eISSN: 2373-6372


Letter to Editor Volume 1 Issue 4
1Department of Gastroenterology and Hepatology, Rutgers New Jersey Medical School, USA
2Department of Internal Medicine, Rutgers New Jersey Medical School, USA
3Department of Radiology, Rutgers New Jersey Medical School, USA
Correspondence: Henry S Dinneen DO, Department of Internal Medicine, Rutgers New Jersey Medical School, 150 Bergen Street UH I-248, Newark, NJ 07103, USA, Tel 973-972-6056, Fax 973-972-6077
Received: September 09, 2014 | Published: October 25, 2014
Citation: Protopapas G, Henry S Dinneen DO, Al-Khalili R, Demyen M (2014) Superior Mesenteric Artery Syndrome Presenting With Concurrent Portal Vein Thrombosis. Gastroenterol Hepatol Open Access 1(4): 00020. DOI: 10.15406/ghoa.2014.01.00020
We present a case of a 63 year old male presenting with superior mesenteric artery syndrome and concurrent acute portal vein thrombosis.
Keywords: superior mesenteric artery syndrome, SMA syndrome, portal vein thrombosis, portal vein thrombus
SMA, superior mesenteric artery; PVT, portal vein thrombosis; SMV, superior mesenteric vein; EGD, esophagogastroduodenoscopy; CT, computed tomography
Superior mesenteric artery (SMA) syndrome is a rare form of upper intestinal obstruction caused by narrowing of the angle between the SMA and the aorta, resulting in compression of the third portion of the duodenum. Rapid weight loss has been implicated in the development of this syndrome. The typical symptoms of SMA syndrome include abdominal pain, nausea, vomiting, anorexia and postprandial fullness.1,2 Acute portal vein thrombosis (PVT) occurring in the setting of SMA syndrome has previously been described in a pediatric patient.3 We present a case of an adult male with SMA syndrome presenting with concurrent acute portal vein thrombosis.
A 62 year-old African American man presented with periumbilical abdominal pain, nausea and bilious, non-bloody vomiting for two days. One month prior to presentation he was evaluated for a four-month history of watery, non-mucoid diarrhea with associated 15 lb unintentional weight loss. This workup included stool studies, colonoscopy, and CT of the abdomen, all of which were normal. His medical history was notable for uncontrolled diabetes mellitus type II, seizure disorder, and untreated hepatitis C. On examination he was a cachectic male with a calculated BMI of 14.8. He was hemodynamically stable and afebrile, with a diffusely tender abdomen and voluntary guarding. There were no stigmata of liver disease. Laboratory studies revealed a leukocytosis of 15.9; however an extensive infectious work-up including blood, urine and peritoneal cultures was negative. Liver function tests, amylase, lipase, and lactate levels were all normal. A CT of the abdomen revealed narrowing of the distance between the SMA and the aorta at the level of the 3rd portion of the duodenum (Figure 1a), with associated dilation of the stomach and proximal duodenum. These findings were consistent with SMA syndrome. Also seen were non-occlusive thrombi in the branches of the portal vein consistent with acute PVT (Figure 1b). Finally, mild compression of the distal superior mesenteric vein (SMV) was appreciated on CT. An abdominal ultrasound revealed a decreased SMA-aortic angle of 16-24 degrees (Figure 2a) and a distance between the two measuring 6mm (Figure 2b), thereby confirming the diagnosis of SMA syndrome.4 Esophagogastroduodenoscopy (EGD) was subsequently performed, revealing a dilated stomach with large amounts of gastric contents. A decompressive gastrostomy tube with a feeding jejunal extension was placed. The patient was managed medically with anticoagulation and empiric antibiotics and demonstrated clinical improvement. He was subsequently discharged to a nursing facility following a 2 week hospitalization; the gastrojejunostomy tube was kept in place on discharge. The patient returned to the hospital 2 months later with urosepsis further complicated by diabetic ketoacidosis and uncontrolled seizures. The patient ultimately expired from these comorbid illnesses before follow-up imaging could be obtained.
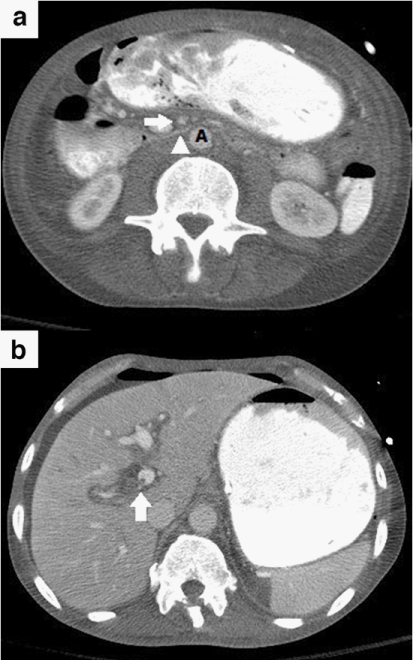
Figure 1 (a) Axial contrast CT image demonstrates narrowing of the distance between the superior mesenteric artery (arrow) and the aorta (A) at the level of the third portion of the duodenum (arrowhead). Also note the distention of the stomach and first and second portions of the duodenum proximal to the level of the crossing superior mesenteric artery.
(b) Axial Contrast CT image obtained during the portal venous phase demonstrates a non-occlusive thrombus within the right portal vein (arrow).
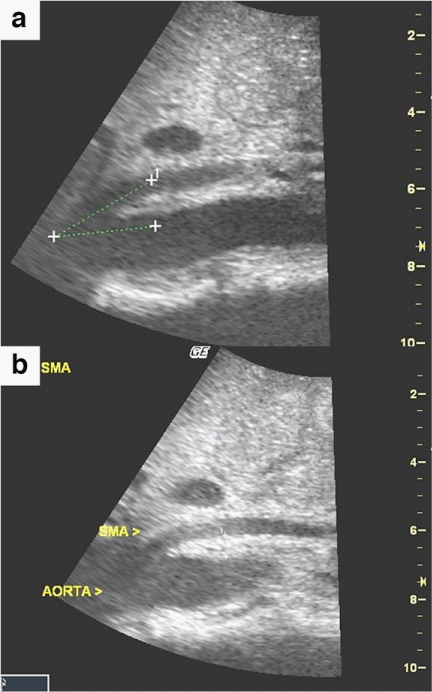
Figure 2(a) Sagittal ultrasound image of the abdomen demonstrates a decreased superior mesenteric artery-aortic angle of approximately 16-24 degrees.
(b) Sagittal Abdominal ultrasound image demonstrates a decreased distance between the aorta and the superior mesenteric artery of 6 mm.
This case highlights the relationship between the portal and systemic vasculature and surrounding bowel. There is a paucity of literature detailing the effects of SMA syndrome on the portal vasculature, with only one other reported case of SMA syndrome with concomitant portal vein thrombosis. A 10-year-old girl presented with SMA syndrome complicated by gastric wall pneumatosis, portal venous gas, and thrombosis. Increased intraluminal gas pressure with extension to the hepatic portal venous system was thought to have contributed to development of the PVT.3 Our patient presented with a markedly distended stomach and duodenum, and therefore a similar mechanism may have accounted for development of a PVT. A lack of gas appreciated in the portal system on CT, however, does not support this etiology. In prior case reports of malignancy and PVT, direct compression of the SMV by tumor mass with consequent venous stasis has been implicated in the development of PVT.5 In our case; local compression on the SMV by the distended proximal duodenum may have mimicked a similar pathophysiology.
Special attention should be paid to the pressure effects of a dilated proximal duodenum or dilated stomach on the adjacent abdominal vasculature. We should remain alert to the possible association of SMA syndrome and portal vein thrombosis.
None.
All authors have contributed to and agreed on the content of the manuscript, and the respective roles of each author. This manuscript has not been published previously, in any language, in whole or in part, and is not currently under consideration elsewhere for publication. The authors of this article have no financial relationships to disclose.

©2014 Protopapas, et al. This is an open access article distributed under the terms of the, which permits unrestricted use, distribution, and build upon your work non-commercially.