eISSN: 2373-6372


Review Article Volume 6 Issue 2
Institute of Liver Disease and Liver Transplant, India
Correspondence: V Jayanthi, Global Health City, Chennai, India, 600020, India
Received: October 27, 2016 | Published: February 9, 2017
Citation: Jayanthi V, Jain M, Vij M, Varghese J (2017) Natural History of Non Cirrhotic Portal Fibrosis - a Tropical Experience. Gastroenterol Hepatol Open Access 6(2): 00185. DOI: 10.15406/ghoa.2017.06.00185
Non cirrhotic portal fibrosis is a clinical entity of uncertain etiology. The disease is usually non progressive, though a subset of patients may progress to progressive liver failure. Various factors have been implicated in the causation of the disease. The present review highlights the natural history of this entity.
Non-Cirrhotic Portal Hypertension (NCPH) includes Extra Hepatic Portal Vein Obstruction (EHPVO) and Non-Cirrhotic Portal Fibrosis (NCPF). The natural history of NCPH especially NCPF is not clear. Non-cirrhotic portal fibrosis (NCPF) is a clinical entity of uncertain etiology that is typically characterized by periportal fibrosis due to involvement of small and medium branches of the portal vein, resulting in the portal hypertension.1 In Japan this is referred to as idiopathic portal hypertension. In rest of the of the world it has been named as hepatoportal sclerosis,2,3 non cirrhotic intrahepatic portal hypertension (NCIPH)4 and idiopathic non cirrhotic intrahepatic portal hypertension (INIPH).5 From Southern India, the same clinical entity is being described as non cirrhotic idiopathic portal hypertension (NCIPH) and is considered as an important cause for cryptogenic cirrhosis with confirmation on liver biopsy.6,7
In India, in the early 1990’s, NCPF was an important cause for NCPH and was increasingly reported from the northern parts of Indian subcontinent and constituted 15–30% of all causes of presinusoidal portal hypertension.8,9 However, its incidence has decreased considerably over a period of time.1 The present review highlights the literature focusing on the natural history of NCPF with personal observations made on this clinical entity during clinical practice.
Clinico - pathological correlation in NCPF
Clinically, patients with NCPF are young men in the third and fourth decade of life.8,10–12 They usually present with recurrent well tolerated upper gastrointestinal bleed, requiring multiple blood transfusions, compensated in most instances, with a mild to moderate hepatomegaly, a massive splenomegaly, anemia and thrombocytopenia.11 Approximately, 10%-34% do present with ascites.13 Death in these patients is often due to a variceal bleed rather than liver dysfunction.
Natural history
NCPF is often considered as non progressive, though 10% may manifest present with ascites, an acute on chronic liver failure and even end stage liver disease. Survival is prolonged with complete asymptomatic intervals once variceal bleed is controlled by either endoscopic eradication of varices or reduction in portal pressure by a surgical shunt.
Gross and histopathological description
The spectrum of gross findings in NCPF ranges from those seen in EHPVO and that seen in early cirrhosis.
On gross pathological specimens: The liver is either normal sized, enlarged, or at times even shrunken. The surface is likewise either smooth, bossalated, wrinkled, or may show surface nodularity simulating cirrhosis. Fibrous thickening of capsule of the liver with increased vascularity is frequently seen.14–16 The most consistent finding in the portal venous system is the dilatation of the main portal vein with thick sclerosed walls, together with thrombosis in medium and small portal vein branches, referred to as obliterative portal venopathy.17
On histopathology: Typical findings within the intrahepatic portal venous system are :
Parenchymal changes: These include, thin incomplete periportal / perisinusoidal septal fibrosis, preserved lobular architecture and differential atrophy.18–20 Incomplete septal cirrhosis and nodular regenerative hyperplasia may also be associated with NCPF or idiopathic portal hypertension and may be the late manifestation of this clinical entity.21–23
Intrahepatic portal veins: Findings include sinusoidal dilatation ((megasinusoids), obliterative portal venopathy i.e. luminal narrowing or obliteration of small portal venous branches (third degree branches and thereafter) accompanied by dense deposit of elastic fibers, increase in number of portal vascular channels (portal angiomatosus simulating intrahepatic portal cavernoma) and dilated portal veins herniating into the surrounding parenchyma (paraportal shunt vessels)
Portal venous trunk: The major portal vein shows thickening of the wall, endophlebosclerosis, intraluminal thrombosis and even calcification.17
Pathogenesis
The aetiology remains elusive. Some of the aetiological factors incriminated include arsenicosis,24,25 immunological abnormalities26 imbalance of von Willebrand factor and ADAMTS13,27 schistosomal infection and E coli sensitisation.28,29 Pathogenetic mechanism is unclear. Wanless hypothesised that the obliteration of portal venules results in progressive distortion of intrahepatic circulation with subsequent parenchymal remodeling.19 There is atrophy of the hepatocytes in areas with reduced portal blood supply and compensatory hyperplasia of the hepatocytes in well perfused areas, similar to that seen in partial nodular hyperplasia and nodular regenerative hyperplasia variants of intrahepatic NCPH.20 Eapen and others in recent publications27 on NCIPH, have incriminated fall in von Willebrand factor and a corresponding increase in ADAMTS13 as one of the likely triggers towards endophlebitis, formation and progression of thrombosis within the intrahepatic portal venous radicles, ischemia to neighboring hepatocytes and further progression to fibro cirrhotic changes.
On follow up of these patients, there is increasing evidence that in 20 to 33% of cases, the liver undergoes slow parenchymal atrophy due to reduced blood supply to the periphery, nodular transformation of the liver with extensive subhepatic (insular fibrosis) and portal fibrosis. In addition, the lack of compensatory hepatic arterial changes results in worsening of ischemia and this further contributes to liver cell failure.30
Clinico - pathological correlation
A study from North India reported an overlap of clinical features of NCPF and cirrhosis in around 5% of patients with idiopathic portal hypertension. These patients terminally, developed ascites, jaundice, and hepatic encephalopathy making it difficult at times to differentiate this from end stage liver disease due to cirrhosis.31 Ten patients with hepatitis C (5 patients), hepatitis B (one patient) or non alcoholic fatty liver disease (4 patients) had characteristic portal vein changes. The existence of two aetiological possibilities i.e. virus and NCPF in a given patient is likely to result in rapid progression to ESLD.
Histopathological description of explant livers in these patients had shown areas of closely placed nodular hyperplastic parenchyma separated by compressed hepatocytes, portal fibrosis, mega sinusoids and hepatic peliosis. The major portal vein and its medium sized branches had variable grades of obliterative changes, the veins being replaced by fibrous intimal thickening with luminal compromise with or without thrombosis.32
Bernard et al.33 observed that few patients with idiopathic portal hypertension behaved like end-stage liver disease and developed features of decompensation in the form of ascites, jaundice and hepatic encephalopathy during the course of illness. In a subset of patients with NCPH, complications such as acute or chronic liver failure or an end stage liver disease with decompensation,34–39 and hepatopulmonary syndrome are severe enough to warrant a liver transplantation.40,41 We had an opportunity to study, the gross and histology in liver explants (MJ) of 2 (both men) of 57 patients (3.5%) with a pre - transplant diagnosis of cryptogenic cirrhosis but had NCPF in the explant specimen. Grossly, the liver (Figure 1) showed patchy surface nodularity. The cut surface showed vague nodulartity. The capsule was mild thickened. Light microscopy revealed variable portal expansion with dense fibroelastosis; fibrous septa were seen extending from the portal tracts into adjacent lobular parenchyma linking with other portal tracts (portal to portal fibrosis) and the central veins (portal to ventral vein). Crowding of the portal tracts was also appreciated. The portal veins show fibrointimal thickening, medial muscular hypertrophy and narrowed lumen in foci. Few aberrant blood vessels immediately adjacent to the peripheral portal tracts are noted. Obliterated portal veins with increased portal vascularity was also noted. The lobular parenchyma showed patchy macrovesicular steatosis along with mild ballooning and sinusoidal dilatation. The central vein also showed thickening of the wall in foci. Nodular regenerative hyperplasia was also noted (Figure 2). Thus features of NCPF were noted in both the liver explants of “cryptogenic cirrhosis” cases.
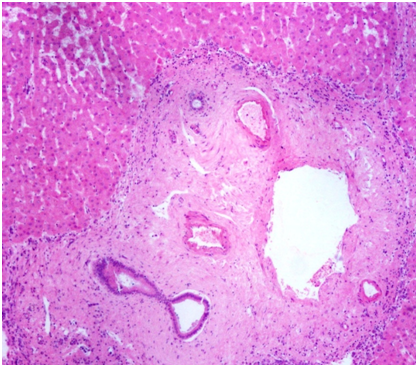
Figure 2 Light microscopy displaying dense portal fibrosis with portal vein thickening and luminal narrowing.
In a retrospective observational follow up study between 2001 and 2010, the senior author in their series of 34 patients (men age 24.9 years; male: female ratio 1:1.8) with a clinical, biochemical and ultrasonography features of NCPF, observed that at end of study, 20 (58.82%) patients had no progression of stage of liver disease while 14 (41.17%) progressed to cirrhosis over a mean period of 5.2 years. The longest follow up was for 10 years. Follow up with ultrasound and liver function tests at 6 monthly intervals, showed a significant reduction in size of the liver in 8 with differential enlargement of right and left lobes in the remaining 6. Eight patients developed ascites and required diuretics. These were patients who had classical and were followed up at 6 monthly intervals for progression of the problem until December 2010.42 Literature review and personal observations both clinically and in explant livers, has undoubtedly outlined that NCPF is indeed a dynamic state wherein there is progression of intrahepatic fibrosis secondary to phlebosclerosis of large and medium sized intrahepatic portal venous system; aetiology and pathogenesis remains speculative.
In conclusion few important messages are forthcoming on natural history of NCPF:
None.
The authors declare no conflict of interest.

©2017 Jayanthi, et al. This is an open access article distributed under the terms of the, which permits unrestricted use, distribution, and build upon your work non-commercially.