eISSN: 2373-6372


Case Report Volume 8 Issue 1
Consultant Endoscopic and laparoscopic surgeon, Ronak Endo-laparoscopy and general surgical hospital, India
Correspondence: Vipul Yagnik, Consultant Endoscopic and laparoscopic surgeon, Ronak Endo-laparoscopy and general surgical hospital, 77, Siddhraj Nagar, Rajmahal Road, Patan-384265, Gujarat, India
Received: August 13, 2017 | Published: November 24, 2017
Citation: Yagnik VD (2017) Isolated Superior Mesenteric Artery Dissection: A Rare Cause of Chronic Abdominal Pain. Gastroenterol Hepatol Open Access 7(7): 00269. DOI: 10.15406/ghoa.2017.08.00269
Isolated superior mesenteric artery dissection (ISMAD) is unusual. We present a case of a 30-year-old man who had chronic abdominal pain for three months. Contrast-enhanced computed tomography (CECT) revealed type B superior mesenteric artery dissection (SMAD) without thrombus. The patient was managed conservatively.
Keywords: isolated superior mesenteric artery dissection, chronic abdominal pain, endovascular management
Isolated superior mesenteric artery dissection (ISMAD) is rare. In a series of 6,666 autopsies, the incidence of superior mesenteric artery dissection (SMAD) was 0.06%. There have been 323 cases of ISMAD reported in the literature.1 Chronic abdominal pain due to mesenteric ischemia caused by SMAD is rare. We report a case of type B ISMAD, which was treated conservatively with oral anticoagulants. Therapeutic options include conservative management as in the index case, endovascular management, or open surgical management using bypass or direct surgical reconstruction of the dissection. The treatment guidelines for ISMAD have not been established because of the rarity of the condition.
A 30-year-old male patient presented with abdominal pain and vomiting for three days. He was known to be diabetic and presented to the surgical outpatients’ department with the complaint of abdominal pain, on and off for three months. He did not smoke or drink alcohol. There was no history of hematemesis or melena. On physical examination, the temperature was normal, pulse 110/min, respiratory rate 18/min, and blood pressure 140/86 mmHg. Minimal epigastric tenderness was elicited on palpation and bowel sounds were auscultated. Rectal examination was normal. Laboratory findings were normal with a hemoglobin of 14.3g/dL, hematocrit 42%, platelets 425,000/mm3, and white blood cell count 10,000/mm3. Serum analysis revealed the following: random blood sugar, 332mg/dL; aspartate aminotransferase, 24U/L; alanine aminotransferase, 22U/L; and creatinine, 1.0mg/dL. Coagulation profile including PT with INR and aPTT were normal. An ultrasound of the abdomen revealed normal findings. We performed a contrast-enhanced computed tomography scan, which showed a small contrast-filled pouch in the proximal superior mesenteric artery (SMA) (Figure 1,2). However, all other branches showed normal vascularity and the SMA origin was normal. No thrombus was seen within the lumen of the vessel. 3D reconstruction imaging revealed mild enlargement of the SMA with a contrast-filled pouch (Figure 3). We treated the patient conservatively using low molecular weight heparin and tablet aspirin 150 mg daily for anticoagulation. The patient improved and was discharged on warfarin. He was in followed up for six weeks without any problems, and then was lost to follow-up.
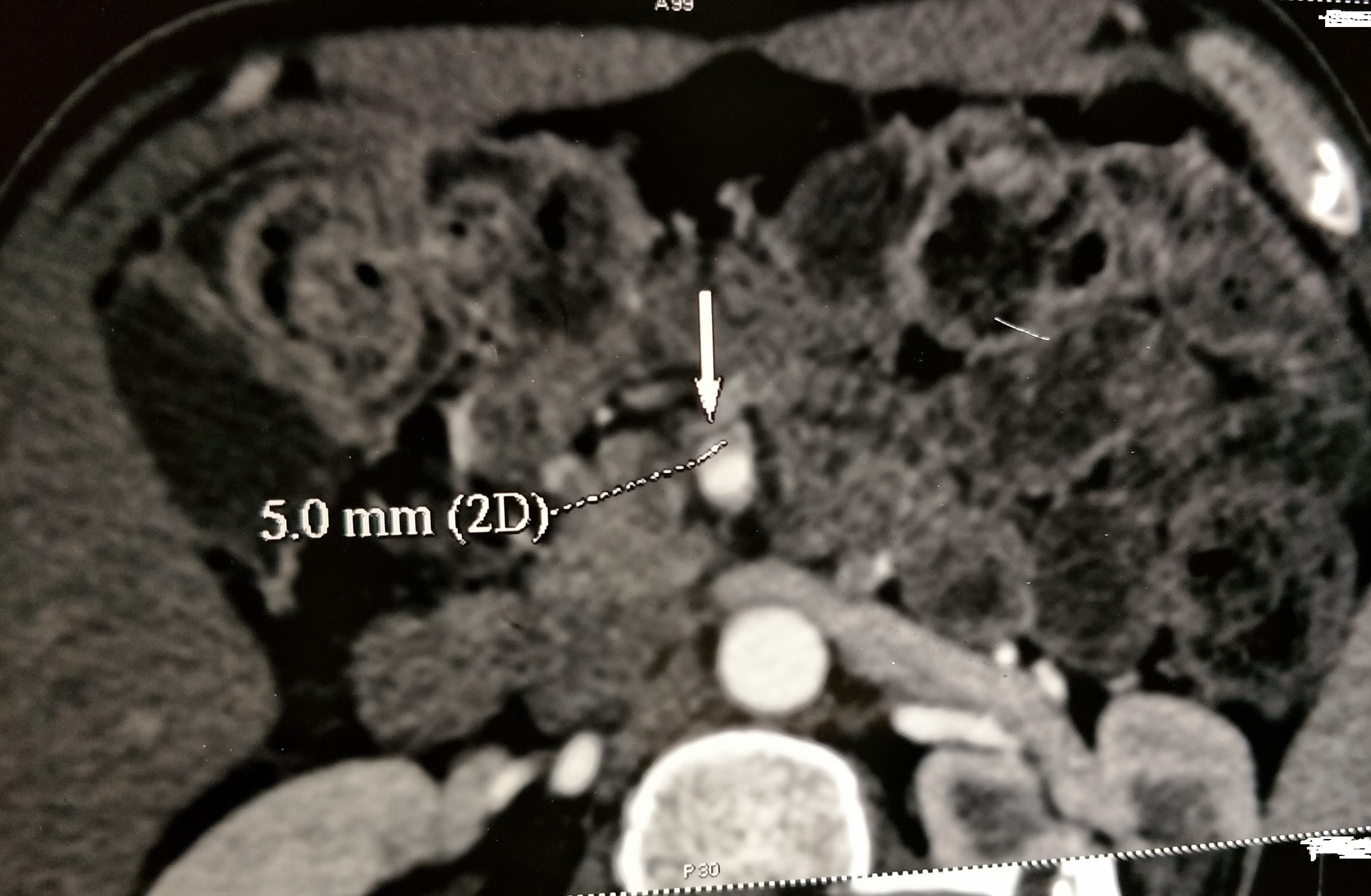
Figure 1 Axial, arterial-phase, contrast-enhanced, CT scan shows Small contrast filled pouch seen in the proximal Superior mesenteric artery.
ISMAD is rare. In a series of 6,666 autopsies, the incidence of SMAD was 0.06%. Since Bauerfield et al first reported the disease in 1941, Luan et al described 296 patients with ISMAD up to 2013.1 Common clinical manifestations include acute abdominal pain, nausea, and vomiting. Ileus, melena, diarrhea and emaciation are other manifestations, while 18 % of patients are asymptomatic.1 Chronic abdominal pain is rare in SMAD and is either due to dissection, vasospasm, inflammation, or mesenteric ischemia. However, 47 of the reported patients did not have any abdominal pain and the dissection was detected only incidentally. An extensive review of the literature by Subhas et al showed that ISMAD occurred more commonly in males. Most cases were reported in the fifth decade of life.2 Predisposing factors for SMAD include hypertension, smoking, cystic medial necrosis, vasculitis, fibromuscular dysplasia, atherosclerosis,3 and, in rare cases, strenuous exercise and trauma. The majority of cases of ISMAD were reported from Asia. This may indicate a genetic predisposition to SMAD in the Asian population.4 A classification based on the location of the SMAD, the Luan classification,5 is as follows:
SMAD may further be classified as grade I (peritonitis absent) and grade II (peritonitis present).6
Although dissection can be seen with the help of Doppler ultrasonography, computed tomography is the preferred imaging modality. Magnetic resonance angiography is an alternative examination, but it often fails to show the small details that computed tomography does. The asymptomatic patient can be managed conservatively. Endovascular intervention is recommended when aneurysmal dilation exceeds 2 cm in diameter, if there is bowel ischemia, or if there is compression of the lumen of greater than 80%.7
Treatment guidelines for ISMAD have not been established because of the rarity of the condition. For grade I ISMAD, most cases might be successfully treated with medical therapy, and endovascular stent placement appears to be an acceptable alternative if medical treatment fails. For grade II ISMAD, endovascular stenting combined with laparoscopic exploration and/or open surgery could be a reasonable option.8,9
ISMAD is rare. Computed tomography is the preferred imaging modality. Therapeutic options include conservative management as in the index case, endovascular management or open surgical management using bypass or direct surgical reconstruction of the dissection.
There is no conflict of interest.
None.

©2017 Yagnik. This is an open access article distributed under the terms of the, which permits unrestricted use, distribution, and build upon your work non-commercially.