eISSN: 2373-6372


Research Article Volume 11 Issue 2
1Department of Internal Medicine and Gastroenterology, Cairo University, Egypt
2Department of Internal Medicine, Cairo University, Egypt
3Department of Medicine, Mid Columbia Hospital, USA
4Department of Gastroenterology, Johns Hopkins University Hospitals, USA
Correspondence: Abeer Awad Abdellatif, Lecturer of Internal Medicine, MD, Kasr Al-Aini Hospitals, Cairo University, Cairo, Egypt, Tel 01002776494
Received: February 20, 2020 | Published: April 21, 2020
Citation: Okasha HH, Abdelfattah Y, Ashoush OA, et al. Role of ultrasound and ultrasound guided fine needle aspirationin diagnosis of peritoneal diseases. Gastroenterol Hepatol Open Access. 2020;11(2):84-87. DOI: 10.15406/ghoa.2020.11.00419
Introduction: Peritoneal diseases have different types of presentations which can be detected by endosonography. The aim of our study is to assess the performance of ultrasound (US) and US-guided FNA in diagnosis of different peritoneal diseases.
Material & methods: we collected the data from 53 Egyptian patients with suspected peritoneal lesions and localized ascites. The detailed sonographic features were assessed for any peritoneal masses, deposits, omental heterogeneity and thickness, and for the detection of any fluid collections. The final diagnosis was reached by the positive cytopathological examination of aspirate taken by FNA. The patients who lost follow up, with severe coagulopathy or whose final diagnosis was not reached were ruled out from the study.
Result: ultrasound showed high sensitivity (97.9%) with 95.9% PPV, 75% NPV and 94.34% accuracy while US-FNA shows high specificity (100%) with 100% PPV, 45.45% NPV and 88.68% accuracy rate in diagnosis of different peritoneal diseases.
Conclusion: Ultrasound and FNA are very valuable in detection and diagnosis of different peritoneal benign and malignant diseases. In spite of statistically significant increase in sensitivity of US diagnosis of different peritoneal diseases more than that diagnosed by FNAC, yet, US FNA is crucial for confirming the diagnosis for determination of the plan of management of different peritoneal lesions.
Keywords: ultrasound, FNA, diagnosis, peritoneal diseases
US, Ultrasound; FNA, Fine needle aspiration; APD, antro-posterior diameter; AUC, area under the curve; PPV, positive predictive value; NPV, negative predictive value; ROC, receiver operating characteristic
The peritoneum is a sheet of serous membrane that has a large surface area equal to the surface area of the skin, approximately 2m2, in adults. It lines the abdominal cavity and surrounds the multiple abdominal organs.1 The peritoneum and peritoneal cavity are commonly involved in many primary and secondary diseases such as primary malignancy (mesothelioma), infectious disease (tuberculosis), and disseminated malignancy (peritoneal carcinomatosis). The peritoneal diseases have different types of presentations such as ascites and/or peritoneal masses, deposits or nodules.2 Ultrasound (US) is an accurate, safe, inexpensive, and readily accessible imaging tool for investigation of many peritoneal diseases which can detect many primary or secondary peritoneal diseases especially if done by well trained sonographer who must be aware of the potential involvement of the peritoneum and peritoneal cavity with many specific diseases.3
Asis a wide variety of clinical and sonographic characteristics of the primary diseases of the peritoneum, so the awareness of the key imaging, pathophysiologic, and demographic characteristics of primary involvement of the peritoneum is very important for the sonographer to identify these lesions appropriately and reaching the final diagnosis. However, there is a limitation in identifying the early peritoneal lesions which measure less than 0.5 cm and in identifying the diffuse peritoneal disease that the sonographer must be aware of Patrick DM.4 Thickening and/or enhancement of peritoneal reflections, plaques/sheets of soft-tissue that form small or large masses, lymphadenopathy, thickening and distortion of the mesentery, thickening, nodularity and serosal deposits of bowel wall are some of common ultrasonographic findings that can be detected in different peritoneal diseases.5,6
FNAC under image guidance (US or CT) is considered a revolution in the field of cytopathological diagnosis. It is characterized by having a high degree of accuracy, being a minimally invasive procedure to the patient and allowing reaching the probable diagnosis before surgery without subjecting the patient to much more invasive procedure. However, it does not always differentiate between benign and malignant lesions.7–9 The aim of our study is to assess the performance of US and U/S-guided FNA in the diagnosis of peritoneal diseases.
Study design and population
This prospective study analysed data from 53 Egyptian patients who were referred to the GIT Unit in the Internal Medicine Department of the Faculty of Medicine of Cairo University during period from February 2016 to march 2018. The included patients were referred for US and US FNA for diagnosis of peritoneal diseases.
Inclusion criteria
All patients older than 18 years were referred for US and US-FNA for conditions involving the peritoneum and peritoneal cavity that were suspected clinically or with other imaging modalities. The study protocol was revised and approved by the Medical Research Committee in the Internal Medicine Department at Faculty of Medicine Cairo University. Informed consent from each participant was obtained after good explanation about the study objectives& procedures. All procedures for data collection were treated with confidentiality according to Helsinki declarations of biomedical ethics.
Exclusion criteria
Methodology
For all patients, US and US FNA were performed at the request of the consultant physician. For confidentiality, the patient names were omitted and replaced with numerical codes. On the day of the procedure, the patients were subjected to a thorough history and clinical examination. All patient data were recorded. U/S was performed using a Hitachi EUB-7000 US unit (Hitachi Medical Systems, Tokyo, Japan).
For patients who underwent US FNA, prothrombin time was checked before the procedure, the site of puncture was marked on skin and the area was cleaned with antiseptic solution. Local anaesthesia was given with xylocaine injection. Needle inserted (Chiba needles) under complete imaging guidance technique with biopsy attachment. The needle size used ranging from 18 to 22 G attached to 10ml syringedirected to one of three passes according to the accessibility of the lesion. The aspirate was spread over glass slides, air dried and fixed in 95% alcohol and was sent for cytopathological examination. The percent of cases were done by 1st pass were28.3% while 67.9%, 3.8% for 2nd and 3rd passes respectively. For all patients, the detailed sonographic features were assessed, including thickness [antro-posterior diameter (APD)], echotexture (echogenic, echo-poor or heterogenous), the presence of any peritoneal masses or deposits, and the presence or absence of any fluid collections.
The final diagnosis was reached by the positive cytopathological examination of aspirate taken by FNA. Patients with benign aspirate were followed for at least one year with stationary or regressive course of the disease. All US and US-FNA were done by a single gastroenterologist. In our study there were no major complications a part from mild pain and discomfort at the puncture site for short duration needing no hospital admission.
Compliance with the study
All patients were compliant with the study.
Statistical analysis
All patient data were documented using Excel 2010. Data were processed using SPSS version 20 for Windows 2010as follows: Description of quantitative variables as mean, SD and range. Description of qualitative variables was done as number and percentage. All qualitative data were analysed using the chi-square test or the Fischer’s exact test, as appropriate. The chi-square test was used to calculate Pearson’s chi-square and its P value when both table variables were quantitative. The sensitivity, specificity, accuracy, positive predictive value (PPV) and negative predictive value (NPV) were calculated. Receiver operating characteristic (ROC) curves were applied to calculate the area under the curve (AUC) and the sensitivity and specificity of the tests used. Cut-off values were calculated. And in this context the differences for which P>0.05 were not considered to be significant, differences for which P<0.05 were considered to be statistically significant and differences for which P<0.001 were considered to be highly significant.
The total number of patients involved in the study were 53 including 23 (43.4%) males and 30 (56.6%) females with age ranging from 25 to 70years with a mean (SD) of 47.2 (9.56) years. The percent of benign and malignant diseases diagnosed by US was 7.5% and 92.5% respectively, while that diagnosed by FNA was 20.8% and 79.2% respectively. The final diagnosis was 9.4% benign lesions and 90.6% malignant lesions. Although the meanantro-posterior diameter of the omentum of the patients with benign lesions was smaller than that of malignant lesions (14.3±6.2mm versus 24.32±13.9mm) this difference did not reach statistical significant, probably due to the smaller number of patients with benign peritoneal diseases. The final diagnosis of our 53 patients was 38 cases of peritoneal deposits (34adenocarcinoma, 1 peritoneal deposit with liver metastases, 1 neuroendocrine tumour, 1 papillary serous adenocarcinoma, 1 signet ring carcinoma), 2 cases of lymphoma, 4 cases of pseudomyxoma, 4 cases of mesothelioma, and 5 cases of TB (Table 1).
Final Diagnosis |
Number |
% |
Deposits |
38 |
45.3 |
Deposits (adenocarcinoma) |
35 |
|
Deposits (neuroendocrine tumor) |
1 |
|
Papillary serous adenocarcinoma |
1 |
|
Deposits (Signet cell carcinoma) |
1 |
|
Deposits with liver metastases (Figure 1) |
1 |
|
Lymphoma |
2 |
3.8 |
Pseudomyxoma |
4 |
7.5 |
Mesothelioma (Figure 2) |
4 |
7.5 |
TB |
5 |
9.4 |
Total |
53 |
100 |
Table 1 Final diagnosis of the patients
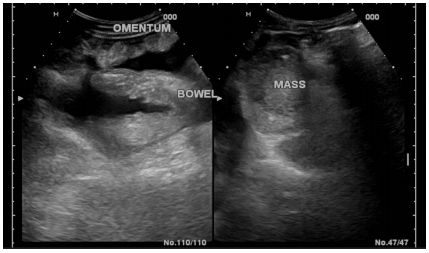
Figure 2 A patients with mesothelioma showing thickened omentum with heterogeneous texture and ascites.
Results depicted in Table 2 demonstrate performanceof US and US-FNA in detecting the final diagnosis in different peritoneal diseases. It revealed 97.9% sensitivity, 60 % specificity for US diagnosis with 95.9% PPV and 75% NPV compared to 87.5% sensitivity, 100% specificity for US-FNA diagnosis with 100% PPV and 45.45% NPV as demonstrated in Table 2. The accuracy rate for US diagnosis was 94.34% in comparison to 88.68% for US-FNA.
|
Sensitivity |
Specificity |
PPV |
NPV |
Accuracy |
US |
97.9% |
60% |
95.9% |
75% |
94.34% |
US-FNA |
87.5% |
100% |
100% |
45.45% |
88.68% |
Table 2 Sensitivity & specificity of US and US-FNA in detecting the final diagnosis
The current study evaluated the value of both US compared with US-FNAC in peritoneal disease diagnosis. The peritoneum and peritoneal cavity are commonly involved in many primary and secondary diseases such as primary malignancy (mesothelioma), infectious disease (tuberculosis), and disseminated malignancy.8 In the present study, the number of patients involved were 53 including (23, 43.4% males) and (30, 56.6% females) with male predominance and age ranging from 25 to 70years. This is comparable with Mangal et al.10 study10 who studied 85 cases [(57, 67%) males and (28, 33%) females] of retroperitoneal lesions using US- guided FNA, their age ranges from five to 82years.10
In the present study, no major complications were found apart from mild pain at the site of needle puncture that lasted for few minutes. Similarly Singh et al reported minor complications in their study and no major complications as pancreatitis, hemorrhage or pneumothorax were recorded.8 Percutaneous fine needle aspiration is a safe, cost effective accurate and minimally invasive procedure essential in the diagnosis of intra-abdominal lesions as peritoneal masses with no need for laparotomy.8 US-guided percutaneous FNA of abdominal masses was first reported by Kristensen et al.11 whostated that FNA guided by ultrasound is important for preoperative diagnosis if there is a cystic degeneration in a solid lesion or if there are any malignant features.10
Similar to other previous studies,11,12 the present study showed that malignant lesions were much more common than benign lesions, the percent of benign and malignant diseases diagnosed by US equal 7.5% and 92.5% respectively, compared with those diagnosed by FNA which were equal 20.8%, 79.2% for benign and malignant lesions respectively. Evaluation of the sensitivity & specificity of US and US-FNA in detecting the final diagnosis in different peritoneal diseases in our results showed 97.9% sensitivity, 60% specificity for U/S diagnosis with 95.9% PPV and 75% NPV compared to 87.5% sensitivity, 100% specificity for US-FNA diagnosis with 100% PPV and 45.45% NPV, so the accuracy rate for US diagnosis was 94.34% in comparison to 88.68% for U/S-FNA. It is encouraging to compare these results with Ahn's et al study which concluded that sonography may provide reliable support in a wide range of masses and peritoneal lesions in the abdomen.13 AlsoStepanov et al concluded that ultrasound examination of the peritoneal masses is an effective method for diagnosing and adequate staging in cases of late-stage tumours.14 More over according to Levi et al study 2009 US can be a very accurate, safe, cheap, and accessible imaging way for investigation of many peritoneal diseases.15
However, these results differ from some published studies, for example, Wang et aldid a retrospective analysis on 153 consecutive patients with ascites and/or abdominal distension with no specific cause. All of the patients showed abnormalities of the peritoneum or greater omentum after ultrasonography, ultrasound-guided percutaneous biopsy is used for final diagnosis of these peritoneal lesions.16 A specific histopathological diagnosis was made in 142 out of 153 patients, with an overall diagnostic accuracy of 92.8%. They concluded that ultrasonography can allow easy visibility of any abnormality in the peritoneum, however it is not so easy to diagnose peritoneal lesions using ultrasound only because of difficult listing a differential diagnosis from other abdominal organs like the intestines. In spite of the difference between the ultrasonographic images of benign and malignant lesions are quite clear, their images may overlap, which makes the lesions hard to differentiate. For this reason, a biopsy is needed.16
To conclude, in spite of statistically significant increase in sensitivity of US diagnosis of different peritoneal diseases more than that diagnosed by FNAC, yet, ultrasound-guided percutaneous biopsy is crucial confirm the specific peritoneal pathology to determine further plan of management.
None.
Author declares that there are no conflicts of interest.
The authors declared that this study has received no financial support.

©2020 Okasha, et al. This is an open access article distributed under the terms of the, which permits unrestricted use, distribution, and build upon your work non-commercially.