing the patient to relax. The duration of the treatment session will reflect the ability of the patient to endure treatment which is usually a few minutes. The patient undergoing this procedure must be able to actively move the mandible according to instructions from the operator; therefore paediatric patients not yet able to be cooperative are excluded. The technique should not only be used in cases of recurrent acute otitis media, but also for treatment of other tubal dysfunctions, as the tube has elastic properties, and stimulating its opening using with active muscle movements could help the well-being of the patient.8 (Figure 2).
The Eustachian tube (ET) plays an important role for the function of the middle ear, stimulating the drainage and ventilation. The muscles that affect the smooth functioning of the ET include contractile areas used not only within the auditory sphere, but also those belonging to mastication functions such as the pterygoid muscles. A feature attributed to the two mastication muscles, is to allow the peristaltic movement of the tube, in synergy with the LVPM and TVP (levator veli palantini muscles), during the process of swallowing; the same active movement of the LP and PM, even in the absence of swallowing, allows the tube to open. There are very few texts available within the body of scientific literature in the field of tube treatment and research in particular has only been conducted in the field paediatrics. The proposal of a new treatment method for the Eustachian tube with an intrabuccal approach is borne out of the needed to stimulate new research in osteopathy, suggesting a technique that mirrors recent anatomical knowledge as a common basis for a starting point. With this in mind, it may lead to new scientific findings and improved results to the overall health in patients. It is hoped that scientific research is stimulated by new perspectives raised in this article.
None.
None.
The authors declare that there are no conflicts of interest.

©2017 Bordoni, et al. This is an open access article distributed under the terms of the, which permits unrestricted use, distribution, and build upon your work non-commercially.