eISSN: 2373-6372


Research Article Volume 5 Issue 2
1Department of Pediatrics, All India Institute of Medical Sciences, India
2Service of pediatric gastroenterology and hepatology, Department of Pediatrics, Cliniques Universitaires St Luc, Belgium
3Department of Radiodiagnosis, All India Institute of Medical Sciences, New Delhi, India
Correspondence: Sharat Varma, Service of pediatric hepatology and gastroenterology, Cliniques universitaires St Luc Avenue Mounier 52, B1200, Brussels, Belgium, Tel 32 (0) 2 764 52 76
Received: June 16, 2016 | Published: August 24, 2016
Citation: Varma S, Jana M (2016) MRI in Primary Intestinal Lymphangiectasia: A Diagnostic Tool and to Delineate Localization of Involvement.Gastroenterol Hepatol Open Access 5(2): 00137. DOI: 10.15406/ghoa.2016.05.00137
Introduction and aims:Intestinal lymphangiectasia (IL) is a rare protein losing enteropathy caused by congenital malformation or obstruction of the intestinal lymphatic system. Determining presence and extent of involvement is challenging, as if the region of involvement is further to the duodenum it’s not visualized by upper GI endoscopy. Computerized tomography (CT) scan and video capsule endoscopy (VCE) can be used but their use is limited by size of capsule endoscope and radiation exposure in CT scanning. Hence we evaluated MRI for confirming the diagnosis and evaluating the extent of intestinal involvement.
Methods and patients:4 children with confirmed primary IL underwent MRI scan to evaluate dilated lymphatics and extent of disease.
Image analysis:Images were analyzed for the presence of bowel wall thickness, presence of intestinal obstruction, mesenteric lymphangiectasia, hypodense intramural focus in bowel wall, T2WI hyper‒intense focal area in the bowel wall and any other associated abnormality.
Results:Bowel thickening and dilated lymphatics seen as tubular hyper‒intense channels in the sub‒serosal layers within the small bowel walls were seen. Segmental localization to isolated jejunal involvement was observed in one patient.
Conclusion:MRI can be used to diagnose and evaluate extent of involvement of intestinal lymphangiectasia.
Keywords:Intestinal lymphangiectasia, Protein losing enteropathy, Magnetic resonance imaging
IL; Intestinal lymphangiectasia, CT; Computerized tomography scans, MRI; Magnetic resonance imaging, VCE; Video capsule endoscopy
Intestinal lymphangiectasia (IL) is a rare protein losing enteropathy caused by congenital malformation or obstruction of the intestinal lymphatic drainage system.1 Elevated pressure in the intestinal lymphatic system causes dilatation and rupture of the lacteals, with loss of lymphatic fluid which is rich in fat and protein. Consequently the clinical features of diarrhea, growth retardation, edema, ascites and hypo‒proteinemia develop.1,2 Depending on the presence of an underlying etiology IL could be classified as primary or secondary. Primary IL (PIL) also known as Waldman disease is rather rare entity with not more than 200 cases reported so far.2,3 Given the rarity of PIL the evaluation and management strategies have not changed much over the past decade.2 There have been reports on successful usage of computerized tomography (CT) scan and video capsule endoscopy (VCE) to diagnose and delineate the extent of intestinal involvement.4-12 The significance of determining the extent of involvement lies in the good response to surgical excision of the involved intestinal segment if a localized disease is present, as medical management outcomes are modest and often frustrating.13-15 Localized involvement poses a problem of diagnosis as well, if the region of involvement is further to the duodenum and not under direct visualization in the screening upper GI endoscopy. The utilization of VCE and CT scan for diagnosis and localization of disease in children is associated with issues related to size of capsule endoscope and the radiation exposure in CT scanning. Hence we tried to analyze the usage of MRI and as a diagnostic tool and also for localization of the disease in children with PIL.
Children diagnosed with IL were included in the study as per the criteria listed in Table 1. After inclusion in the study, each child underwent MRI scan.
MRI imaging was performed on a 1.5 T scanner (Magnetom Avanto; Siemens, Erlangen, Germany). Older children underwent imaging without sedation, whereas younger children needed intravenous sedation. Images were acquired in coronal and axial planes. The sequences acquired were
|
Inclusion Criteria (Confirmation of PIL as per Criteria Below) |
|
Histological confirmation of IL on intestinal biopsy |
|
Serum hypoalbuminemia |
|
Increased stool A1‒AT (>24ml/24hr without |
|
Diarrhea and >56ml/24hr without diarrhea) |
|
Increased fecal fat |
|
Absence of proteinuria |
|
Exclusion Criteria (Exclusion of Secondary IL ) |
|
Cardiac abnormalities on echocardiography |
|
Tuberculosis |
|
HIV infection |
|
Presence of clinical hemi‒hyprtrophy |
Table 1 Criteria of children diagnosed with IL
Image analysis
Images were analyzed for the presence of bowel wall thickness, presence of intestinal obstruction, mesenteric lymphangiectasia, hypodense intramural focus in bowel wall, T2WI hyper‒intense focal area in the bowel wall and any other associated abnormality.
Four patients were included and their clinical characteristics are detailed in Table 2. The mean age of symptomatic presentation was 44.25 months (1‒109 months) while mean interval between onset of symptoms to diagnosis was 15.5 months (3‒26 months). The main presenting complaint was chronic diarrhea in 3 of 4, while 1 had presented with repeated episodes of generalized edema. All had features of protein losing enteropathy, high fecal fat, lymphangiectasia on biopsy and no underlying etiology for the IL could be identified. The imaging findings were of diffuse bowel thickening, tubular hyper‒intense channels within the sub‒serosal layer of the small bowel (Figure 1). One patient showed segmental localization, with limited involvement of the jejunum (Figure 2a & 2b).
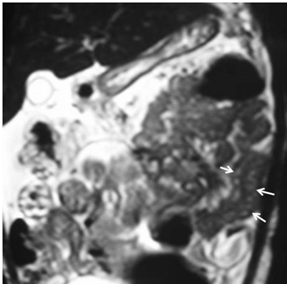
Figure 1 Coronal HASTE MR image shows ascites and diffuse thickening of the small bowel loops. There are multiple tubular and hyperintense channels in the jejunal wall (arrows).
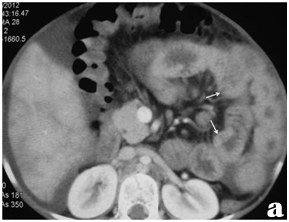
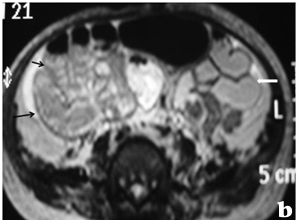
Figure 2 MR images of a 11 month female child with intestinal lymphangiectaisa. Coronal HASTE (a) and axial T2W spin echo fat saturated (b) images show ascites and diffuse thickening of the mid and distal jejunal and ileal loops. There are multiple tubular and tortuous hyperintense channels in the jejunum (arrow); note the normal thickness of the proximal jejunal walls (block arrow).
|
Child 1 |
Child 2 |
Child 3 |
Child 4 |
Demographics |
||||
Age at first presentation (months) |
6 |
1 |
58 |
86 |
Age at diagnosis (months) |
9 |
11 |
84 |
109 |
Time between presentation and diagnosis (months) |
3 |
10 |
26 |
23 |
Gender |
Male |
Female |
Male |
Female |
Clinical features |
||||
Main symptom |
Diarrhea |
Episodic Anasarca |
Diarrhea |
Diarrhea |
Chronic diarrhea |
Yes |
No |
Yes |
Yes |
Generalized edema |
Yes |
Yes |
No |
Yes |
Ascites |
No |
No |
Yes |
Yes |
Biochemical findings |
||||
S. Protein (mg/dl ) |
1,9 |
2,7 |
3,3 |
3,1 |
S. Albumin (mg/dl) |
0,6 |
1,9 |
1,6 |
2,2 |
72 hour fecal fat test ( Normal :< or = 7 gm/day) |
Increased |
Increased |
Increased |
Increased |
Stool alpha‒1‒AT (mg/ml) (Normal :< or = 54 mg/ml) |
140 |
180 |
120 |
210 |
Endoscopic findings |
||||
White spots on duodenal mucosa on upper GI endoscopy |
Present |
Present |
Present |
Present |
Intestinal biopsy histology |
||||
Dilated lymphatic in mucosa/sub mucosa |
Present |
Present |
Present |
Present |
Villous atrophy |
Absent |
Absent |
Absent |
Absent |
Giardia |
Absent |
Absent |
Absent |
Absent |
Table 2 Amplitude in mill volts of the Lead-1 of electrocardiography in sheep
*Significant (P≤0.05); NSNot significant (P>0.05)
The diagnosis of IL is currently confirmed by the visualization of dilated lymphatics on endoscopy with corresponding histology of the intestinal biopsy specimens. This approach has significant shortcomings as the lymphatics maybe dilated only post prandial and not visualized when the endoscopy and biopsy were performed.3 In addition if the region of small bowel involvement is distal to the duodenum this approach would give a falsely normal result.4-11 This aspect assumes more significance as it’s the patients who have localized involvement, benefit most from a definitive surgery wherein the involved segment would be removed and the patient would lead a normal life, with normal no dietary restrictions thereafter.13-15 The missed diagnosis of IL by endoscopy and biopsy has been reported to be as high as 14%.2 VCE has proven to be useful in such cases and has aided in establishment of the diagnosis of IL. In children the VCE is more difficult to perform in comparison to adults on account of the size of the capsule. The cost and availability of VCE continue to be a hindrance to its widespread usage as well. Imaging with MRI has been used as non‒invasive diagnostic tools and also for excluding other factors that may cause secondary IL.5,8-10,16,17 The usage of MRI has an inherent advantage over CT and VCE but its findings and utility in children with IL have been rarely reported.
In our study of 4 children with PIL, which is a rather rare disease with approximately 200 cases reported; we have find MRI to be accurate in diagnosis and segmental localization. We found findings on MRI to be bowel wall thickening, bowel wall enhancement and intramural hyper‒intensities in the affected bowel wall (Figure 1 & 2). All the 4 patients had bowel wall thickening and 3 of the 4 had intramural linear hyper‒intense signal intensity on T2WI MRI (Figure 1 & 2). One patient demonstrated localized involvement of the distal jejunal loops only on imaging (Figure 2). The sensitivity of MRI to detect lymphangiectasia on the basis of bowel wall thickening is 100% (taking endoscopy and biopsy as gold standard) while it was 75% if the finding of T2WI hyperintense linear signal intensity in the bowel wall was taken as a diagnostic criteria. Specificity could not be calculated as there was no ‘true negative’.
The MRI has distinct advantages as it avoids ionizing radiation exposure and usage of contrast media. In our series, MRI was successfully performed in all of the four children. The scanning time was 25‒30 minutes. In smaller children and infants, respiratory triggered sequences were used as the imaging was performed under general anesthesia. The technical drawbacks related to MRI abdomen in our study group included lack of proper luminal distension, and artifacts due to peristaltic activity/ respiratory movements. The artifacts due to peristalsis were not significant to cause diagnostic dilemma. The spatial resolution required for delineating the fine details of the bowel wall was achieved on MRI. Hence the MRI should be used as imaging modality of choice rather than the CT scan and in cases where due to practical reasons VCE is not possible; especially in younger children. From the statistical point of view, the study had limitations in terms of lack of control group and a small number of study population. Thus imaging studies, preferably MRI, in children could provide imaging features to provide indirect pathological evidence of intestinal and mesenteric lymphangectasia and support the diagnosis in the case of a normal endoscopic and histological examination when there is a strong clinical suspicion. Further they should be used to identify the extent of disease involvement and guide surgical treatment if possible.
Informed consent taken from parents of minor children.

©2016 Varma, et al. This is an open access article distributed under the terms of the, which permits unrestricted use, distribution, and build upon your work non-commercially.