eISSN: 2373-6372


Mini Review Volume 10 Issue 2
1Department of Internal medicine. Military Hospital of Gabes, Tunisia
2Sfax Faculty of Medicine, University of Sfax, Tunisia
3Department of Radiology. Hedi Chaker Hospital of Sfax, Tunisia
Correspondence: Dr Salem Bouomrani, MD, PhD, Department of Internal medicine, Military Hospital of Gabes. Gabes 6000, Tunisia, Tel +00216 98977555
Received: January 28, 2019 | Published: April 3, 2019
Citation: Bouomrani S, Feki W. Pancreatic and gastrointestinal hydatidosis. Gastroenterol Hepatol Open Access. 2019;10(2):108?110. DOI: 10.15406/ghoa.2019.10.00366
Hydatidosis is a cosmopolitan parasitosis that is still endemic in several countries. The main locations of this disease are the liver and lungs accounting for more than 90% of cases. Other rare localizations can be seen in less than 10% of cases and are said to be unusual or "ectopic": splenic, renal, bone, neurological, cardiac, soft tissue... The pancreatic and gastrointestinal localizations of humain echinococcosis remain exceptional and unusual even in the endemic areas of this parasitosis, often representing real diagnostic and therapeutic challenges. Through this review we discuss the main epidemiological and clinical features of pancreatic and gastrointestinal localizations of human hydatid disease.
Keywords: hydatid cyst, hydatidosis, echinococcosis, pancreas, gastrointestinal tract
The pancreatic localization of the hydatid cyst (HC) is exceptional and unusual;1,2 in fact, only one case was found in the Tunisian series of Bellil S et al of 256 cases of extra-pulmonary operated HC (0.4%),3 whereas no case was noted in the series of 42 cases of intra-abdominal operated HC of Abebe E et al.4 and no case was noted in the Lianos GD et al.5 series of 233 patients treated for hydatid cyst over a period of 33 years, of which 18 presented unusual locations.5 Its overall frequency is estimated by series and recruitment services at 0.2-2%,1,2,6,7 and is often very difficult to diagnose preoperatively.2,8
This localization is most often secondary or part of a diffuse hydatidosis;7,9 primitive forms of pancreatic HC are much rarer.6–8 All portions of the pancreas (body, head and tail) may be the site of this parasitosis;1,6–9 similarly, an anecdotal case of primary HC of the main pancreatic duct has been reported.10
The pancreatic HC may remain asymptomatic for a long time. The symptomatic forms are classically presented by vague and atypical abdominal pains1,6,8,9 or by an abdominal mass, most often epigastric.6,8 More rarely, jaundice, hepatomegaly or deterioration of the general state with significant weight loss8 can be noted. Complicated forms may exceptionally occur as an acute surgical abdomen.2,7,11 Possible complications of pancreatic echinococcosis are: intracystic suppuration,2 fistulization and rupture in neighboring organs or abdominal cavity,6,9 and exceptionally pancreatic necrosis (a case of acute necrotic pancreatitis of hydatid origin was reported) (Figure 1-3).7
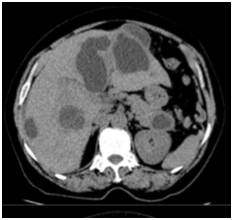
Figure 1Axial abdominal CT-scan without injection of contrast product: hydatid cyst of the tail of the pancreas, with associated multiple hydatid cysts of the liver.
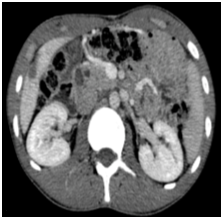
Figure 1Axial abdominal CT-scan with injection of contrast product: primitive and isolated hydatid cyst of the head of the pancreas.
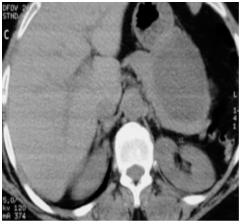
Figure 3Axial abdominal CT-scan with injection of contrast product: giant hydatid cyst of the tail of the pancreas.
Preoperatively this localization represents a real diagnostic challenge,8,9,11–13 and even with ultrasound and CT the differential diagnosis problem with the pancreatic pseudocyst and pancreatic cystadenocarcinoma, especially in mono-vesicular forms, may not be solved.1,2,10 The treatment of choice is radical surgery (cystectomy) with maximum conservation of endocrine and exocrine functions of the pancreas.1,2
Hydatid involvement of the digestive tract is more unusual even in the endemic areas of this parasitosis.5,12,14,15 indeed no case was noted in the Tunisian series of Bellil S et al.3 of 256 cases of operated extra-pulmonary HC,3 as well as in the Turkish series of Balik AA et al.12 of 27 patients operated for extra-hepatic intra-abdominal HC,12 whereas only one case of duodenal HC was found in the Ethiopian series of Abebe E et al of 42 patients operated for intra-abdominal hydatidosis.4
Gastrointestinal hydatidosis is exceptionally primitive and isolated;14,15 it is most often associated with disseminated intra-abdominal echinococcosis with multiple organs involvement, or more rarely with diffuse systemic hydatidosis.16,17
Physiopathologically, gastrointestinal echinococcosis may result from a direct digestive localization of HC,14,15 but most often results from the rupture or fistulization in the digestive tract of HC of other localizations;18 there have been reports of perforations and fistulizations of HC of the spleen in the colon,19,20 hepatic HC in the duodenum,21–23 mesenteric HC in the small intestine,24 adrenal HC in the proximal jejunum,25 retro-peritoneal HC in the rectum or appendix,16,26–28 and pancreatic HC in the duodenum.6
Localizations of the different segments of the digestive tract have been reported as sporadic observations: stomach,17 small bowel,14 ileocecal angle,29 colon,5 rectum,30,31 appendix,28,32,33 and Vater ampulla.34
The clinical presentation of hydatidosis of the digestive tract can range from simple digestive discomfort to the acute pseudo-surgical abdomen.14,35 Abdominal pain, abdominal distension, intestinal pseudo-obstructions or abdominal mass may also be reported.14,15,17 More rarely complicated forms of HC of the digestive tract can be seen with presentations of acute appendicitis, appendiceal gangrene with perforation,28 intestinal obstruction,14 single or multiple colonic perforation27 or Low gastrointestinal bleeding (by fistulization/rupture of a splenic HC in the colon).20
The main differential diagnosis of these localizations is with garstointestinal stromal tumors.17 These locations represent real diagnostic and therapeutic challenges and the imaging is not too contributive to the diagnosis of certainty that remains Intraoperative.5 Radical surgery is the treatment of choice.
As rare and unusual as they are, the pancreatic and gastrointestinal localizations of human hydatidosis deserve to be known by hospital practitioners, especially in the endemic countries of this parasitosis. Only early diagnosis and adequate and timely management are the guarantors of a better prognosis for these potentially fatal locations.
None.
Author declares no conflicts of interest.

©2019 Bouomrani, et al. This is an open access article distributed under the terms of the, which permits unrestricted use, distribution, and build upon your work non-commercially.