eISSN: 2373-6372


Research Article Volume 4 Issue 3
Hospital Británico de Buenos Aires, Facultad de Medicina de la Universidad Católica Argentina, Argentina
Correspondence: Juan Carlos Patrón Uriburu, Servicio de Coloproctología (Department of Coloproctology), Hospital Británico de Buenos Aires (British Hospital of Buenos Aires), Perdriel 74, Ciudad Autónoma de Buenos Aires, Argentina
Received: December 23, 2015 | Published: March 22, 2016
Citation: Patrón Uriburu, Cillo M, EstefanÃa D, Ruiz H, Fernandez L, et al. (2016) Enhanced Recovery After Surgery (ERAS) Implementation of aProtocol in Laparoscopic Colectomy, Initial Experience in a Single Institution in Argentina. Gastroenterol Hepatol Open Access 4(3): 00101. DOI: 10.15406/ghoa.2016.04.00101
Background: An ERAS protocol is a set of guidelines to improve perioperative care. Its application in conventional colorectal surgery should be considered the new standard; its advantages in laparoscopic surgery are discussed.
Objectives: To evaluate the applicability of ERAS in laparoscopic colorectal surgery. Secondary objective: comparative analysis of early results.
Setting: Hospital Británico de Buenos Aires (British Hospital of Buenos Aires). Design: Retrospective. Population: 35 patients operated on by laparoscopy within the ERAS protocol (A), compared to a similar control group (B), outside the ERAS protocol. Period: March 2011 to August 2012. Method: the applicability of all steps of the protocol was evaluated. The variables compared were fluid management, tolerance of diet, intestinal transit, length of hospital stay, complications, mortality and readmission rate.
Results: Group A: 8.57% referred not to have fully understood the protocol, 25.71% did not meet preoperative indications. 28.5% had no epidural catheter. 80% of patients received adequate hydration. 43% did not ingest the preparation of carbohydrates. 80% received early feeding; mobilisation was delayed in 28.5%. Intraoperative fluid infusion in group A was significantly lower than in controls. Group A tolerated liquids and solids earlier than controls. In group B, one more litre of parenteral hydration was used during hospitalisation. Passage of stool occurred earlier in group A than in controls. Overall morbidity was not significant. The length of stay was significantly lower in group A. Readmission was similar. There was no mortality.
Conclusion: It is possible and safe to apply an ERAS protocol in laparoscopic colectomy with an acceptable compliance in our hospital, with a faster discharge and the same rate of readmissions.
Keywords: fast-track surgery, enhanced recovery, laparoscopic colectomy
In the last two decades, colorectal surgery has made a historical qualitative leap forward with the consolidation of laparoscopic surgery for benign disease, and more recently for malignant.1–9 Soon after the report on the first laparoscopic colectomy, a Danish surgeon called Henrik Kehlet10 published a small series of patients with colorectal disease operated on with open surgery, achieving an average hospital stay surprisingly similar to the one of laparoscopy. He had implemented a package of measures to improve perioperative care, called a ‘fast-track’ protocol, a term that at present has been replaced by the acronym ERAS (Enhanced Recovery After Surgery) or multimodal rehabilitation.
An ERAS protocol consists in combining multiple techniques, such as epidural anaesthesia, minimally invasive techniques, optimal pain control and aggressive rehabilitation, including early oral feeding and forced mobilization.11 This new approach begins with improvements since the preoperative phase, which until then had not been taken into consideration. Another significant difference with conventional care is that every guideline applied is based on strong evidence and subjected to periodical revisions and modifications.12
The application of a multimodal standardised care programme in abdominal surgery is reflected on the reduction in hospital stay, with a more efficient use of beds and hospital resources, and potentially fewer errors in perioperative management due to standardization.8 Randomised studies showed a reduction in hospital days without compromising the safety of the patients, with a lower morbidity and a readmission rate similar to the one of colonic surgery with conventional care.14
The usefulness of the implementation of such protocols in colorectal laparoscopic surgery has been widely discussed. The Dutch prospective randomised LAFA trial, published in 2011, clearly shows how the patients who underwent laparoscopy benefited from multimodal care, with a shorter hospital stay and lower costs than those who were under conventional care and had undergone laparoscopy or open surgery.15
The successful implementation of an ERAS programme requires team training, an adaptation of the protocol to the same hospital environment in which it will be applied and constant monitoring and improvement of the medical team, as continuing education is one of its cornerstones at all levels, from the patients to the medical and non-medical staff.16,17 In 1994, Salomón et al.,18 report one of the first experiences in Argentina with the laparoscopic approach in colorectal surgery.18 Today, most elective surgeries are performed in this manner in our institution. In 2010, we introduced in our working team the concept of multimodal care (ERAS) and started by planning a protocol to be applied in our context with the hypothesis of reducing the global morbidity of colorectal surgery with conventional care, which is around 15 to 30% according to different series, both for the laparoscopic approach and for the conventional one.9–19
Objectives
The primary objective was to assess the applicability of an ERAS protocol in elective laparoscopic colorectal surgery and the secondary objective was to undertake a comparative analysis of the initial results of the series.
A retrospective analysis was carried out including all the patients who underwent successive laparoscopic surgeries of benign and malignant disease not selected according to the guidelines of an ERAS protocol, included in a prospective database of the Department of Coloproctology of the Hospital Británico Buenos Aires. The period analysed covers from March 2011 to August 2012.
The name ‘ERAS protocol’ was given to the adjusted, modified guidelines taken from the LAFA14 study (Table 1). These were agreed upon by the different intervening departments. Their applicability was assessed in pilot tests, until a coordinated performance from pre-, intra- and postoperative care was achieved. Once the protocol was fine-tuned, it went through another adjustment and finally approved for implementation by the ethics committee.
|
ERAS (Group A) |
Conventional care (Group B) |
Preoperative phase |
||
Doctor’s office |
Information on ERAS protocol |
As usual |
Informed consent |
Informed consent |
|
Anaesthesiology consultation |
Explain types of anaesthesia |
No |
Psychological consultation |
Yes |
No |
Previous day |
||
Mechanical bowel preparation |
No |
Yes (phosphates) |
Left colon; Enemol® / Microenema®: 1x at night |
||
Last meal |
6 h before surgery (NO FIBRE) |
Previous night |
Fluids |
pHB preparation 500 cc |
As usual |
Anxiolytic (before sleeping) |
Lorazepam 1 mg |
No |
Day of admission |
||
First thing in the morning (afternoon surgery) |
Breakfast 6 h before surgery + 250 cc of pHB preparation |
As usual |
Two hours before surgery |
pHB preparation 250 cc |
No |
Anaesthesia |
||
Hydration |
Fluid restriction (FL: Ringer 1500 cc) |
At the discretion of the anaesthesiologist |
Antiemetic |
Ondansetron 4 mg |
At the discretion of the anaesthesiologist |
Epidural catheter |
T6–T10; first dose of bupivacaine 0.25% with adrenaline 1:200.000, 8–10ml + morphine 2 mg |
NO |
Infusion: bupivacaine 0.125% + fentanyl 2 mcg/ml-10ml/h in the 48-h postoperative period |
||
General anaesthesia |
Balanced |
As usual |
Hypotension |
Decrease in B P> 20%, vasopressor |
At the discretion of the anaesthesiologist |
Thermal blanket |
Obligatory |
Optional |
Drains |
No |
Optional |
NG tubes |
No |
Optional |
Immediate postoperative phase |
||
2-h postoperative period |
Forced mobilisation |
Mobilisation on demand |
p HB preparation 250 cc |
- |
|
Diet |
Nil per mouth |
|
Analgesia |
With continuous infusion pump through epidural catheter |
As usual |
IV rescue (avoid opioids) |
||
First postoperative day |
||
Normal diet |
Liquids |
|
p HBpreparation1 litre |
No |
|
FL 21ml/h |
FL as usual |
|
Lactulón® or Agarol® 1 do seat night |
No |
|
Remove Foley catheter |
Assess Foley catheter removal |
|
Forced mobilisation (6 h out of bed) |
Mobilisation on demand |
|
Second postoperative day |
||
Withdraw FL |
Assess withdrawal of FL |
|
Remove epidural catheter / analgesia p.o. |
Usual analgesia |
|
Normal diet |
Diet as tolerated |
|
Mobilise 8 h out of bed |
Mobilisation on demand |
|
|
Plan discharge |
Evaluate discharge |
Table 1 Adapted ERAS protocol,br>FL, fluid loading
The 35 initial patients were identified for analysis; they were designated as ‘group A’. In the search for a control group, the month of August 2012 was used as cut-off date, selecting the last 35 patients who underwent laparoscopies performed by the same surgical team, outside of the ERAS protocol, and who met the exclusion criteria described in detail below; these were designated as ‘group B’. An analysis of the demographics (age, gender, ASA class, pathology and surgery type) was carried out in order to determine the occurrence of preoperative factors that would prevent group comparison. The following exclusion criteria were considered for both groups:
The compliance or applicability of every step of the protocol was assessed with percentage points from 0 to 100 and carried out by means of interviews with patients and the revision of medical records.
The variables analysed in group A were: for the preoperative phase, whether patients understood the protocol and whether they had complied with it; for the intraoperative phase, percentage of patients that had an epidural catheter placed and of those that received an adequate fluid volume; and for the postoperative phase: whether the intake of fluids and solids was adequate according to the protocol, whether the quantity of liquids administered parenterally was correct, whether laxatives were prescribed, how many mobilised early and how many received physiotherapy. The variables compared were intra- and postoperative fluid management, tolerance of diet, intestinal transit, days of hospital stay, complications, mortality and 30-day readmission rate. In order to simplify the analysis of the sample, those resections involving from the cecum to the splenic flexure were regarded as right colectomy, and left colectomy were those involving from that point up to and including the upper rectum.
As regards mechanical bowel preparation, it consisted in the traditional method using oral laxatives (phosphate or polyethylene glycol) the day before surgery. In the case of patients who did not receive mechanical bowel preparation and had to undergo anastomosis of the left colon using the double-suture technique, a commercial enema was used before being admitted to the hospital the morning of the surgery or a rectal lavage was performed in the operating room after anaesthesia, depending on the preference of the performing surgeon.20–24
Every aspect of the protocol was explained in detail to each patient in group A; they were sent instructions in a PDF file by email with details of how to prepare for their surgery and what it consists in. They were also emailed instructions for respiratory therapy for the preoperative phase and a third file with nutritional recommendations; each of them was prepared by the respective department. Since the preoperative phase, all patients were given contact information for them to contact the surgical team by email or telephone should they have any doubts interpreting the instructions or any concerns once they were discharged from the hospital.
Regarding early ambulation, it involved the forced mobilisation out of bed aided by a physiotherapist, a nurse or a relative of the patient two hours after arrival to the room. Early feeding consisted in the oral intake of a light diet within 24 hours after surgery, without waiting for the auscultation of bowel sounds or the passage of flatus or stool.25–28
The carbohydrate-based liquid mixture developed by the Department of Nutrition was given the name Preparado Hospital Británico (pHB; British Hospital Preparation). The patients were instructed to drink it two hours before and two hours after surgery. It was intended to be as similar as possible to Nutriciapre Op®, which is used in other countries as preoperative beverage and it is not available in the national market.29 As regards pHB, it consists of Powerade® with the addition of one sachet or teaspoonful of sugar per bottle.
Patients included in group A were followed since the preoperative phase by a multidisciplinary team, whereas patients in group B received the conventional instructions given for the standard preoperative phase of colonic surgery. The fluids administered parenterally during the intra- and postoperative phases were divided in ‘less than 1500 cc’, ‘1500 to 2000 cc’ and ‘more than 2000 cc’.
Hospital stay represents the days in which the patient remains in hospital, from surgery until discharge. Only full days or half days were considered; no hourly records were kept. A full day spans from surgery until the following day before 11 a.m., and regarded successively from then onwards. Discharge criteria included tolerance of oral diet, control of oral analgesia, passage of flatus or stool and the patient’s willingness to leave the hospital. The term ‘readmission’ was used for patients admitted to hospital with any pathology within 30 days of surgery.
Morbidity was defined as any surgery-related adverse event within the following 30 days, classified according to Dindo and Clavien; mortality was also evaluated.30,31 Ileus was characterised as the presence of two or more episodes of vomiting with no passage of flatus. It was regarded as resolved when the passage of flatus with no nausea, vomiting or abdominal distension was confirmed.32 The surgical technique was standard depending on the pathology to be treated, and the number and disposition of the trocars were at the performing surgeon’s discretion. Vascular pedicles were treated intracorporeally. Conversion was defined as any incision performed to complete the surgery not exclusively with the purpose of removing the surgical tool.33
Numerical variables are expressed as mean ± standard deviation or mean and range. Categorical variables are reported as percentages. In order to compare proportions, Fisher’s exact test was used. To compare numerical variables in two groups, Student’s t-test was chosen for independent samples or the Mann-Whitney test, as appropriate. In all cases, values were considered significant if p<0.05. The analysis was performed using Stata 11.0 software.
Preoperative demographics in both groups were comparable. Average age was 61.5 years. There were no statistical differences as regards distribution by gender. Sixty percent of the patients in group A were ASA class III; in the control group these constituted 54% (Table 2). Distributions by disease type and procedure performed were similar in both groups, with no statistical differences. Among the patients in group A, more prior abdominal surgeries were registered than in group B patients (20% and 11%), but with no significant differences (Table 3).
|
Group A |
Group B |
p |
Age (range) |
61.4 (40–83) |
61.5 (42–80) |
0.98 |
Male sex (%) |
17 (48.57) |
16 (45.71) |
0.5 |
ASA III (%) |
21 (60) |
19 (54.3) |
ns |
Malignant disease (%) |
19 (54.3) |
23 (65.7) |
ns |
Prior abdominal surgeries (%) |
7 (20) |
4 (11.43) |
0.25 |
Hemicoloctomy |
9 |
9 |
- |
Hemicoloctomy |
26 |
26 |
- |
Table 2 Demographics
Group A (35) |
Yes (%) |
No (%) |
Understood the protocol |
32 (91.4) |
3 (8.6) |
Complied |
26 (74.3) |
9 (25.7) |
No bowel preparation |
35 (100) |
- |
Epidural catheter |
25 (71.5) |
10 (28.5) |
7 (20)* |
||
3 (8.6)& |
||
Intraoperative FL |
28 (80) |
7(20) |
Intake of pHB 2 h post-op |
20 (57.2) |
15 (42.8) |
Early diet |
28 (80) |
7 (20) |
Postoperative FL |
25 (71.4) |
10 (28.5) |
Received laxatives |
23 (65.7) |
12 (34.3) |
Early mobilisation |
25 (71.4) |
10 (28.5) |
Physiotherapy |
22 (62.8) |
13 (37.1) |
Table 3 *Lack of adherence of the anaesthesiologist &Patient refusal; FL, fluid loading; pHB, prepared Hospital Británico (British hospital preparation)
Protocol application in group A
Preoperative phase: Three patients (8.57%) claimed not to have understood the protocol completely. Nine patients (25.71%) did not comply with the preoperative instructions completely, even though they had previously claimed not to have doubts or objections to them. No patient in group A received mechanical bowel preparation; in group B, every patient received mechanical preparation the day before surgery. Intraoperative phase: No epidural catheter was used in 28.5% (10) of the patients in group A: 2 due to fear, 1 due to a previously undetected spinal pathology, and 7 (20%) due to the anaesthesiologist’s lack of adherence to the protocol. The volume of fluids received following a hydration plan was correct for 80% of the patients. The remaining 20% received a volume of infused fluids larger than expected; in none of these latter cases was arterial hypotension the reason.
Postoperative phase: Almost half of the patients (42.8%) did not drink the pHB preparation for different reasons (due to an oversight, fear, etc.). This delayed the start of the diet in 3 patients (8.57%). Eighty percent of the patients received early feeding; 65.7% were given a dose of oral laxative the day after the surgery. Although 71.5% were mobilised early, mobilisation was delayed in 10 patients (28.5%); 4 (11.4%) due to fear or a limited understanding of the instructions and 6 (17.14%) due to contraindication by nursing and/or internal medicine staff. Only 62% received physiotherapy, in spite of its being prescribed in all cases (Table 3 & Figure 1).
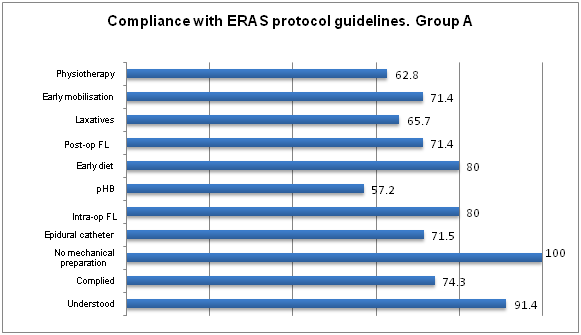
Figure 1 Values correspond to percentage of patients who complied.
Post-op FL, postoperative fluid loading; pHB, preparado hospital Británico [British hospital preparation]; Intra-op FL, intraoperative fluid loading
In comparison, intraoperative fluid management in group A was as follows: 37.2% of the patients received less than 1500 cc, 42.8% from 1500 to 2000 cc and the remaining 20%, over 2000 cc. Comparatively, 68.6% of the patients in group B received high volumes (less than 2000 cc), and the rest between 1500 and 2000 cc; no patient in this group received a low volume or less than 1500 cc. There was a significant difference between both groups with p<0.00001 (Table 4 & Figure 2).
Intra-op fluid loading & (ml) |
Group A (%) |
Group B (%) |
< than 1500 cc |
13 (37.2) |
- |
1500-2000 cc |
15 (42.8) |
11 (31.4) |
> than 2000 cc |
7 (20) |
24 (68.6) |
Table 4 Intra-op: intraoperative (t-test: p<0.00001)
As regards postoperative evolution, patients in group A tolerated the intake of liquids and solids before those in the control group: 4.25 (2–24) h vs 18.2 (12–48) h in the former case, and 27.4 (12–96) h vs 49.2 (24–72) h in the latter; in both cases, the difference was significant (Table 4 & Figure 3). In group A, the urinary catheter was removed significantly earlier (20 vs 42 h) with p = 0.0004. Faster ambulation was also observed in this group when compared to the controls: 10 (2–48) h vs 32 (12–72) h (p<0.0001). In group B, one more litre of parenteral hydration was used during hospital stay (2257 ml), as opposed to 1271 ml in group A, (p<0.0001). In 10 (28.6%) patients in group A, the hydration plan was extended as indicated by the internal medicine staff.
No difference was observed between patients in both groups concerning the passage of flatus (28 vs 36 h; p = 0.07), but bowel movement in patients in group A occurred earlier than in controls (1.2 vs 2.7 days) p = 0.007 (Table 5).
|
Group A |
Group B |
p |
Fluids p.o. (h)* |
4.25 (2-24) |
18.2(12-48) |
0.0001 |
Diet (h)* |
27.4 (12-96) |
49.2(24-72) |
0.0001 |
Mobility |
10 (2-48) |
32(12-72) |
0.0001 |
Fluid therapy |
1271 (1000-3000) |
2257(2000-3000) |
0.0001 |
Urinary catheter (h) |
20.4 (12-120) |
42.9(12-48) |
0.03 |
Passage of flatus (h)* |
28 (12-72) |
36(12-120) |
0.07 |
Passage of stool (days) |
1.2 (0-4) |
2.7 (0-6) |
0.007 |
Hospital stay (days) |
3 (1.5-6) |
4.5 (3-7) |
<0.0001 |
Discharge on second day |
12 (34.28%) |
0 |
|
Discharge on third day |
17 (48.57%) |
3 (8.57%) |
|
Discharge ≥ fourth day |
6 (17.14%) |
32 (91.42%) |
|
Table 5 Post operative phase: n(%), (range)
As regards complications, two patients had arrhythmia in group B and none in group A, with no significant difference. One patient in group A had fever during the postoperative phase, and two in group B. Twenty percent (5/25) had complications related to the epidural catheter, but it was reversible in all cases. Two patients developed pruritus, 2 orthostatism and 1 lower limb paraesthesias. On the other hand, the incidence of postoperative ileus was similar in both groups: 3 (8.5%) patients in group A and 4 (11.4) in group B. The same values were observed concerning surgical site infections. Even though global morbidity in group A was 37% and in group B 42.8%, all complications were grade I and II in the Clavien-Dindo classification; therefore, there were no reoperations in the present series (Table 6).
Complications |
Group A (%) |
Group B (%) |
Clavien-Dindo |
Arrhythmia |
0 |
2 (5.7) |
II |
Fever |
1 (2.8) |
2 (5.7) |
I |
Pruritus |
2 (5.7) |
0 |
I |
Orthostatism |
2 (5.7) |
0 |
I |
Lower limb paraesthesias |
1 (2.8) |
0 |
I |
Ileus |
3 (8.5) |
4 (11.4) |
I |
Surgical site infections |
3 (8.5) |
4 (11.4) |
I |
Reoperation |
0 |
0 |
- |
Readmission |
1 (2.8) |
1 (2.8) |
- |
Mortality |
0 |
0 |
- |
Total |
13 (37.1) |
15 (42.8) |
|
Table 6 Postoperative complications
Global hospitalisation time was 3 days (1.5-6) in group A and 4.5 days (3-7) in group B (p<0.0001). Thirty-four percent of the patients in group A (12) were discharged before completing two days of hospitalisation; in group B, there was no record of patient discharges in that period of time. On the third day, 48.6% (17) of the patients in group A were discharged, and in group B 8.6% (3), whereas on the fourth day, 91% (32) of the control patients were discharged, as compared to 17% (6) in group A (Table 5 & Figure 4). One patient in each group was readmitted: in group A due to abdominal pain, with no pathological findings in follow-up studies, being discharged after 48 h. In group B, one patient was readmitted due to fever of unknown origin. There were no records of mortality in the series (Table 6).
The cornerstones of the ERAS protocol are based on continuing education, not only of the surgeon, but also of the patient and the entire surgical team. This makes its implementation difficult and highlights the need for revisions to assess its applicability. Failures are frequent at any of the levels, especially in the first experiences. Certain points may be highlighted as indispensable and, at the same time, as being applied less in traditional care. For instance, avoiding mechanical bowel preparation; not fasting for more than 6 hours for solids and 2 hours for fluids; consuming carbohydrates during the perioperative phase;34 receiving a good level of analgesia, mainly using an epidural catheter; avoiding opioids; using a low volume of parenteral fluids;35,36 forced mobilisation and early feeding.37–39 Even if it is possible to obtain good results without the implementation of all the measures, multimodal care teams must implement them at the highest possible percentage and this must be monitored throughout the entire process.40
In our series, in spite of the fact that all of the patients included claimed to have understood the instructions, it was established that in 8.5% of the cases there was some degree of error in their interpretation and 25% of non-compliance for different reasons, such as having forgotten or failing to comply due to other factors. However, when more than one person was involved in the compliance with the guidelines, the error rate was higher. This could be observed in the error levels in the postoperative phase care, which are higher than 40%. In a multi-centre series of patients undergoing conventional surgery, Maessen et al.,40 observe a similar experience. The authors suggest that improving compliance in the postoperative phase is the most difficult aspect in the implementation process. This is due to multiple factors, with the organisational factor being the most important. They suggest as a solution to this problem to involve the patient and the family further in their own recovery. Among these measures, they also recommend scheduling surgeries in the morning and early in the week, in order to avoid discharging patients during the weekend.40
A more recent contribution on colorectal laparoscopic surgery combined with an ERAS protocol has found a 31% deviation on average. Having identified as the main negative variable the lack of early mobilisation, the authors state that ileus and analgesic failure are the factors that most frequently delay ambulation.41 When the multivariate analysis was carried out, the pathology and the intraoperative complications were identified as independent predictors of deviation from the protocol. It is easy to understand that complications hinder the applicability of the protocol–which is why they were excluded from the analysis in this series, as well as the conversion. But when the pathology was analysed, the authors were surprised to notice that patients with benign non-inflammatory disease were the ones who deviated the most, with a 56% failure, whereas patients with malignant disease were the ones who complied with the protocol, being regarded as the best model to assess applicability.41
The lack of early mobilisation should be considered a predictor of other failures, and taken as a red flag within the protocol; the same point is noted in the LAFA study.41–45 In our series, 71% of the patients mobilised early, but no multivariate analysis was undertaken to assess patients who did not mobilise early. Another aspect in which difficulties were faced was in the insertion of epidural catheters, in 30% of the cases. The lack of compliance with the use of an epidural catheter by the anaesthetic team was 20%. We believe that this point is one of the most easily solved, since it is part of the education and learning curve, as observed in other experiences.42,43 Despite having registered 5 complications due to this practice, none of them was serious and they were all reversible, but in 3 cases they led to a delay in the discharge.
Another intraoperative variable assessed, fluid restriction, had a higher acceptance (80%). Comparatively, there was better fluid management in group A, as it needed less volume replacement than group B, both in the intra- and postoperative phases.
In the present study, we did not observe a lower complication rate when complementing laparoscopic surgery with an ERAS protocol, as compared to the same surgery combined with conventional care. This is possibly owing to the fact that it is an initial, reduced number of patients. The LAFA study shows similar results as regards morbidity in the four groups compared (laparoscopic surgery with and without ERAS and conventional surgery with and without ERAS), but clearly defines the benefits of combining both of these minimally invasive techniques, which translate into early discharge without a higher readmission rate in the case of laparoscopy with ERAS, considering it as a parameter of best outcome.15 On the other hand, a meta-analysis published recently evaluates 6 prospective randomised trials of malignant colorectal disease operated laparoscopically with and without an ERAS protocol. It observed fewer complications in the group combining laparoscopy and ERAS, with a similar readmission rate.44
In this series we also observed a shorter hospital stay, with the same morbidity and readmission rate as in the control group. Rossi et al.,45 assess the feasibility and safety of early discharge, examining 91 patients that were discharged on the second postoperative day, out of a series of 882 laparoscopic colectomies under multimodal care. They did not observe an increase in complications or in the readmission rate in this group of patients.45 Multimodal care plans were designed to reduce surgical stress and the complications brought about by the wrong implementation of perioperative care.10
Advanced age, malnutrition and comorbidities are factors that delay discharge and increase morbidity in elective colorectal surgery. But, paradoxically, this high-risk group is the one that would benefit the most from multimodal care.46–49 Twenty-eight point five percent (28.5%) and 26% of patients in groups A and B, respectively, were older than 70 years of age, and in both groups over 50% were ASA grade III patients. Selections carried out in order to obtain an early discharge exclude patients with a higher risk of complications. This analysis includes this group of patients, as it does not seek an early discharge from hospital, but rather a lower complication rate in this particular group. It was not the objective of this study to carry out a comparison between risk groups. However, other authors show how safe and advantageous it is to treat high-risk patients with these perioperative care measures.46–49
This series shows the safety and applicability of a protocol under the strict guidelines of the ERAS Group to laparoscopic colectomy, with an acceptable compliance in our field, earlier hospital discharge and the same readmission rate. Future contributions with a larger number of patients are necessary in order to confirm the initial results.
None.
Author declare that there is no conflict of interest.
None.

©2016 Patrón, et al. This is an open access article distributed under the terms of the, which permits unrestricted use, distribution, and build upon your work non-commercially.