eISSN: 2373-6372


Case Report Volume 10 Issue 3
Hospital Universitario de Puerto Real, Spain
Correspondence: German Santamaria Rodriguez, Hospital Universitario de Puerto real (CADIZ), Spain
Received: August 05, 2019 | Published: May 29, 2019
Citation: Rodríguez GS, Prado AM. Ulcerative colitis and lymphoproliferative disorder. Gastroenterol Hepatol Open Access. 2019;10(3):132-136. DOI: 10.15406/ghoa.2019.10.00371
The lymphoma of the primary gastrointestinal tract (LGIP) is a rare form of presentation of gastrointestinal tract lymphomas. Inflammatory bowel disease and its base treatment are known risk factors for its appearance. We report a 56-year-old female patient with Ulcerative Colitis of eight years of evolution, treated only with mesalazine due to azathioprine intolerance. After a recent weight loss and abrupt change in the intestinal habit, a new coloncoscopy was performed showing a rectal ulcerative lesion with a depressed center, corresponding to a follicular non-Hodkin B lymphoma. The patient was treated with RCHOP chemotherapy (Rituximab cyclophosphamide doxorubicin vincristine prednisone) initially successful but pending re-evaluation after 4 cycles for finally disease remission.
Keywords: colitis, ulcerative, inflammatory bowel disease, lymphoma, large b-cell, diffuse
Ulcerative colitis, as well as intestinal inflammatory diseases in general is associated with a higher incidence of neoplasms, both due to the chronic inflammatory process and to many of the drugs used. Emphasize colon adenocarcinoma, cholangiocarcinoma (associated with PBC), lymphomas or skin cancer.
The lymphoma of the primary gastrointestinal tract (LGIP) describes the lymphoma that originates in the gastrointestinal tract, representing only 5-10% of all lymphomas1–3 and up to 20% of extranodal lymphomas 4,5.
This type of lymphoma, however, is infrequent, constituting only 1-4% of gastrointestinal neoplasms5. Studies have suggested that the incidence of LGIP has increased,4,7 a trend that could be explained by the presence of immunosuppression states, whether mediated by an acquired immunodeficiency syndrome (AIDS), by drugs in the context of a post-transplant or associated with diseases autoimmune diseases such as rheumatoid arthritis, systemic lupus erythematosus or celiac disease.4,8,9
Among the drugs that favor the development of lymphoma, thiopurine (azathioprine and 6-mercaptopurine)11,11 and, to a lesser extent, anti-TNF biological therapy.11
Although LGIP can compromise any region of the gastrointestinal tract, the most affected areas are the stomach, followed by the small intestine and the ileocecal region.11 Although the colorectal region can be compromised in up to 20% of LGIP4,11,11 primary colorectal lymphoma is very rare, constituting <1% of neoplasms at this level.11
Similarly to what occurs in other areas of the gastrointestinal tract, primary colorectal lymphoma is mainly a non-Hodgkin B-cell lymphoma, with diffuse large B-cell lymphoma being the most frequent. It can also present as a follicular lymphoma, lymphoma associated with lymphoid tissue of the mucosa, lymphoma of mantle cells and lymphocytic small cell.11,11
We present the case of a 56year-old woman, No allergic medication reactions, smoker of 10cig/day, an abortion (negative for Antiphospholipid syndrome) and with ischemic cerebrovascular stroke in 2010 without aftermath. Ulcerative pancolitis of 8years of evolution, in treatment with 5´ ASA (Mesalazine), with last complete colonoscopy previous year, showing ulcerative proctosigmoiditis with moderate activity and the rest of the surrounding quiescent mucosae.
She consulted for intestinal tract disorder consisting of 2-3 daily stools alternating with constipation in the last month, loss of about 7kg of weight at that time and general malaise with abdominal discomfort.
The examination revealed a palpable mass of about 4m in the right lower quadrant, not displaceable, painless that the patient had gone unnoticed and apparently not adhered to deep planes.
Lab test only Ca 125 of 359 U/ml stood out
Ultrasonography: an inflammatory mass-plastron in the right iliac fossa was found in the theoretical ileocecal area of about 4x5cm maximum diameter, as well as bilateral pleural effusion, minimal perihepatic and perisplenic free ascites and retroperitoneal adenopathies. Also compression of both ureters with bilateral hydronephrosis
Abdominal CT: a large retroperitoneal mass is observed that involves vascular structures with thickening and hypercaptation of rectum, cecum and terminal ileum walls, as well as multiple inguinal adenopathies, the largest in the left iliac fossa of 26mm.
Before an unexpected polyadenopathic picture with associated polyserositis, the etiological approach was initiated: Thoracentesis was initially performed with extraction of pleural fluid compatible with transudate, normal ADA.
Negative Mantoux
We consulted with the Surgery team and exeresis of the larger inguinal lymphadenopathy was carried out for anatomopathological study.
Subsequently, a colonoscopy was performed where, at the first Houston valve, an ulcerated lesion with a depressed center was identified, which appeared to extend around 1/3 of the circumference of the rectum, from which multiple biopsies were also taken. With the presumptive diagnosis of eventual disseminated rectal cancer in a patient with the known inflammatory disease, both samples were submitted for A.P study.
Also a TPE was taken out glandular involvement supra and, to a greater extent, infradiafrgamatics, highlighting an increase in retroperitoneal hyper metabolic density; as well as intestinal infiltration and right parotid doubtful. Probable splenic and medullary bone hyperreactivity with dubious right iliac focus. Moderate amount of normometabolic ascitic fluid.
Proposed Ann-Arbor Stadium IV (Figures 1-10)
Finally, after histopathological and immunohistochemical study, the diagnosis of follicular non-Hodkin B lymphoma, histological grade 2, was confirmed in both anatomopathological samples.
It was referred to Hematology for treatment with the diagnosis of Non-Hodgkin B Follicular Lymphoma Grade 2 Bulky abdominal. Stage IIIB. FLIPI 2, taking a therapeutic regimen with CHOP (Rituximab + Cyclophosphamide + Adriamycin + Vincristine and prednisone) with re-evaluation after 4 cycles.
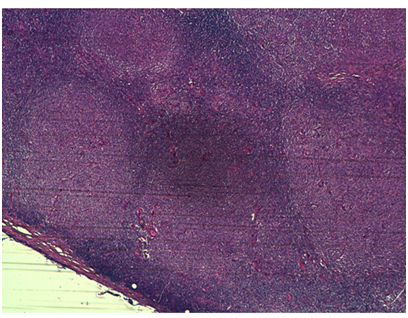
Figure 4 Follicular pattern in inguinal adenopathy. Tumor composed of atypical large lymphoid cells with pleomorphic nuclei and prominent nucleolus
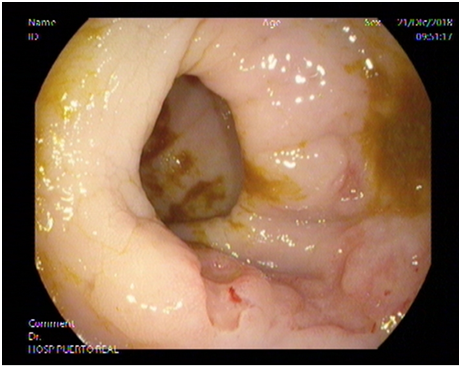
Figure 6 Diffuse non-Hodgkin lymphoma of large B cells of rectum in a patient with a history of ulcerative colitis on colonoscopic examination. (Pre-chemotherapy injury).
The risk of lymphoma in patients with IBD is mainly associated with the use of immunosuppressive drugs (such as thiopurines or anti-TNF.) In our case, the rapid evolution (Colonoscopy a year ago with minimal aphthae in the rectum and sigma, not very compatible with the Inflammatory well-known with little activity) and being only in treatment with mesalazine at sub-therapeutic doses (1.2gr) and with some cycle of isolated steroids, not being associated to any of the expected drugs.
Given the form of presentation, the differential diagnosis was a challenge due to the unusual way of debut and finally after imaging tests and histopathological and immunohistochemical techniques, the referred diagnosis was reached, finding the patient stable at the present time and in remission.
Primary rectal lymphoma is infrequent, constituting only 0.05% of all primary neoplasms of the rectum.11 Its frequency is less than primary lymphoma of ascending colon and cecum, given the greater amount of lymphoid tissue in that area compared to the rest of the colon and rectum.7 The clinical, iconographic and endoscopic presentation are nonspecific and subtle, so diagnosis is difficult, being most of the time indistinguishable from other colon diseases, either neoplastic or inflammatory as it occur in our case.
When lymphoma is located in the rectum, the main clinical features are rectal bleeding, proctalgia, tenesmus, and changes in the intestinal habit (diarrhea or constipation).11 In some cases, the diagnosis is made incidentally, as it was presented in our patient.11
Although the majority of primary colorectal lymphomas are non-Hodgkin B-cell lymphomas, studies in China and Korea have shown a higher percentage of T-cell lymphoma, which would have a worse prognosis.22,22 PET/CT are techniques of choice for the staging and extension of the evaluation of the presence of a given mass, area of stenosis and ganglionic involvement.22 Colonoscopy may show a variable involvement of the mucosa, whether it is a mass, an ulceration or infiltration22 and allows obtaining biopsies for a pathological diagnosis.
At present time the risk of lymphoma has become a relevant variable to take into consideration when setting the therapeutic strategy in patients with IBD. Persistent chronic inflammation may play a role in the promotion of carcinogenesis and the development of lymphoma precursor cells, which would lead to overstimulation and continuous proliferation of the immune system.22 However, unlike what happens with rheumatoid arthritis15, the incidence of LGIP in patients with IBD is relatively low, indicating that IBD alone would not be a definitive independent risk factor in the development of lymphoma.22
Infection by EBV is another known risk factor associated with the appearance of a lymphoma; Dayshard et al. showed that those patients with IBD treated with thiopurine who later developed a lymphoma had more frequent EBV in the tumor cells,22 which we could not demonstrate in our patient after examining minutely the biopsy samples.
Finally, the use of thiopurinics and anti-TNF has also been associated with the risk of lymphoma, although evidence is scarce. In the case of thiopurinics, studies are contradictory, probably due to bias in the population studied and the duration of therapy.11,11,22,22 Studies have suggested a 4-year threshold for thiopurine therapy as a risk factor for developing a lymphoma,22,22 a situation that did not occur in our patient. The risk of lymphoma associated with the use of anti-TNF in patients with IBD is difficult to quantify, since most patients have treatment associated with thiopurine or methotrexate concomitantly33 Recently, a large population of a multicenter study of over 11,011 patients followed up for a median of 98 months showed that neither immunosuppressants nor anti-TNF drugs therapy seem to increase the risk of developing a lymphoma or other extracolonic cancer.33
In summary, managing colorectal lymphoma requires a multidisciplinary evaluation, where prognosis and survival of the patient is determined by the stage of the lymphoma at the moment of diagnosis. Regarding treatment alternatives, there is no consensus on the best therapeutic strategy, with the options being: surgery, chemotherapy and radiotherapy, either as a single or combined treatment.11,33–33 In our patient, chemotherapy with an R-CHOP scheme was chosen, achieving criteria of complete remission after 6 cycles, without complications . In relation to the effect of chemotherapy on the evolution of IBD, different studies have shown its beneficial effect.33,33 The evolution of our patient has been favorable, being evaluated three months after the end of his chemotherapy, being presently in clinical remission (clinical May index 0) and endoscopic (Mayo endoscopic index 1 at the level of rectum and sigmoid.
In conclusion, although LGIP is infrequent entity, it should be considered in patients with IBD who do not show a favorable or torpid evolution. The involvement of IBD and the immunological bases that promote lymphocyte activation, together with the role played by thiopurine and anti-TNF treatments in the appearance of lymphoma remains controversial and must be elucidated.
None.
Author declares there are no conflicts of interest.

©2019 Rodríguez, et al. This is an open access article distributed under the terms of the, which permits unrestricted use, distribution, and build upon your work non-commercially.