eISSN: 2373-6372


Research Article Volume 1 Issue 4
1Department of Gastroenterology, Second Affiliated Hospital, Guangzhou Medical University, China
2Department of Gastrointestinal Surgery, Second Affiliated Hospital, Guangzhou Medical University, China
Correspondence: Man-peng Lin and Hui Yang, Department of Gastroenterology, Second Affiliated Hospital, Guangzhou Medical University, No.250 Changgang Dong Road, Guangzhou, 510260, China, Tel 86-020-34153522
Received: August 24, 2014 | Published: December 3, 2014
Citation: Guo J, Lin M, Zhang D, Yang T, Hong C, et al. (2014) Successful Colonoscopic Sclerotherapy for Bleeding Internal Hemorrhoids with Lauromacrogol.Gastroenterol Hepatol Open Access 1(4):00023. DOI: 10.15406/ghoa.2014.01.00023
Background and aim: Inspired by the success of endoscopic sclerotherapy for the treatment of bleeding gastric varices, we investigated a new minimally invasive method for the treatment of bleeding internal hemorrhoids.
Patients and methods: From 2009 to 2013, 110 outpatients with 2- or 3-degree bleeding internal hemorrhoids underwent colonoscopic sclerotherapy with Lauromacrogol. Patients with mixed hemorrhoids, fistula and fissure were excluded in this study. All patients were visited after 1 week and followed up through a telephone interview after 1 month, 6 months, 1 years and 2 years. 93 patients were performed colonoscopy examination after 1 year or 2 years.
Results: As shown in this study, no patient had immediate complications. Mild postoperative pain occurred in 13 cases (12%) after the initial treatment, but could be alleviated spontaneously without pain medication. 26 patients (23.6%) showed mild self-limiting rectal bleeding one week after the treatment. All patients displayed pelvic infection, rectal prolapse and urinary retentions. Three months later, 95.5% of patients (105/110) were effectively treated. 5 patients carried out another sclerotherapy with injection of Lauromacrogol due to recurrent hemorrhage. A total of 93 patients (85%) were contacted by telephone for a follow-up to document results of the treatment after 1 month, 6 months, 1 year and 2 years. Among them, 70 cases (75%) showed no symptoms. 23 cases (25%) had some residual symptoms including occasional bleeding and prolapse, however, there were no requirements for further treatment. No patients experienced fecal incontinence. The duration of the operation in our study is 16.3±5.1minutes. The total cost of this sclerotherapy with Lauromacrogolis 2536±167.8 Yuan.
Conclusion: Lauromacrogol colonoscopic sclerotherapy therapy is an efficient, cost-effective and simple outpatient treatment for bleeding internal hemorrhoids with minimal complications
Keywords: sclerotherapy, internal hemorrhoids, lauromacrogol, colonoscopy, bleeding
RBL, rubber band ligation; PPH, prolapse and hemorrhoids
Hemorrhoids are the most prevalent anorectal disorder among adults, and it has been stated that up to half of people may experience problems with hemorrhoids at some point in their lives.1,2 Symptomatic internal hemorrhoids lead to nearly 3.5 million physician visits per year at an estimated cost of $500 million.3 Bleeding is the common and severe internal hemorrhoid complain and represent the second most-common colorectal cause of severe hematochezia, however, these patients should undergo colonoscopy or screening flexible sigmoidoscopy to exclude other causes of colorectal bleeding.4
There are different non-operative and surgical therapeutic approaches to internal hemorrhoids bleeding. However, all method for treatment of hemorrhoid has advantages, disadvantages, limitations and complications.5 Sclerotherapy is one of the nonsurgical treatments, which involves the injection of one of a number of sclerosants into the submucosal space of the hemorrhoid to be treated or into the apex of the hemorrhoid itself.6 Sclerotherapy has the advantage of being an easy, fast, and inexpensive outpatient procedure. However, serious complications have been reported after sclerotherapy, including severe rectal pain, hematoma, and perirectal abscesses, as well as sepsis.7–9 Rubber band ligation (RBL) is probably well-accepted and highly efficacious nonsurgical therapy for hemorrhoidal disease. However, RBL was associated with more pain and the occurrence of post-banding pain is variable (1%-50%).10
Chen et al.11 demonstrated that Lauromacrogol injection is a safe and effective sclerosants for esophageal varices. It has similar clinical effects to sodium morrhuate; while it has fewer side effects. The soft tissue reaction that follows causes thrombosis of the involved vessels, sclerosis of the connective tissue, and a refixation of the prolapsing mucosa to the underlying rectal muscular tissue. Inspired by the success of endoscopic sclerotherapy for the treatment of bleeding gastric varices, we investigated a new minimally invasive method for the treatment of bleeding internal hemorrhoids.
Patients and method
Between August 2009 and February 2013, this study enrolled consecutive outpatients with 2- or 3-degree internal hemorrhoids bleeding. Colonoscopy was performed to exclude other sources of bleeding. All of the patients didn’t respond to conservative treatment in clinics or community hospitals. Patients were excluded from these studies, who were with a history of surgical intervention in the anus and rectum for colorectal tumor, anal fissure, anal fistula, hypertrophied anal papillae, blood coagulation disorder, immunodeficiency, pregnant woman, fourth-degree hemorrhoids and other complicated hemorrhoids. The clinical features and personal information were recorded, including bleeding, prolapse, anal pain, abnormal defecation, age, sex, occupation and address.
All treatments were accomplished in the Endoscopy Department of our outpatient clinic. The apparatus included the Olympus colonoscopy (CF-240I or CF-H260AZ/I), Sclerotherapy Needle (25G, Wilson Cook). We injected 10-15ml Lauromacrogol (SHANXI TIANYU pharmaceutical. Co.Ltd, (97) medicine authorized No.H20080445) each patient, according to the size of internal hemorrhoidal bundle. Approximately 1–2 mL of Lauromacrogol was injected into the vessels of the hemorrhoids. Appropriate change of the patients’ posture was needed to make sure the biopsy hole below the colonoscopy lens. Patients were placed in modified left lateral decubitus (Sims’ position) first and changed to supine decubitus and right lateral decubitus when needed. Lauromacrogol was injected in the internal hemorrhoidal bundle around the dentate line in 25-30 angle on the rectal mucosa to assume the sclerosant into the involved vessels with an appropriate depth—not to blanch the mucosa, and not deep enough to injure the underlying muscle. We compressed the injection position 30-60 seconds using the front of colonoscopy to achieve hemostasis. After treatment, the patients continued to be observed for 1 or 2 h to detect the early complications (such as bleeding and pain). The patients were recommended to use a high-fiber diet, stool softener (Duphalac 15ml tid * 3 days). In addition, the patients were required to pay more attention to anal health and excessive straining during defecation. The post-banding symptoms were recorded, consisting of postoperative pain and postoperative bleeding. After 1 week to 24 months, patients were contacted by telephone for a follow-up to document results of the treatment. Re-examination of colonoscopy was recommended after 3 months and therapeutic effect was graded as cure, improvement, and failure (three grades).
This study was approval by the ethical committees of Guangzhou Medical University and performed according to the Declaration of Helsinki. After explanation of the associated risks and benefits and description of this study protocol, all patients were asked to provide written informed consent.
Statistical analysis
The statistical analysis of data was done by using SPSS 13.0. The description of data was done in form of mean ± SD for quantitative data; while frequency and proportion for qualitative data. The analysis of data was done to test the statistical significant difference between groups. Student’s t-test was used to compare between 2 groups for quantitative data, and X2 test was used for qualitative data. The statistical significance was determined at the level of 0.05.
A total of 110 patients (64 male and 46 female) with a mean age of 45.5 years (SD=10.8 years) were enrolled into this study. Among them 44% of patients (48/110) had the second-degree hemorrhoids and 56% of patients (62/110) had the was the third-degree hemorrhoids. According to Goligher’s (1976) classification, second-degree hemorrhoids could prolapse, but reduce spontaneously after defecation; third-degree hemorrhoids needed to be reduced manually. All of the patients suffered from hemorrhoids bleeding at different extend, which had continued to bleed at least once a week in 68 patients (62%) or daily in 42 patients (48%) Table 1. From our results show n in this study, we found that no patient had immediate complications. Mild postoperative pain occurred in 13 cases (12%) after the initial treatment, but could be alleviated spontaneously without pain medication. 26 patients (23.6%) showed self-limiting rectal bleeding one week after the treatment, and the blood loss was less than 5ml per day. All patients displayed pelvic infection, rectal prolapse and urinary retentions. Three months later, 95.5% of patients (105/110) were effectively treated. No anorectal stenosis, rectal tenesmus, pain and prolapses were observed in these patients.5 patients carried out another sclerotherapy with injection of Lauromacrogol due to recurrent hemorrhage. A total of 93 patients (85%) were contacted by telephone for a follow-up to document results of the treatment after 1 month, 6 months, 1 year and 2 years. Among them, 70 cases (75%) showed no symptoms. 23 cases (25%) had some residual symptoms including occasional bleeding and prolapse, however, there were no requirements for further treatment. No patient experienced fecal incontinence. The duration of the operation in our study is 16.3±5.1minutes, which indicates the treatment is fast and convenient. The total cost of this sclerotherapy with Lauromacrogol is 2536±167.8 Yuan so we regard it as an economical method.
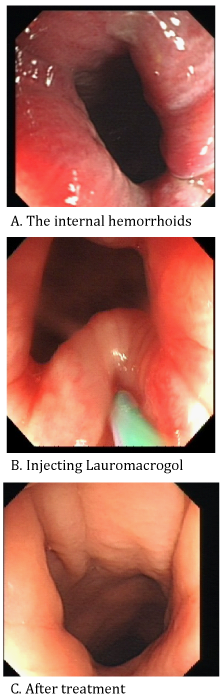
Figure 1 Video: colonoscopic sclerotherapy for bleeding internal hemorrhoids with lauromacrogol.
The procedure of the lauromacrogol sclerotherapy.
Variables |
Number (%) |
Age |
|
20-39 |
33(30) |
40-59 |
49(45) |
60-79 |
28(25) |
Gender |
|
Male |
65(58) |
Female |
46(42) |
Stage |
|
Second-degree |
48(44) |
Clinical presentation |
|
Bleeding at least once a week, but not every day but not every day |
68(62) |
Daily |
42(38) |
Table 1 Clinical data for patients
Hemorrhoidal disease is one of the most common anorectal diseases, dating back to antiquity. It has been stated that 50% of the population will experience symptomatic hemorrhoid disease at some point in their lives.12 The procedure for prolapse and hemorrhoids (PPH), proposed by Longo in 1998, uses a circular stapling device to divide, resect, and repair the mucosa and submucosa. It is regarded as the most effective approach for curing the hemorrhoids by surgeons. However, this surgical treatment needs hospitalization, being accompanied with postoperative pain and huge cost. Although surgery is superior to drug treatment in terms of complete cure, patients are frequently reluctant to undergo surgery.13 The main non-operative approaches to bleeding internal hemorrhoids include the rubber band ligation (RBL) and the sclerotherapy. The role of sclerotherapy in treatment of internal hemorrhoids is still in dispute. In a prospective study Khoury et al.14 demonstrated that 89.9% of patients with grades 1 and 2 hemorrhoids were helped, whereas a recent randomized, controlled trial demonstrated no advantage of sclerotherapy over bulk laxatives.15 In this study we showed that the Lauromacrogol sclerotherapy is effective. Contrary to some reports in the literature, sever complications, such as tissue necrosis, perforation and anal stricture did not occur in any patients in our study, which indicates that the Lauromacrogol sclerotherapy is safe. The cost of Lauromacrogol sclerotherapy is low, which is benefit to the patients. Conclusively, in terms of safety of use and results, the Lauromacrogol sclerotherapy is a feasible, easy, fast, and inexpensive outpatient procedure.
The main limitation of our study is its retrospective, single-center design and relatively small number of patients. We are currently preparing a larger, multicenter, prospective, randomized trial with the Lauromacrogol sclerotherapy.
None.
None
The authors declare that they have no competing financial interests.

©2014 Guo, et al. This is an open access article distributed under the terms of the, which permits unrestricted use, distribution, and build upon your work non-commercially.