Advances in
eISSN: 2378-3168


Review Article Volume 9 Issue 3
1Florida International University, USA
2 REDI LLC, USA
Correspondence: Maria Jose Míguez, Florida International University, School of Integrated Science and Humanity,11200 SW 8th St. Suite AHC4-355, Miami, FL 33199, USA
Received: April 13, 2019 | Published: May 9, 2019
Citation: Miguez MJ, Gray C, Stanton C, et al. Mentholated cigarettes or weight problems, which came first. Adv Obes Weight Manag Control. 2019;9(3):59-64. DOI: 10.15406/aowmc.2019.09.00275
Background: Despite the old myth that smokers are skinnier, obesity is reaching epidemic proportions among smokers living with HIV, and particularly among women. We have previously observed an association between the use of mentholated cigarettes and obesity, but it is unclear whether obesity was a result from menthol induced-alterations, or if weight problems were a pre-existing condition.
Methods: Smokers living with HIV and ready to quit were consecutively enrolled in our clinical trial. With a response rate of 98%, 154 female smokers were enrolled until 12/2018. Smoking history was obtained and participants were grouped into users of mentholated cigarettes=Group 1, or Group 2 if non-mentholated users. The study visit includes collection of anthropometrics, along with a history of weight problems. Two main outcomes were examined: (1) the relationship between Body Mass Index (BMI) and proximal predictor variables derived from the Socio-Ecological Model: socioeconomic status, and unhealthy habits (dietary intakes, physical activities, sleep and smoking); and (2) the prevalence of overweight and obesity (BMI >30) and the history of obesity as a function of the type of cigarette used.
Result: The prevalence of obesity among this group was 51%, whereas in the general population is 38.3% (NHANES). An association was found between obesity and one SES component, race/ethnicity. Two behavioral factors were significant: high consumption of sugars and use of mentholated cigarettes. The age of smoking onset did not differ between groups 1 and 2, suggesting that smoking onset was not triggered by their weight concerns. Weight gain associated with pregnancies tended to affect the development of obesity in women during midlife and beyond (OR=2.1 95% CI 0.7-7.1, p=0.07). However, the history of obesity did not differ between Groups 1 and 2. Binary regression confirmed in the adjusted model the effects of history of obesity during childbearing years, use of mentholated cigarettes, and limited physical activity on current obesity trends.
Conclusion: Data points to the primacy of behavioral factors, such as the use of mentholated cigarettes. Analyses confirmed that obesity was not a precondition linked to start smoking, indicating that it is likely to be the consequence of using mentholated cigarettes. Reduced physical activity also is contributing to the rising obesity rates.
Obesity, defined as a body mass index (BMI ≥30), has reached epidemic proportions in the United States and it is one of the nation’s leading public health challenges. Obesity rates for males and females in the U.S. had been similar, however,1–3 more recently just over 40 percent of women are obese, compared to 35 percent of men. These rates are of high concern when compared to the 15 percent of women worldwide. Aggressive tobacco industry advertising have resulted in over 20 million female smokers in the United States.4 For years, the tobacco industry has exploited the belief that smoking is helpful in controlling weight, to influence commencement and continuation of smoking.1-3 Adults do not only use smoking as a method for weight control; adolescents who have dieted or are constantly concerned with weight are also more likely to start smoking.5–7 Notably, these observations were gender and specific, significant among females, but not among males.5–7
A recent epidemiological analysis pointed to another vulnerable population.7 Thompson and colleagues found a 42% point prevalence rate of obesity among females PLWHA (n=4,217). Clearly higher than the 36% rate among the general population (derived from the National Health and Nutrition Examination Study).7 In contrast, the respective male rates were 18.8% and 34.7%.7 Thus, the field of HIV and obesity research would benefit from more information to understand gender disparities. The additional knowledge may also aid health professionals for counseling these women. It can also facilitate developing novel pharmacological and behavioral interventions.
The Institute of Medicine recommends the use of Social Ecological Model (SEM) to study the obesity epidemic.8 The SEM posits concentric layers of personal, community, organization, government, industry and societal domains influencing obesity. Although the rising rates have been attributed to obesogenic conditions (e.g., inexpensive and often nutrient-poor food, or less favorable living environments), not all living on these settings are obese. Therefore, individual factors are playing a dominant role. Beyond dietary intakes, growing evidence suggests that physical activity and sleep alterations (time and quality) are risk factors for the development of obesity. Indeed, global surveillance has demonstrated that physical activity, although varied between countries, predicts obesity. They also discovered that reduced activity among women contributes to the observed inequalities on obesity. We have beforehand found that use of mentholated cigarettes, which is preferred by women, is another behavioral factor associated with obesity.9 Yet, it is possible that females with a history of being overweight are more likely to start smoking to control weight, compared to those without such antecedents. To date, most studies focusing on factors associated with body weight have been crosssectional;yet a longitudinal study designed should be preferred. Equally important to understand the increasing trends of obesity, is to study factors associated with body weight development. Our study aims to address this gap by examining if overweight adults have a prior history of obesity, and if the results vary according to the type of cigarette. Understanding how these factors are associated with weight may help to determine the cumulative health risk that current smokers may have as a function of the type of cigarette used.10
Design and setting
The Patch Study is an ongoing, randomized clinical trial involving HIV+ smokers who were motivated to quit. The trial has been ongoing since 2016, and is taking place in Miami, Florida. The aim is to recruit a total of 500 participants. The trial was powered to detect differences in biochemically verified 7-day point prevalence abstinence at 3, 6, and 12-months of follow-up (80% power, type I error rate of α= 5%, assuming a 20% loss to follow-up).
Current analyses spanned from June 2016 to December 2017, for a total of 18 months of enrollment and follow-up.
Adults were eligible if HIV status, smoking status, and willingness to quit were confirmed. For safety reasons, subjects were excluded if they had any contraindication to nicotine patches or gums, were involved in other smoking and/or drug cessation or weight control programs, or had comorbid conditions that limited their safe participation, such as the presence of psychotic or disabling psychiatric disorders. Written study materials, informed consent forms, and the study protocol were approved by Western IRB (WIRB). All procedures occurred at the University of Miami’s Clinical Translational Research Site.
Smoking surveys
After giving informed consent, participants provided an exhaled breath carbon monoxide sample (Vitalograph; Lenexa, KS) for biochemical verification of smoking status. Then, subjects completed several standardized surveys to profile smoking history, including the number of cigarettes smoked per day and the history of tobacco use (cigarettes vs. cigars). This data, along with age of initiation and the total number of years smoking, enabled estimation of cumulative exposure. To measure dependence we selected the Fagerström Test for Nicotine Dependence (FTND), due to its validity, reliability, and availability in English and Spanish.10 Participants were also asked about exposure to second-hand smoke (SHS), symptoms of lung disease, and personal/family history of respiratory conditions. Upon completion of the baseline visit, participants’ expired breath carbon monoxide samples were collected for verifying purposes.
Use of menthol-flavored cigarettes
This variable was based on self-reports (yes/no). It was also reconfirmed with the participant’s preferred brand conveyed to us. The Universal Product Code (UPC) on the cigarette packages were used to determine the type of cigarette and the concentrations of nicotine, TAR, CO, and menthol. Based on these parameters, smokers were dichotomized as menthol users or non-menthol users. Users of both type of cigarettes were not included in the analyses.
Anthropometric Measurements
Participants’ anthropometric measures were obtained at each visit. Body weight and height were measured to the nearest 0.1kg, after removal of shoes and outerwear, using a calibrated balance. Weight and height were used to calculate body mass index (BMI; weight [lbs]/height [inches]2×703). Participants were classified as thin, if BMI was less than 18.5kg/m2, eutrophic if BMI was 18.5 to 24.9kg/m2, overweight if BMI was 25 to 29.9kg/m2, and obese if BMI was 30kg/m2 or higher.11–13 Studies suggest that waist to hip ratio (WHR) is more accurate than BMI for predicting the risks of cardiovascular disease and premature death, so we obtained those measures.12 As per national guidelines, the waist circumference was measured at the top of the iliac crest after fasting overnight.13 The hip circumference measurement was obtained around the widest portion of the buttocks. Following national guidelines, abdominal obesity was defined as a waist circumference greater than 102 centimeters (40 inches) in males, and 88 centimeters (35 inches) in females.14–16
Past history of weight problems and dieting
Finally, participants were inquired regarding a history of obesity and dieting. History of obesity was obtained using the following age brackets: 0-11, 12-18, 19-39, and at post-partum.
Sleep and physical activity
The Stanford 7-day Physical Activity Recall Scale (PAR) estimates both work-related and non-work-related physical activity.17 For each day of the past week, participants report the approximate number of hours they slept, and spent in the moderate, hard, and arduous activity. The survey includes a wide range of activities, from household cleaning to exercising and playing sports, or practicing a musical instrument. We recorded dietary intakes (24-hour food recall)18 and used the ESHA software food processor to determine intakes.
Covariates
We also investigated other risks and protective factors associated with obesity. Using computerized questionnaires, we recorded dietary intakes (24-hour food recall),18 socio-demographics, and the medical history including use of ART. Based on self-reports, subjects were categorized as African American, White non-Hispanic (Caucasian), or Hispanic. Age was stratified by 20-year gaps between groups (18 to 39, 40 to 59, or 60 and more years). Annual income was categorized as $0 to $11,000, $11,001 to $20,000, $20,001 to $49,999, or more than $50,000. Education level was assigned a code between 1 and 16, representing each year of schooling from elementary/middle school through college or vocational training. Participants were questioned regarding alcohol intake in the past six months, using two standardized and validated brief screening questionnaires: The Alcohol Use Disorders Identification Test (AUDIT),19 and the Alcohol Dependence Scale (ADS).20
Beyond sociodemographics we examined HIV associated clinical factors. T cell counts were quantified using Flow cytometry (percentage and absolute numbers of T lymphocyte subpopulations CD3+/CD4+ and CD3+/CD8). A good immunological response was defined as having more than 500 CD4+ cells. Viral load was determined at each visit using the ultrasensitive Amplicor HIV monitor test (Roche Diagnostic System).
Statistical analysis
All statistical analyses were conducted using SPSS 21.0 (SPSS Inc., Chicago, IL, USA). For all analyses, statistical significance was considered as a two-tailed p-value <0.05. Means, standard deviation and percentages were used to describe the characteristics of the study sample. Analysis of variance (ANOVA) was performed to test for significant differences in mean of anthropometric measurements and the variables of interest. Regression analyses were executed to evaluate predictors of body mass index, and any factors that were significantly associated with BMI were included in the final model.
A total of 341 participants have been randomized in our clinical trial; of them, 167 were female smokers and were eligible to be included for these analyses. The mean CD4 count for the group was 659 cells/μL. More than half (60%) had undetectable viral loads, with 90% having less than 1000 copies. Demographics and smoking behaviors were assessed at baseline. Reflecting the current trend of the HIV epidemic, the mean age was above 50 years in both groups (23-69 years old). Females were mostly of low and middle-class income. This distribution is in line with prior reports indicating that smoking rates are higher for persons living below the poverty line.21
In contrast to the popular perception that smokers are thinner, overall BMI scores were 28.8±8.8, highlighting the profile of this at-risk population. Overall, the prevalence of obesity among this group of females was 51%, and of overweight was 19%. Only a third of the group was eutrophic, and the remaining females were either overweight or obese (35%). Middle-aged subjects were more likely to be overweight than their younger counterparts (18-39 y OR:2, p=0.03). Sociodemographic characteristics are summarized in Table 1. Studies have observed that obesity prevalence varied by sociodemographics. Groups were very similar in educational level and income, yet the weight patterns were dissimilar among race/ethnic groups. Compared to the obese and the overweight groups, a higher proportion of eutrophic individuals were Caucasians. On the other hand, Hispanics were either overweight or obese. Near a third of the African Americans had an ideal BMI (18-25).
Mentholated versus non-mentholated
First, we confirmed that there were no significant sociodemographic or clinical differences between users of mentholated and non-mentholated cigarettes. As shown in Table 2, both groups had a similar smoking profile. However, a higher proportion of users of mentholated cigarettes reported annual incomes below $10,000.
Does smoking affect body mass index/ weight?
To better understand how smoking and body weight relate, it is crucial to account for the type of cigarette being used. Despite similar amounts of smoking, and exercise patterns, PLWH who smoked menthol-flavored cigarettes had significantly higher BMI values than non-menthol smokers (29.2±7.8 vs. 25.2±4.4, p=.02). As depicted in Table 3, additional analyses indicated differences in several anthropometric measures.
Association between childhood and childbearing weight status and adult obesity
Since prior studies have shown the association between adolescent and childbirth weight problems with obesity in adults later on, we explored such an association. Figure 1 shows the proportion of females that reported being obese in childhood, adolescence, or adulthood, if they were obese or not now.
Females that are obese now were five times more likely (95% CI 1.2-34, p=0.01) of having a history of obesity during adolescence (12-18 years). They were six times more likely to have been overweight, and 14 times more likely to have obesity during the 19 to the 39-age bracket. However, there were no differences in the history of obesity between users of mentholated cigarettes and those of non-mentholated ones. During adolescence the risk was inverse (OR=0.7 95% CI 0.19-3.4, p=0.42) and the risk of obesity in the childbearing years was 1.1 for menthol users (95% CI 0.2-7.9, p=0.4).
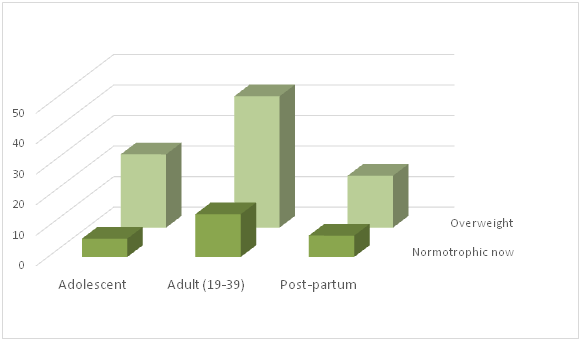
Figure 1 shows the proportion of females that reported being obese in childhood, adolescence, or adulthood, if they were obese or not.
|
Predictors |
Obese |
Overweight |
Eutrophic |
p-value |
|
Age |
49.5±8.8 |
50.7±8.0 |
50.8±9.1 |
0.6 |
|
Race/ethnicity Caucasian African American Caribbean Hispanic |
3.8 % 84.6 % 1.3 % 10.3 % |
3.4 % 86.2 % 0 % 7 % |
17.8 % 82.2 % 0 % 0 % |
.01
|
|
Income < $10K $10 - $29K $30-79K |
83 % 15 % 2 % |
83% 14 % 3 % |
76 % 18 % 6 % |
.35 |
|
Education |
5.9±2.3 |
5.6±2.1 |
5.4±2.2 |
.34 |
|
Age Start Smoking |
17.9±7.8 |
16.3±3.6 |
18.3±7.9 |
.50 |
|
Years Smoking |
30.9±10.6 |
31.5±11.6 |
31.8±9.5 |
.58 |
|
CD4 |
697.3±470 |
603.1±428 |
628.2±460 |
.56 |
|
Viral Load undetectable |
40% |
32% |
50% |
.32 |
Table 1 Group Characteristics by BMI
|
Predictors |
Mentholated N=145 |
Not mentholated N=22 |
p-value |
|
Age |
51.2±8.8 |
51.9±8.7 |
0.6 |
|
Income < $10K |
80% |
61% |
0.02 |
|
$10 - $29K |
17% |
32% |
|
|
$30-79K |
3% |
7% |
|
|
Education |
5.7±2.1 |
5.6±1.9 |
0.68 |
|
Baseline Fagerstrom |
5.3±1.96 |
5.4±2.0 |
0.94 |
|
Body Mass Index |
28.89±7.59 |
26.55±5.32 |
0.94 |
|
Years Smoking |
30.91 ±11.6 |
31.87±9.57 |
0.58 |
|
CD4 cell count/ml |
661.3 ±460 |
642.7±472 |
0.87 |
|
Viral load undetectable |
41% |
44% |
0.48 |
|
Viral load detectable |
59% |
56% |
Table 2 Sociodemographics by type of cigarette use
|
Mentholated cigarettes |
Non-Menthol |
P value |
|
|
Waist |
38.15±7.4 |
36.36 ± 5.3 |
0.05 |
|
Hip |
41.59±6.2 |
39.69± 4.36 |
0.06 |
|
Triceps |
18.9±11.3 |
16.39 ± 8.6 |
0.11 |
|
Abdomen |
38.90±19.0 |
32.2±15.38 |
0.03 |
Table 3 Anthropometrics by Type of Cigarette
|
|
B |
Wald |
Significance |
Exp (B) |
|
Menthol (yes/no) |
1.947 |
5.093 |
0.024 |
7.008 |
|
Obesity Childhood |
18.649 |
0 |
0.998 |
1.25 |
|
Obesity Adolescence |
0.037 |
0.001 |
0.981 |
1.03 |
|
Obesity & Dieting (19-39) |
3.888 |
7.416 |
0.006 |
48.8 |
|
Obesity & Dieting middle age |
4.028 |
2.488 |
0 |
56.1 |
|
Exercise |
-1.29 |
5.808 |
0.016 |
0.275 |
Table 4 Final Regression Analyses
Note: Regression model was adjusted for covariates such as sociodemographics and clinical parameters. Since they were not significant.
Physical activity and smoking
National Guidelines recommend at least 2½ hours of moderate-intensity exercise weekly; however, only 40% of these females met these recommendations. Furthermore, physical activity was lower among smokers of mentholated cigarettes (1.2±0.43 vs. 1.6±0.51, p=0.008). Subjects reporting the recommended hours of physical activity did not differ from the less active in any sociodemographic parameter. However, clinically they had less viral burdens (314.8±225.8 vs. 4736.4±1532.8 p<0.05). An examination of survey records shows differences in physical activity but not in the overall number of calories consumed or the number of hours of sleep.
Final analysis
For the final analyses, the model was adjusted for sociodemographics and clinical parameters such as CD4, viral load, and antiretroviral treatment. In Table 4, multivariate regression analysis confirmed that the type of cigarettes smoked significantly predicted BMI. In the adjusted model, past history of obesity in early adulthood was also a significant predictor of obesity. Only age was significant among all the sociodemographic variables.
The analyses uncovered several interesting findings. Although most people presume that smokers are skinnier, over two-thirds of our participants were either overweight or obese. This finding is in line with many researchers describing a direct relationship between smoking and weight gain.22,23 In this regard, our cohort of female smokers living with HIV had a sizable proportion of obese and overweight participants. The hypothesis that smoking mentholated cigarettes adversely affects weight was confirmed, as smokers of mentholated cigarettes were significantly heavier than non-menthol smokers with HIV. We also use the well-validated Bradford Hill criteria. Hill outlined a systematic approach for using scientific judgment to infer causation from statistical associations observed in epidemiologic data, and include checking for: (a) Dose-Response, (b) Pathways and Coherence, (c) Consistency on Replication and Strength of Association and (d) mechanisms. Although our analyses do not permit24 to assess a dose-response; we are confident because there are clear pathways explaining our data. In addition, some large and well-designed studies have replicated our observations.25–26 With regards to potential mechanisms of action, we previously discovered differences in brain derived neurotrophic factor in users of mentholated cigarettes. BDNF is a regulator of human appetite and metabolism, key regulators of weight control.27 Antonio and colleagues also proposed that menthol users had altered food perception of fat and sweetness leading to overconsumption.26 Results are of concern because both obesity and smoking rates are skyrocketing among PLWHIV. Moreover, they both are significant contributors to morbidity and mortality.28–32
However, this time we are also providing compelling evidence that overweight/obesity is not a significant pre-condition before starting smoking in this group. To our knowledge, this is the first study of this kind. Identifying the women’s age at which weight gain starts, known as adiposity rebound, is critical from a public health perspective. Since cohort studies28 found that weight problems during adolescence were reasonable predictors of adulthood obesity, we explored this relationship. While we initially uncovered a similar result, in the final model it was no longer significant. Instead, our final model suggests that the childbearing years (early and middle adulthood), better forecast the weight problems of these women in later life. This finding highlights the importance of gender-specific studies and the need to design sustainable interventions to optimize female weight during these critical years. It also points to the possibility that hormonal effects may be one of the underlying mechanisms of action. As African Americans prefer mentholated cigarettes, it will be relevant to determine their role on the weight increments observed on Black women compared to other groups. Another potential mechanism, found in our study as well as in population studies,29 is reduced physical activity. These findings need to be analyzed considering some limitations. First, the data derived only from people living with HIV, yet studies from the general population have reached similar conclusions. Second, while our study is longitudinal, the life history of weight problems was based on women’s self-reports, and thus are subject to recall bias. Overall, the data support the existence of a close association between mentholated cigarettes and obesity. These findings highlight the need for more longitudinal studies and a closer examination of mentholated products. More work is also needed to identify the biological mechanisms involved.33
None.
The authors declared there is no conflict of interest.

©2019 Miguez, et al. This is an open access article distributed under the terms of the, which permits unrestricted use, distribution, and build upon your work non-commercially.