International Journal of
eISSN: 2381-1803


Research Article Volume 4 Issue 5
1Department of Radiation Oncology, University of Virginia School of Medicine, USA
2Department of Statistics, University of Virginia, USA
3Center for the Study of Complementary and Alternative Medicine, University School of Nursing, USA
4Empirical Technologies Corporation, USA
Correspondence: Tyvin Rich, MD FACR Hampton University Proton Therapy Institute 40 Enterprise Parkway Hampton, USA
Received: October 29, 2016 | Published: December 21, 2016
Citation: Rich T, Pfister R, Alton J, Gerdt D, Baruch M (2016) Assessment of Cardiovascular Parameters with the CareTaker Device during Meditation. Int J Complement Alt Med 4(5): 00135. DOI: 10.15406/ijcam.2016.04.00135
Introduction: Cardiovascular parameters like heart rate variability and blood pressure can now be measured with minimal physical impact and were used to study a group of volunteers who practice meditation.
Methods: Volunteer subjects were instructed to wear a tiny digital artery pressure sensor designed to measure blood pressure and heart rate. Subjects were observed during a general rest interval and then instructed to meditate. The individual meditation practice was accompanied with either reverse abdominal or a form of non-specific breathing technique for about 15minutes. Cardiovascular parameters were compared prior to and during meditation in the same subject.
Results: The comparisons between rest and meditation in each subject generally showed greater variance of blood pressure and heart rate variability with the latter. A spectral analysis showed the emergence of a low frequency parameter with meditation and is consistent with previous observations of LF during various forms of meditation. The subjects practicing RE had a large shift in LF compared to practioners of non-RE meditation.
Summary: In this exploratory study of experienced meditators, an LF HRV increase, generally considered to be a marker of autonomic balance in the literature, emerged more prominently in one group. The social context of the subject may influence the degree of shift in the LF and the type of practice of meditation, possibly related to the breathing technique used during meditation.
Keywords: cardiovascular parameters, transcendental mmeditation, hypertension, heart rate variability, antihypertensive, caretaker device, median absolute deviation, lomb-scargle
HRV, heart rate variability; RE, reflective exercise; CT, care taker; MAD, median absolute deviation
Meditation is popularly known for its healing and spiritual aspects and is derived from ancient traditions of India and the martial arts of China.1 Recognized branches of meditation today are mantra (Transcendental Meditation and Benson’s Relaxation Response) and Mindfulness Meditation,2 Yoga,3 and the practices of Tai Chi & Qi Gong.2 These forms of meditation are increasingly used as a complementary mind/body therapeutic strategy for chronic diseases like hypertension, cardiovascular diseases and substance abuse; cancer patient’s constitutional symptoms and a variety of stresses of modern life have also been addressed with meditative approaches.2
There is growing interest in exploring measurements of cardiovascular dynamics in subjects who meditate because the practice lowers elevated blood pressure.4 These observations have prompted continued assessment of heart rate variability (HRV) in subjects during meditation in order to gain further understanding of the interactions of autonomic parasympathetic and sympathetic regulation as related to practice. For example, very prominent LF (0.1HZ) HRV was found in normal subjects during Chinese Chi & Kundalini yoga meditation.5 In another study, meditation techniques characterized by slow breathing (<0.15Hz, less than 9 breaths per minute) resulted in very prominent and regular oscillations in the LF band on HRV.6 In these studies and others7 show the LF/HF ratio significantly shifted lower during meditation and was interpreted as indicating a relatively strong parasympathetic “mobilization.”
These reports guided us in a non-invasive evaluation of cardiovascular dynamics in subjects with the use of the Caretaker (www.caretakermedical.net) device during meditation in a diverse group of volunteers. The direct blood pressure measurements, power spectrum analysis of HRV, and blood pressure, were analyzed with the goal of exploring changes experienced between rest periods and meditation in the same subject. We were interested in distinguishing changes experienced by practitioners of a westernized form of Qi Gong, termed the reflective exercise technique (RE)8 from practitioners of other meditative exercises pooled together.
Subjects and meditation protocol. Thirty two volunteers were recruited who claimed knowledge and experience with meditation; the median age was 53 (range 21 to 70years) in 14 females and 17 males. Six subjects (2F and 4M) had a history of hypertension; three were taking antihypertensive medications. Two volunteers had used caffeine during the hour prior to meditation and one had participated in mild exercise in the preceding hour. No one smoked tobacco.
Twenty-six volunteers were “advanced” meditators who practiced >12months (range of meditation was at least one year to > 30years), 4 were intermediate (3 to 12months practice), one was a beginner (practicing meditation less than 3months); one did not admit to a meditation practice duration but claimed a long standing personal practice of unclassified meditation/mental relaxation. Of the 32 subjects, 14 subjects practiced RE while the other 18 subjects were recruited from either a weekly meeting forum that practiced mindfulness meditation or from members living at the Yogaville complex in central Virginia, performing various techniques such as mantra, prayer, integral yoga, and mindfulness meditation. All volunteers signed an informed consent reviewed and approved by Empirical Technologies, Inc, independent scientific review committee. The detailed demographic data and other relevant questions that could influence cardiovascular dynamics are shown in Table 1.
Age |
Gender |
HBP |
BP Meds |
BP |
Level |
Type of meditation practice |
Meditation frequency |
Breathing practice during meditation |
52 |
M |
no |
No |
127/73 |
advanced |
reflective exercise |
occasionally (every other day) |
reverse |
56 |
F |
yes |
No |
163/96 |
intermed |
mindfulness meditation |
every day (mixed) |
breath of peace |
54 |
M |
no |
No |
156/104 |
advanced |
reflective exercise |
occasionally (mixed) |
reverse |
54 |
M |
yes |
Yes |
138/88 |
intermed |
reflective exercise |
every day (mixed) |
reverse |
52 |
M |
yes |
No |
159/99 |
Intermed |
insight meditation |
occasionally |
“awareness of breath”, but not controlled breath) |
53 |
F |
yes |
Yes |
116/73 |
advanced |
mindfulness meditation |
occasionally |
no special |
62 |
M |
no |
No |
131/92 |
advanced |
reflective exercise |
occasionally |
reverse |
70 |
M |
no |
No |
137/82 |
advanced |
mindfulness meditation |
occasionally |
focused on breath |
56 |
M |
no |
No |
133/83 |
advanced |
reflective exercise |
every day |
reverse |
58 |
M |
no |
No |
116/80 |
intermed |
reflective exercise |
occasionally |
reverse |
33 |
M |
no |
No |
134/94 |
advanced |
reflective exercise |
rarely |
reverse |
21 |
M |
no |
No |
132/68 |
advanced |
reflective exercise |
occasionally |
reverse |
57 |
M |
yes |
Yes |
167/109 |
advanced |
reflective exercise |
every day |
reverse |
20 |
F |
no |
No |
117/74 |
advanced |
reflective exercise, without movement |
occasionally |
reverse |
22 |
M |
no |
No |
141/82 |
advanced |
reflective exercise without movement |
occasionally |
reverse |
22 |
M |
no |
No |
133/69 |
advanced |
reflective exercise |
occasionally |
reverse |
42 |
M |
no |
No |
145/74 |
n/a |
none (lowers pulse) |
n/a |
n/a |
22 |
F |
no |
No |
107/69 |
advanced |
reflective exercise |
every day (mixed, rarely RE) |
Dr. Weil’s “4-7-8” |
56 |
F |
no |
No |
119/78 |
advanced |
integral yoga |
every day |
Non-reverse |
64 |
F |
no |
No |
134/70 |
advanced |
Japa (with a mantra) |
every day |
Non-reverse |
49 |
F |
no |
No |
91/56 |
advanced |
“no name meditation” |
every day |
Non-reverse |
62 |
F |
no |
No |
107/64 |
advanced |
Non-reflective exercise |
every day |
Non-reverse |
67 |
M |
no |
No |
101/72 |
advanced |
Non-reflective exercise |
every day |
Non-reverse |
64 |
F |
no |
No |
145/73 |
advanced |
“sit” - no name meditation |
occasionally |
Non-reverse |
61 |
F |
no |
No |
106/64 |
advanced |
Jaba – mantra |
every day |
Non-reverse |
27 |
M |
no |
No |
98/56 |
beginner |
Non-reflective exercise |
every day |
Non-reverse |
28 |
F |
no |
No |
99/65 |
advanced |
Mantra meditatio |
every day |
Non-reverse |
40 |
M |
no |
No |
118/72 |
advanced |
blank |
every day |
Non-reverse |
63 |
F |
no |
No |
100/70 |
advanced |
Sitting+ mantra |
Occasionally |
Non-reverse |
24 |
F |
no |
No |
117/74 |
advanced |
reflective exercise |
Rarely |
Non-reverse |
66 |
M |
yes |
No |
168/115 |
advanced |
Prayer meditation |
every day |
no special |
29 |
M |
no |
No |
133/89 |
advanced |
Prayer meditation |
every day (mixed) |
no special |
Table 1 The detailed demographic data and other relevant questions that could influence cardiovascular dynamics
*p < 0.10 for comparison within groups at rest and during meditation
**p < 0.05 for comparison within groups at rest and during meditation
†p<0.10 for comparison between RE group and non-RE group
††p<0.10 for comparison between RE group and non-RE group
An important question asked of the participants was what type breathing they used. All subjects admitted to a breathing technique that we classified as 1. Reverse abdominal breathing, 2. “Non-reverse” if they did not understand the former term, or 3. a specific technique participants labeled themselves (Table 1). The importance given to breathing varies by practice, and can be considered active breathing where part of the technique concentrates on timing and depth (e.g., Zen Buddhist meditation, Yoga, Tai Chi), or passive or “natural” as in TM®, RR, CSM, Vipassana, and MBCT.2 For example, Yoga, which covers thousands of techniques, uses both active and passive breathing. Though the direction for active breathing may be relatively uniform across the techniques in a given practice (e.g., Zen Buddhist meditation), other practices use a wide array of breathing techniques that change according to the outcome desired (e.g., Kundalini yoga). For those practices that utilize passive breathing, there is no consistent pattern or rhythm as “breathing naturally” will vary by practitioner. Reverse abdominal breathing is also called “Taoist” breathing and is considered to have beneficial effects on the immune system.2 The technique calls for tightening of the abdominal muscles while inhaling and relaxing them with exhalation. This is a popular method in the eastern martial arts and is believed to increase guardian chi.8
RE’s version of reverse abdominal breathing is distinguished by 5 features: 1. the breathing is “light,” exclusively through the nostrils; 2. the breathing cycle is approximately 3 seconds for inhalation and 3 seconds for exhalation; 3. lower abdominal muscles gently contract in sync with inhalation and relax in sync with exhalation; 4. teeth of the upper and lower jaw lightly touch together, which causes the mastoid muscles of the jaw to flex mildly; 5. the tongue is lifted up to fill the upper palate with the tip resting behind the front teeth. These distinguishing features, along with other factors not taken into account, may have contributed to the cardiovascular dynamics that the study identified.
Non-invasive cardiovascular monitoring of subjects with the Caretaker device. The Caretaker device (CT) is an FDA approved external monitor that measures digital artery pressure with a low pressure sensing cuff attached to the base of the thumb (Figure 1).

Figure 1 The Caretaker device (CT) is an FDA approved external monitor that measures digital artery pressure with a low pressure sensing cuff attached to the base of the thumb.
The protocol used with these volunteers was to ask the subjects to sit quietly for several minutes while connected to the CT device. After about five minutes subjects were told to start their meditation practice using the breathing method that they were accustomed to while meditating. Meditation was performed for 10minutes and the subject was then instructed to stop. The Care Taker device records raw expression data at 500Hz. Using a smoother to eliminate false peaks, heart beats can be detected as peaks above a certain threshold. Subsequently, the series of inter beat intervals for a subject are taken to be the differences between times of these peaks and the instantaneous heart rates at each beat are calculated as the inverse of these interbeat intervals.9,10 For each heart beat, the systolic blood pressure and diastolic blood pressure are taken to be the differences in the pressure components of the raw expression data. The beat-to-beat time series of systolic and diastolic blood pressure and instantaneous heart rate, taken from a representative subject who practiced RE meditation, are displayed in Figure 2.
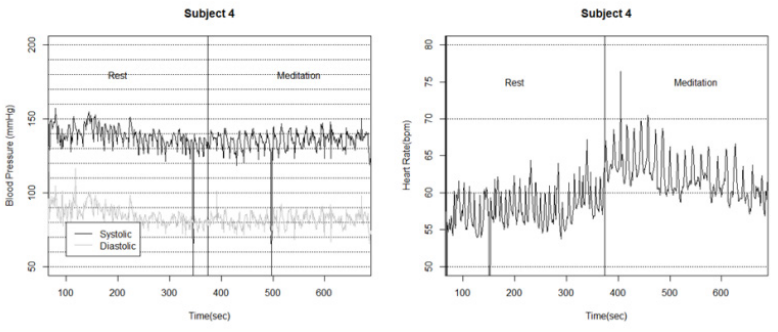
Figure 2 Caretaker output in a representative subject. The systolic and diastolic blood pressure readings calculated from the raw expression data are displayed in the left plot. In the right plot are the instantaneous heart beats. In both plots the rest and meditation periods are labeled. Notice that in both plots, large low-frequency oscillations begin with the initiation of meditation.
Signal processing and data analysis
Peaks in the signal are sometimes falsely identified as heart beats due to movement. Similarly a heart beat may be missed due to rapidly changing thresholds in the beat-detection algorithm. These occasional failures in the beat-detection can cause outliers in the time series and must be removed. Outliers in each heart rate series were identified visually and removed. To identify outliers in the systolic blood pressure series, a median smoother with a 30second window was used to calculate median smoothed series and the median absolute deviation (MAD) estimator, also with a 30second window, was used to estimate the standard deviation of each series about the median smoothed series. All observations outside 3times the standard deviation of the median smoothed series were identified as outliers and removed from the series.
Each time series spans both rest and meditation periods. These time periods were identified in each subject’s recordings so that estimates for both time periods could be analyzed. During the analysis it was noted that many records of the Yogaville data did not include the exact start and end time of meditation, possibly due to human or technical error. In these cases, the start and end times were established according to the protocol used consistently. In an effort to remove the potential bias introduced by unknown meditation start times in these subjects, 15 seconds at the beginning and end of each rest period and meditation period were removed. It is thought that this significantly reduces any bias introduced by estimated start and end times as well as any extraneous movement during the transition from rest to meditation. Two subjects did not have pre-meditation rest periods recorded, so estimates from their post-meditation rest period were used instead. The means and variances of each series were calculated and the Lomb-Scargle method for unevenly spaced observations was employed to estimate the Fourier spectral power of each time series. A low frequency power (0.04-0.15Hz) and a high frequency power (0.15-0.4Hz) were calculated as the area under the lomb periodogram within the respective frequency bands. Lomb periodograms for a subject who experienced significant increases in low frequency power in heart rate and systolic blood pressure are displayed in Figure 3.
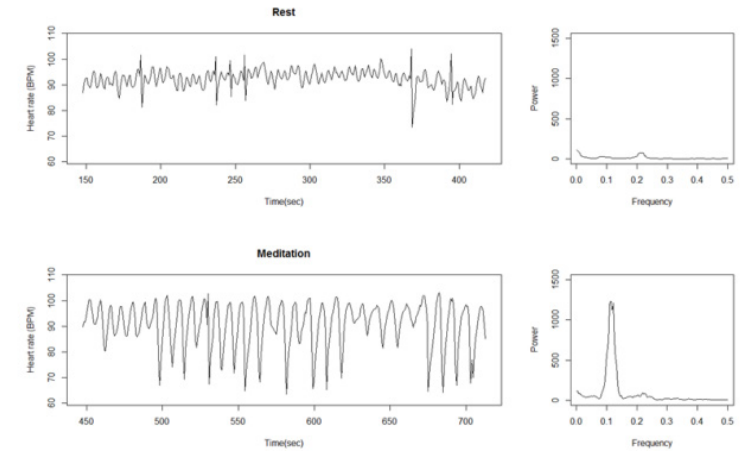
Figure 3 Effects of RE meditation on heart rate and systolic blood pressure on Subject 16. Figures in the left column show the raw time series. Figures on the right are the Lomb periodogram of each time series. The lomb periodograms are smoothed by a sliding mean with a window of 0.01 Hz. Increases in low frequency (0.04-0.15 Hz) power are visible between rest and meditation periods in both heart rate variability and systolic blood pressure variability.
Statistical analysis to test for differences between rest and meditation periods and between the RE group and the non-RE group, a nonparametric Wilcoxin two-sided test was used from the data of the values of low and high frequency HRV and Bp (data not shown).
Within the RE group, subjects experienced an increase in the low to high frequency ratio that is statistically significant at level 0.05 in both heart rate variability and systolic blood pressure variability. Subjects in the non-RE group, when pooled together for their general similarities, did not experience any significant changes during meditation from rest. These results are summarized in Tables 2 & 3. More specifically, 12 of the 14 subjects in the RE group experienced increases in the low frequency power of the heart rate, and all of them experienced increases in the low frequency power of the systolic blood pressure. This distinguishes the RE group from the general population of meditation practitioners represented by the non-RE group. This distinction is illustrated in Figure 4 in a log-scale of the data.
|
|
Heart rate |
Heart rate variance |
Normalized power |
Normalized power HF (0.18 – 0.4 Hz) |
LF:HF ratio |
Overall |
Rest |
69.86+/- 0.36 |
17.31+/- 3.84 |
4.20+/- 4.36 |
2.73+/- 2.90 |
3.24+/- 5.66 ** |
Group |
Meditation |
71.2 /- 10.78 |
27.12+/- 2.88 |
9.57+/- 14.52 |
2.76+/- 3.59 |
7.78+/- 11.51 ** |
RE Group |
Rest |
67.76+/- 1.75 |
19.49+/- 4.85 |
4.31+/- 4.46 * |
3.62+/- 3.62 |
1.58+/- 1.15 ** |
Meditation |
70.33+/- 2.62 |
40.30+/-2.69 † |
15.62+/- 19.14 *†† |
4.18+/- 4.45 |
7.20+/- 9.62 ** |
|
non-RE Group |
Rest |
71.69+/-8.95 |
15.41+/- 3.07 |
4.10+/- 4.42 |
1.95+/- 1.87 |
4.70+/- 7.48 |
Meditation |
71.90+/-9.23 |
15.59+/-4.40 † |
4.27+/- 5.09 †† |
1.53+/- 2.08 |
8.29+/- 13.24 |
*p < 0.10 for comparison within groups at rest and during meditation
**p < 0.05 for comparison within groups at rest and during meditation
†p<0.10 for comparison between RE group and non-RE group
†† p<0.10 for comparison between RE group and non-RE group
|
|
Systolic |
Systolic variance |
Normalized power |
Normalized power HF (0.18 – 0.4 Hz) |
LF:HF ratio |
Overall |
Rest |
122.35+/- .08 |
88.13+/- 75.79 |
10.85+/- 10.15 |
15.79+/- 17.57 |
0.97+/- 0.88 ** |
Group |
Meditation |
121.09+/-1.59 |
75.20+/- 51.46 |
14.68+/- 12.40 |
12.37+/- 14.51 |
2.30+/- 2.16 ** |
RE Group |
Rest |
128.10+/-3.83 |
71.03+/- 48.75 |
6.59+/- 3.63 ** |
9.44+/- 6.17 |
0.81+/- 0.54 ** |
Meditation |
127.24+/-0.47 |
69.61+/- 50.84 |
15.55+/- 12.06 ** |
9.69+/- 14.35 |
2.58+/- 1.99 ** |
|
non-RE Group |
Rest |
117.31+/-9.57 |
103.09+/- 2.38 |
14.58+/- 12.50 |
21.34+/- 22.21 |
1.11+/- 1.10 |
Meditation |
115.71+/-8.72 |
80.09+/- 53.15 |
13.91+/- 13.03 |
14.73+/- 14.71 |
2.05+/- 2.33 |
*p < 0.10 for comparison within groups at rest and during meditation
**p < 0.05 for comparison within groups at rest and during meditation
†p<0.10 for comparison between RE group and non-RE group
†† p<0.10 for comparison between RE group and non-RE group
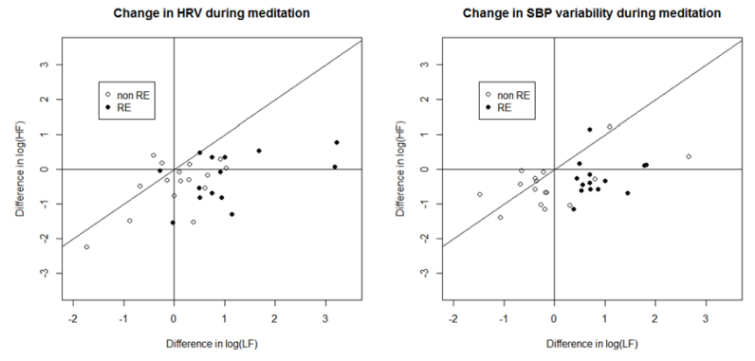
Figure 4 RE subjects generally experienced increases in the LF/HF ratio in heart rate variability. This can be seen in the plot above in which most RE data appear below the diagonal line.
To formally test the differences in effect between the RE group and the non-RE group, the estimates taken during rest periods are subtracted from the estimates taken during the meditation periods. The RE group experienced greater increases in median heart rate, low frequency heart rate variability and low frequency to high frequency ratio in the heart rate power spectrum all at significance level 0.05. The RE group also experienced a significantly greater increase in low frequency systolic blood pressure variability and low to high frequency ratio in systolic blood pressure variability. These results can be seen in Tables 4 & 5 with the power spectrum results scaled with the natural log Table 4.
Heart rate |
Mean |
log variance |
log normalized power LF (0.04 – 0.15 Hz) |
log normalized power HF (0.18 – 0.4 Hz) |
log LF/HF |
RE Group |
2.57+/- 4.80† |
0.53+/- 0.57†† |
1.05+/- 1.03†† |
-0.23+/- 0.72 |
1.29+/- 0.94†† |
non-RE Group |
0.21+/- 1.84† |
-0.01+/- 0.42†† |
0.02+/- 0.71†† |
-0.45+/- 0.74 |
0.46+/- 0.65† |
Table 4 Changes in subject between rest period and meditation period
†p<0.10 for comparison between RE group and non-RE group
††p<0.10 for comparison between RE group and non-RE group
Systolic blood pressure |
Mean |
log variance |
log normalized power LF (0.04 – 0.15 Hz) |
log normalized power HF (0.18 – 0.4 Hz) |
log LF/HF |
RE Group |
-0.86+/- 6.17 |
-0.04+/- 0.54 |
0.87+/-0.52 †† |
-0.27+/- 0.58 |
1.13+/- 0.65 †† |
non-RE Group |
-1.60+/- 5.56 |
-0.11+/- 0.60 |
-0.09+/- 1.01 †† |
-0.41+/- 0.65 |
0.32+/- 0.78 †† |
Table 5 Changes in subject between rest period and meditation period
†p<0.10 for comparison between RE group and non-RE group
††p<0.10 for comparison between RE group and non-RE group
In the practice of meditation there is general agreement about the central role of the inward mental control of attention. The practice is coupled with an awareness of the respiration cycle but the breathing techniques and breathing rate may differ and are not commonly a uniform element involved with the central teaching of meditation practices. Indeed, the criteria for successful meditation have not been well described in the literature as sited by the review of over eight hundred publications on the subject.2 Here we studied meditation practices that differed in their approach to breathing either based on the reverse abdominal breathing technique, a key part of RE, or those with non-specific breathing practices during meditation.
In reports where HRV measurements coupled with breathing rate5 or simultaneously measured with blood pressure during meditation practice,6 an unusual observation shows that meditation techniques like the “relaxation response” and “segmented breathing” can induce prominent elevated heart rate and blood pressure fluctuations. These particular findings have been labeled “paradoxical” given the notion that meditation asks the practitioner to concentrate on mental stillness thought to result in quiescent cardiac dynamics. Our data indicate the same as shown in Figure 2 where there is evidence of elevated activity during meditation. Meditation thus appears to be associated with non-blunted cardiovascular rhythmicity and is associated with sympathetic/vagal balance. The benefits of meditation appear to correct chronic patho-physiologic imbalance, possibly directly through normalization of cardiovascular mechanisms.
One gauge of the salubrious effect of meditation is through the evaluation of the spectral analysis of HRV that we performed. First, several reports have shown the utility of HRV is the assessment of short and long term outcomes that reflect physiologic, pharmacologic, and pathologic conditions.8‒10 We and others have identified that meditation increases LF and that this has been interpreted as reflecting an increase in the balance of the autonomic nervous system.5,11
We also describe that there may be a difference in the production of the LF dimension of HRV with the type of meditation, and the associated breathing practice, by showing that the subjects practicing RE had a wider swing compared to non-RE practitioners. One possible explanation for this difference is RE’s distinct approach to reverse abdominal breathing. On the other hand, the absence of an LF increase for the non-RE practitioners could stem from factors associated with living in a community like a Yogaville where the baseline level of LF was higher than those living in a more conventional setting. This is hypothesis generating and presents another dimension of meditation research that suggests there may be a need to account for the social context of the subjects being studied.
Another dimension of our pilot study is the recognition of the utility of using a non-invasive cardiovascular device like the CareTaker. We found it to be quite feasible to make these measurements and were impressed with the lack of disturbance caused by such a small and unobtrusive device that we are confident provided us with useful data without artifact.
None.
Author declares there are no conflicts of interest.
None.

©2016 Rich, et al. This is an open access article distributed under the terms of the, which permits unrestricted use, distribution, and build upon your work non-commercially.