Advances in
eISSN: 2378-3168


Research Article Volume 9 Issue 2
EclaireMD Foundation, USA
Correspondence: Gerald C Hsu, 7 Oak Haven Way Woodside, CA 94062, EclaireMD Foundation, USA, Tel 1-510-331-5000
Received: October 04, 2018 | Published: March 11, 2019
Citation: Hsu GC. Understanding and predicting fasting plasma glucose to control type 2 diabetes (math-physical medicine). Adv Obes Weight Manag Control. 2019;9(2):30-38. DOI: 10.15406/aowmc.2019.09.00270
The author has type 2 diabetes (T2D) for 25 years and, during the past eight years, he collected approximately 1.5 million data of his lifestyle details and medical conditions. His approach is a “math-physical medicine” approach based on mathematics, physics, optical and electronics physics, engineering modeling, signal processing, computer science, big data analytics, statistics, machine learning, and artificial intelligence (AI). His main focus is on preventive medicine using prediction tools. He believes that the better the prediction, the more control you have over your chronic diseases.
The author’s research approach is based on his solid interdisciplinary academic background and successful industrial experiences. His 17 years of college education and 36 years of working experience have prepared him to perform 20,000 hours on T2D research during the past eight years.
He conducted his diabetes research by ensuing a thorough process as follows:
The step-by-step research method in chronological order on this specific subject is described as follows:
During 2010 to 2011, he studied six chronic diseases: obesity, diabetes, hypertension, hyperlipidemia, heart attack, and stroke. Concurrently, he developed a customized software to collect related data of both lifestyle management details and medical conditions. Thus far, using this computer program, he has collected 8,878 glucose data including 7,206 postprandial glucose (PPG) and 1,672 fasting plasma glucose (FPG) for the past 4.7 years from 1/1/2014 to 8/25/2018.
After studying these six medical conditions and how they affect metabolic disorders, he spent a year living in a desert city in 2014 and developed a mathematical governing equation of the human body’s metabolism. He used 10 categories and then added in “time” as the 11th category to get the “dynamic” effect of each variable’s behavior over time. Within the medical output categories, there are four medical conditions: weight, glucose, blood pressure, and lipids. Within lifestyle input categories: there are six lifestyle management details: food, exercise, water, sleep, stress, and life pattern regularity. He further identified a total of about 500 elements within these ten categories to define and describe his desired metabolism model, ending up with 14-pages of a long equation of the human metabolism model. At last, he created two new terms which use simple numbers or percentages to effectively describe his overall metabolism and health status at any time. These two new terms are Metabolism index (MI) and General health status unit (GHSU).
The metabolism curve is similar to the ocean waves by going up and down with various waveforms. Their building components and control methods are extremely different and complicated. You cannot analyze your metabolism based on your medical conditions alone since it only provides a partial picture. You must include detailed lifestyle data in order to get a total picture of your health. During the author’s research process, he has utilized advanced mathematics, statistics, physics, structural engineering modeling, certain powerful techniques from optical physics and electronic wave theory, and modern computer science algorithms and calculation tools. Mathematics includes partial differential equation, nonlinear algebra, topology concept, complex variables, and statistics. Structural engineering modeling includes finite element method to convert the human body’s “continuum” or “analog” system into a “digital” system in order to take advantage of modern computing power to handle its associated big data. Furthermore, the author applied what he learned from his engineering thesis work at MIT; the concept of “plastic” state of a material similar to a “non-reversible” diabetes condition of a chronic disease patient vs. “elastic” state of a material similar to a “reversible” common illness of a healthy person.
The author named his approach as “math-physical medicine” where medicine is the subject and math-physical is an adjective. In other words, his intention is to research on medical problems but utilizes mathematics, physics, and engineering as tools of research. The author has a master’s degree in the field of biomechanics. In his opinion, many schools offer “bio-engineering or medical engineering” curriculums with their emphasis on demonstrating engineering’s beauty and power (engineering or mechanics are subjects here) using medicine as an application domain, instead of truly solving medical problems (medicine is an adjective here).
During the period of 2015-2017, the author focused on developing five prediction tools - Weight, FPG, PPG, Adjusted Glucose, Estimated Hemoglobin A1C or known as A1C. In traditional western medicine, most of the emphasis is placed on treatment of existing medical conditions instead of prediction and prevention. From an engineering standpoint, having prediction tools and developing early-warning capabilities are extremely important to prevent negative outcomes. Similarly, by nature, these medical prediction tools would be extremely useful in preventive medicine as well. The better you can predict glucose behavior, the better chance you can reduce their damage on your internal organs, therefore, eliminating frustration, pain, expense, and risk down the road that are often associated with treatment of complications. This is especially true for chronic diseases since most of them are non-curable (i.e. non-reversible) in the foreseeable future; and therefore, the best and only hope of a patient relies on controlling these diseases and reduce risks from complications.
Weight
Weight control is critical for all people with chronic diseases and, as you may know, weight management is a difficult task for most people. The author took 3-years to bring his BMI down from 32.5 (220 lbs. or 100 kg) to 24.5 (167 lbs. or 76 kg) and 5-years to reduce his waistline from 46 inches (112 cm) to 32 inches (81 cm). He has monitored and analyzed his weight situation since 2012. He investigated the causes and rough percentages of weight loss at night due to: quantitatively measurable factors, such as urination and bowl movements, unmeasurable factors, such as vaporization and internal organ operations, as well as some special factors, such as sudden stress, sleep disturbance, illness, etc. During the past 3-years, both of his averaged weight gain during daytime and weight loss at night are ~2.8 lbs. (1.3 kg) per day. That is why he is able to maintain his body weight around 170 lbs. (77 kg) and BMI at 25. Based on all of these information, his weight computing model can predict his next morning’s weight and it has reached to 99.9% of linear accuracy.
FPG
During November 2015, the author noticed his FPG values increasing without any clear clues. In the following five months, he read more than 100 medical articles, conducted many experiments on his body, and performed numerous correlation analyses but failed to identify its major cause. In the early morning on March 17, 2016, he had a dream, resulting in out of box thinking. Up to that point, he approached the problem with a “traditional engineer’s thinking” which always looked for inter-relationships between output elements (e.g. glucose) and input elements (e.g. food and exercise, etc.). His dream inspired him to dig into relationships among the output elements. He then discovered the hidden high correlation coefficient of 86% between his weight and his FPG values based on data available at that time. After this discovery, he applied both time-series, spatial analyses, least square mean, and frequency domain techniques to derive a linear mathematical equation between weight and FPG (a skewed straight line with a slope of around 25-degree to 30-degree angle) and calculate the equation’s coverage area of data variance. Using his ~1,500 days data of FPG and Weight, his calculation revealed a 94% variance coverage from a +/-20% band. Because of this, his weight prediction serves a direct and most important role on his FPG prediction. In summary, Weight contributes about 80% to 85% influence on long-term FPG formation and the other four factors only contribute about 15% to 25%.
When sleeping, our body does not have many observable activities related to energy infusion and diffusion. The combined weight loss from sleeping from vaporization and urination and internal organ operations (energy diffusion), and weight gain at daytime from eating (energy infusion) minus exercising and internal organ operation (energy diffusion) determine our weight fluctuations. Weight is a mere physical representation of our body’s internal energy exchange. Thus, this weight changes lead directly into the wave fluctuations of both FPG and PPG. In short, FPG changes are the results of our body energy changes at nighttime with weight functioning as the physical representation of this internal energy exchange. He has analyzed this problem using my mechanical engineer’s training on “energy”.
After six months of research in 2017, he identified that other than weight (80-85%), weather related ambient temperature contributes approximately 10% to both FPG and PPG creation models. This is an example of maintaining harmony or achieving balance between the human body and environmental conditions. By now, the author realized that each human body has an existing biorhythm which is the natural outcome from million years of evolutionary improvement and continuous adaption of human body with the environment. We should respect this biomedical rhythm and environmental harmony and try our best not to interrupt, intrude, or destroy it. In his opinion, chronic diseases are created from these “imbalance of our biorhythm”. 1–4
Adjusted Glucose & Hemoglobin A1C
The author created a new term of “adjusted glucose” with different weighting factors for contributions from FPG and PPG, respectively. In order to combine FPG and PPG into one unified daily glucose number and then to determine the predicted A1C level (i.e. mathematical A1C, not lab-tested A1C), the author examined many stages of glucose formation and variations. In order to get an accurate, effective, and practical predicted A1C values, this task cannot be done via a simple conversion factor as indicated in some published medical documents. As we know, even a lab-tested A1C result can be influenced by many factors, such as chemical, environmental, operational, etc. which may contribute to a margin of 15% to 30% build-in error. However, A1C value has been adopted by the medical community as the yardstick of diabetes diagnoses. Therefore, the author adopts the same standard to make sure that his predicted A1C result is as close as possible to the lab-tested A1C results.
He further borrowed one idea from his previous industrial experience in nuclear power plant design and earthquake engineering of having a “safety margin”. Since the intention of this algorithm is to provide an “early-warning” capability to diabetes patients, he designed his final A1C prediction tool to contain only 95% linear accuracy which is about 5% higher than lab-tested A1C results. He did this intentionally to add-in a minimum safety margin of 5%. In other words, his safety margin increases his predicted A1C value by at least 5% higher than lab-tested A1C value in order to “scare” the diabetes patient’s a bit and allow them to modify their lifestyle behavior before the actual lab-testing is conducted, without losing its desired accuracy.
The author spent three years (2015-2017) to develop five prediction models to achieve approximately 95% (for A1C) to 99% (for both FPG and PPG) of linear accuracy (Figure 1) with high correlations (pattern similarity) between two biomedical signal waves, predicted and measured glucose. The following sections cover point by point the information in Figures 1–7.
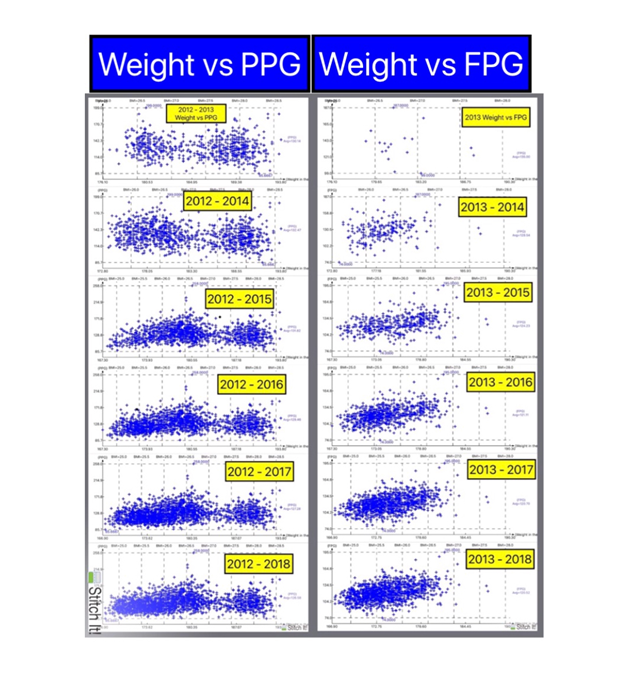
Figure 5 Constant PPG values, despite Weight changes FPG has a linear relationship with Weight (2012 – 2018).
Glucose measurement frequency and timing
Most type 2 diabetes (T2D) patients dislike finger-piercing measurements due to its associated inconvenience, pain, cost, and psychological reactions. In order to conduct his research, the author diligently measured his blood sugar four times a day during the past 6.5 years (more than 2,000 days), once in early morning for FPG and 2 hours after each meal (3 times a day) for PPG. He collected data since 1/1/2012 and recorded all of his measured data and associated lifestyle details into his customized software on his iPhone.
Total identified influential factors and their contributions on FPG
There are five factors for FPG identified and used in his research. Weight contributes about 80% to 85%, weather temperature about 10%, and all of the other three factors about 5% to 10%.
FPG impact by primary influential factors
Using machine learning technique and AI algorithm, his customized software can automatically calculate the conversion factor of FPG fluctuation in certain amount of mg/dL caused by each pound of weight change between two adjacent days.
FPG impact by weather temperature
For FPG, when weather is below 67 degrees Fahrenheit (19.4 degrees Celsius), FPG drops a certain amount of mg/dL by each degree of Fahrenheit decrease. But, when weather is above 77 degrees Fahrenheit (25 degrees Celsius), whether FPG will rise in certain amount of mg/dL by each degree of Fahrenheit increase still needs more investigation on extreme weather conditions. His customized AI software can automatically calculate these equations and obtain useful quantities for prediction and control.
Contribution of FPG on adjusted glucose (as well as on estimated A1C)
FPG: approximately 15% to 25%
PPG: approximately 75% to 85%
This ratio is constantly being self-learned and self-adjusted when a new lab-tested A1C value is entered into the software system. This is an example of “machine learning” application.
FPG data and waveform
Generally speaking, in comparison with PPG waves, FPG waves have longer period, lower frequency, and lower amplitude. Therefore, FPG wave has lower peak and shallower valley, i.e. the “vibration amplitude” is smaller. This is due to the fact that energy diffusion at night is less intensive in comparison with both energy infusion and diffusion of PPG at daytime. The leftover energy is utilized by the body at night. This phenomenon also creates an observation that weight does not fluctuate much from day to day. Above-mentioned characters can be easily analyzed, interpreted, and understood via wave theory from physics and signal processing techniques from engineering.
Correlation between glucose and weight
Investigating Weight and Glucose reveal that FPG is highly related to Weight, which is further related to food portion (total food “quantity”). On the other hand, PPG is highly related to carbs/sugar intake amount (nutrition contents or food “quality”), not related to Weight directly. Based on the author’s experience, by simply reducing his weight while he was obese (BMI>30), his overall diabetes conditions improved rapidly and significantly. However, while in his “overweight” stage (BMI between 25 and 30), it was more difficult for him to lose weight and the task becomes harder in terms of obtaining rapid and clear effectiveness of diabetes control. During this stage, the above-mentioned knowledge of both FPG and PPG greatly helped him to effectively control his T2D conditions. In conclusion, the more you know about the differences between fasting and postprandial glucoses, the easier and more effective job you can do in terms of diabetes control via this “divide and conquer” approach to face these two different glucose challenges.
Correlation between FPG and PPG
The correlation coefficient between FPG and PPG is below 20% which means there are no direct links between these two glucose values.
Relationship between FPG and blood pressure (BP)
No obvious and significant correlation existing between FPG and BP.
Techniques used to build FPG prediction model
The FPG prediction model utilized mathematics equations, three statistical methods including time-series, spatial analysis, and frequency domain analysis, and modern computational tools, such as database, parallel processing, big data analytics, machine learning, and AI.
Linear accuracy and correlation coefficients between predicted and measured FPG
By mid-2018, predicted FPG vs. measured FPG have achieved 99.9% of linear accuracy and 97.4% correlation coefficient. I
Finally, Figure 1 through Figure 6 further illustrate the contents described in this article and displayed on Figure 7.
Figure 1 depicts accuracy and correlation (R) of FPG, PPG, & A1C between predicted and measured values. FPG has 99.9% of accuracy and 97% of R, PPG has 99.9% of accuracy and 84% of R with some phase shift situations, A1C has ~95% accuracy due to build-in 5% safety margin during the period of 6/1/2015 to 8/29/2018. Figure 2 shows pie charts of element contribution percentages of Weight, FPG, PPG, and A1C. Figure 3 displays the relationship between FPG and Weight using both time-series analysis and spatial analysis. Figure 4 demonstrates an extremely low correlation (7%) existed between FPG and PPG, as well as a low correlation (19%) existed between PPG and weight. Figure 5 depicts a formation of annually accumulated “cluster data clouds” for both FPG and PPG. Although PPG has a constant value no matter what weight changes, FPG has a linear relationship with a skewed angle with weight changes. In other words, FPG increases its value when weight jumps. Figure 6 shows the screen of an AI Glucometer which is a medical product that brings theoretical research results to practical disease control. Diabetes patients do not have to suffer from daily finger-piercing or laboratory blood-drawing test. This AI tool can help these patients to predict their glucose values; therefore, they can control their T2D conditions using math-physical medicine research results.
After 2015, the author’s severe T2D condition is completely under control using his developed “math-physical medicine” approach, including metabolism model (MI and GHSU), and five glucose prediction tools. The author has acquired extensive knowledge and useful experience from his own 8-years and 20,000 hours of self-study and research. He also wants to share his knowledge and experience with other T2D patients through medical professionals. He firmly believes that a deeper understanding, quantitative knowledge, and precise pictures of both FPG and PPG will also benefit worldwide healthcare professionals with their tasks of effectively controlling diabetes.
Limitation of research
This article is based on data of metabolic conditions and lifestyle details collected from one T2D patient (himself). It does not cover genetic conditions and lifestyle details of other diabetes patients. Therefore, his conclusions and findings should be re-verified and used with caution when being applied to other patients who are under different metabolic conditions or lifestyles.
Other declarations
During the past 8 years of self-study and research, the author has never hired any research assistant or medical research associate to help with his work. He applied his own invention of a “Software Robot” created during 2001-2009, his AI knowledge, and his previous programming experience (close to 1 million lines) to produce the system architecture, design structure, and some special code of this customized computer software. He used this software to collect and analyze his big data, conduct his medical research, and to control his diabetes disease.
This project was 100% self-funded by using his own money that was earned from a successful high-tech venture in Silicon Valley. He did not receive any financial assistance or grants from any public, private institution or organization. Therefore, there are no concerns regarding any conflict of interest.
First and foremost, the author wishes to express his sincere appreciation to a very important person in his life, Professor Norman Jones at MIT and the University of Liverpool. Not only did he give the author the opportunity to study for his PhD at MIT, but Professor Jones also trained him extensively on how to solve difficult problems and conduct basic scientific research with a big vision, pure heart, integrity, and dedication.
The author would also like to thank Professor James Andrews at the University of Iowa. He helped and supported him tremendously when he first came to the United States. His encouragement assisted the author to build his solid engineering and computer science foundation. He is forever grateful to his earlier mentor, who has a kind heart and guided him during the struggles of his undergraduate and master’s degree work at Iowa.
Finally, but not least, he would like to extend his appreciation to two medical doctors associated with Stanford University and its medical clinics at different periods. Dr. Jamie Nuwer provided him with encouragement on his continuous diabetes research work. Dr. Jeffrey Guardino advised him to write up his research findings to share with other patients and medical professionals.
The author declares there are no conflicts of interest.

©2019 Hsu. This is an open access article distributed under the terms of the, which permits unrestricted use, distribution, and build upon your work non-commercially.