eISSN: 2373-6372


Case Report Volume 9 Issue 1
1Gastrointestinal Endoscopy Excellent Center, Department of Medicine, Thailand
2Department of Surgery, Chulalongkorn University and King Chulalongkorn Memorial Hospital, Thailand
3Department of Endoscopic Diagnostics and Therapeutics, Kyushu University Hospital, Japan
Correspondence: Pradermchai Kongkam, Gastrointestinal Endoscopy Excellent Center, Department of Medicine, Faculty of Medicine, Chulalongkorn University and King Chulalongkorn Memorial Hospital, Thai Red Cross Society 1873, Rama 4 Road, Patumwan, Bangkok, Thailand 10330,, Tel +66-2-256-4356, Fax +66-2-652-4219
Received: September 11, 2017 | Published: January 8, 2018
Citation: Kongkam P, Jaruvongvanich V, Tharavej C, Aso A, Osoegawa T et al. (2018) Esophageal Metastatic Sub-mucosal Lesion of Hepatocellular Carcinoma Diagnosed by EUS. Gastroenterol Hepatol Open Access 9(1): 00282. DOI: 10.15406/ghoa.2018.09.00282
Esophageal metastatic lesions are rare particularly of hepatocellular carcinoma (HCC). The majority of reported cases were diagnosed pot-mortem, only a few cases were identified by upper endoscopy. Endoscopic ultrasound (EUS) has never been reported as a diagnostic tool for esophageal metastasis from HCC, nor has EUS-FNA ever been used for this purpose. We reported a 59-year-old male who was under surveillance post liver transplant from HCC 4years ago, had elevated alpha fetoprotein (AFP) at 258.3ng/ml and a positron emission tomography–computed tomography (PET-CT) showing an increased uptake lesion of standardized uptake value (SUV) 7.5 at gastro-esophageal junction. EUS showed a homogeneous hypoechoic mass measuring 35x20mm from the 3rd layer of the distal esophageal wall and EUS-FNA was performed. Cytopathology was consistent with metastatic HCC. The patient expired 20months later from progressive disease with systematic bacterial infection despite multidisciplinary treatments.
Keywords: endosonography, endoscopic ultrasound, eus, hepatocellular carcinoma, esophagus, metastasis, esophageal metastasis, eus-fna
EUS, endoscopic ultrasound; EUS-FNA, endoscopic ultrasound-guided fine needle aspiration; AFP, alpha fetoprotein; PET-CT, positron emission tomography–computed tomography; SUV, standardized uptake value
Esophageal metastatic lesions are rare particularly of hepatocellular carcinoma (HCC). The majority of reported cases were diagnosed pot-mortem, only a few cases were identified by upper endoscopy. Endoscopic ultrasound (EUS) has never been reported as a diagnostic tool for esophageal metastasis from HCC, nor has EUS-FNA ever been used for this purpose. We recently used both EUS and EUS-FNA to diagnose esophageal metastasis.
A 59-year-old male who was under surveillance post liver transplant from HCC 4years ago, had elevated alpha fetoprotein (AFP) at 258.3ng/ml and a positron emission tomography–computed tomography (PET-CT) showing an increased uptake lesion of standardized uptake value (SUV) 7.5 at gastro-esophageal junction (Figure 1). Upper endoscopy showed unremarkable esophageal mucosa so EUS was performed showing a homogeneous hypoechoic mass measuring 35x20mm from the 3rd layer of the distal esophageal wall (Figures 2.1 & 2.2) and EUS-FNA was performed. Cytopathology was consistent with metastatic HCC (Figures 3.1 & 3.2). The patient expired 20months later from progressive disease with systematic bacterial infection despite multidisciplinary treatments.
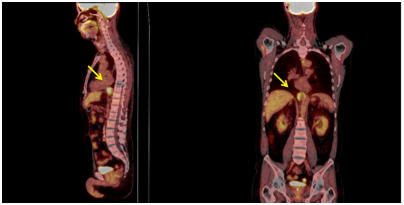
Figure 1 Positron emission tomography (PET) scan showed abnormal uptake of SUV 7.5 at gastroesophageal junction of distal part of the esophagus.
Gastro-intestinal metastasis from HCC is rare with an incidence of only 2%.1 Only 10 cases of the metastases have been reported in the PUBMED (Table 1).2–11 The majority of patients presents with gastrointestinal bleeding, dysphagia and elevated AFP. Diagnosis was mostly made by biopsy from endoscopy.
|
|
Gender/Age |
Presentation |
Diagnostic Method |
Shape |
Tissue Diagnosis |
AFP (ng/ml) |
Survival Time* (months) |
Note |
|
Sohn et al.3 |
M/74 |
Anorexia |
Esophagogram |
Polypoid |
EGD |
ND |
ND |
|
|
Kume et al.4 |
M/56 |
Dysphagia, tarry stool |
EGD |
Polypoid |
Autopsy |
12,200 |
2 |
|
|
Sohara et al.5 |
M/54 |
Melena |
EGD |
SMT |
EGD |
4,987 |
3 |
|
|
Sohara et al.5 |
M/46 |
Hematemesis |
EGD |
Polypoid |
Autopsy |
990 |
7 |
|
|
Cho et al.6 |
M/50 |
Dysphagia, hematemesis |
EGD |
Polypoid |
EGD |
Elevated |
13 |
EUS was utilized |
|
Tsubouchi et al.7 |
M/63 |
Epigastric pain |
EGD |
Polypoid |
EGD |
4,130 |
14 |
EUS was utilized |
|
Choi et al.8 |
M/66 |
Hematemesis |
EGD |
SMT progressed to polypoid in 1 month |
EGD |
3.47 |
7 |
EUS was utilized |
|
Xie et al.9 |
M/50 |
Dysphagia, odynophagia |
EGD |
Polypoid |
EGD |
ND |
More than 7 |
OLT 3y |
|
Hsu et al.10 |
M/54 |
Hematemesis, tarry stool |
EGD |
Polypoid |
EGD |
ND |
4 |
OLT 2y |
|
Fukatsu et al.11 |
M/63 |
Progressive anemia |
EGD |
Polypoid / SMT |
EGD |
ND |
1 |
|
Table 1 Clinical characteristics of patients with HCC with esophageal metastasis were shown in this table
It is hypothesized that esophageal metastasis from HCC came about through the tumor invading the portal vein through hepatofugal portal blood flow12 or direct invasion of tumor cells to the left gastric vein to the esophagus. 7 This case supports a hypothesis of hematogenous spread mechanism of HCC due to the detection of tumor in the submucosa without mucosal involvement.
Based on available information, the majority of esophageal metastases present either as polypoid masses or sub-mucosal lesions which mainly were discovered during endoscopy. EUS were applied in only 3 cases only after the lesions were detected by endoscopy.6–8 In this case, the esophageal metastasis was incidentally suspected from the PET scan. Upper endoscopy did not detect any lesion. Nevertheless, EUS successfully identified the lesion with positive results of HCC from EUS-FNA. This suggests that patients with history of HCC with positive results of PET-CT in the gastrointestinal wall, EUS should be considered as an investigation of choice despite negative finding from endoscopy.
In general, prognosis of esophageal metastasis is extremely poor with an average survival time shorter than 1month.8 Given the fact that this current case was detected in earlier stage than other previously reported cases, his survival time was then longer than other ones.
This case report demonstrated that EUS can diagnose early esophageal metastasis despite negative endoscopic findings. It is hence a potential investigation of choices to search for gastrointestinal wall metastasis including esophagus in patients with positive PET scan. This current case report also supports a hypothesis of hematogenous spreading mechanism of hepatocellular carcinoma.
None.
None.
None.

©2018 Kongkam, et al. This is an open access article distributed under the terms of the, which permits unrestricted use, distribution, and build upon your work non-commercially.