eISSN: 2379-6367


Research Article Volume 6 Issue 3
Neuroscience Institute, Greece
Correspondence: Alen J Salerian, Neuroscience Institute, Zaimi Street 8, 2nd floor, Paleo Faliro, Athens, Greece, Tel 30-689-372-3947
Received: April 06, 2018 | Published: June 21, 2018
Citation: Salerian AJ. The heroin epidemic (2000-2014): manmade influences. Pharm Pharmacol Int J. 2018;6(3):246-251. DOI: 10.15406/ppij.2018.06.00182
Introduction: The United States has been experiencing an epidemic of heroin addiction and deaths. From 2000 to 2014 deaths from heroine rose from 0.7 to 3.4 per 100.000 populations. There were 10.574 heroin overdose deaths in 2014.
Method: Vital statistics were reviewed from 2000 to 2014. We also reviewed the psychiatric literature on heroin addiction through Medline and Google scholar by using the key words, heroin addiction, heroin epidemic, substance abuse, substance and action, etiology of heroin addiction.
Results: From 2000 to 2014 deaths from heroine rose from 0.7 to 3.4 per 100.000 populations. There were 10.574 heroin overdose deaths in 2014. Total overdose deaths rose from 6.2 to14.7 per 100.000 populations from 2000 to 2014. The percentage of deaths associated with prescription opiates declined from 38.1% to 28% while the percentage of heroin deaths jumped from 11% to 28 % during the same period. Illegally manufactured fentanyl and heroin were involved in more than half of the drug overdose deaths of 9 deaths per 100.000 populations in 2014 there are 110 million Americans with chronic pain. Various man made barriers compromising delivery of optimal compassionate patient friendly care seems to be prevalent and include medically unjustified access to endorphin agonists.
Discussion: The evidence suggests endorphin agonists (opiates) are crucial to effectively treatment refractory depression, chronic pain and heroin addiction. It seems likely that less than optimal and or the inefficient delivery of prescription opiates might have been a crucial catalyst- consistent with “Lorenz chaos theory and the butterfly effect “-triggering the US heroin epidemic.
Conclusion: Man-made interventions which resulted in reduction of access to treatment with opiates-might have contributed to the US heroin epidemic.
The United States has been experiencing an epidemic of heroin addiction and deaths. From 2000 to 2014 deaths from heroine rose from 0.7 to 3.4 per 100.000 population.1 There were 10.574 heroin overdose deaths in 2014(1). How did the heroine epidemic develop? What have been the major influences? Does it have man-made causes and solutions? On November 4, 2015 DEA acting administrator Chuck Rosenberg stated: We now know that overdoses from prescription opioid pain relievers are a driving factor in the 15-year increase in opioid overdose deaths. Since 1999, the amount of prescription opioids sold in the U.S. nearly quadrupled, yet there has not been an overall change in the amount of pain that Americans report. Guns are safer than prescription drugs. In 2013 more people died from a drug overdose than guns.2 The aim of this review is to investigate the possible underlying causes of the epidemic of heroin deaths from 2000 to 2014 including the alleged role of overproduction of prescription opiates. It seems also possible that Illegal production of illicit heroin and fentanyl and or increased demand for illicit heroin driven by inadequate supply for easy access to prescription opiates might have been crucial catalysts for the heroin epidemic.
Vital statistics were reviewed from 2000 to 2014. We also reviewed the psychiatric literature on heroin addiction through Medline and Google scholar by using the key words, heroin addiction, heroin epidemic, substance abuse, substance and action, etiology of heroin addiction.
Vital statistics
From 2000 to 2014 deaths from heroine rose from 0.7 to 3.4 per 100.000 populations.1 There were 10.574 heroin overdose deaths in 2014.1 The percentage of deaths associated with prescription opiates declined from 38.1% to 28% while the percentage of heroin deaths jumped from 11% to 28% from 2000 to 2014. Total overdose deaths rose from 6.2 to 14.7 per 100.000 population from 2000 to 2014 (Table 1). Deaths associated with heroin rose from 0.7 to 3.4 and from prescription opiates from 2.3 to 4.3 per 100.000 population from 2000 to 2014 (Table 1) (Figure 1) (Figure 2).1 The US annual suicide rates jumped from 10.2 to 13 per 100.000 from 2000 to 2014 (Table 1). From 2000 to 2014 the annual suicide rates in Japan (Figure 3) and the European union declined.2 CDC vital statistics suggest illegally manufactured fentanyl and heroin were involved in more than half of the drug overdose deaths of 9 deaths per 100.000 population in 2014 (Table 1). There are some 110 million people with chronic pain.3
Overdose |
6.2 |
14.7 |
Suicide |
10.1 |
12.9 |
Prescription opiates |
2.3 |
4.3 |
Medications (non opiates) |
3.2 |
5.7 |
Heroin |
0.7 |
3.4 |
PO/OD % |
38.1 |
28 |
Heroin/OD % |
11 |
28 |
Table 1 US Deaths (2000 vs 2014) Per 100.000 Population
CDC vital statistics reported 9 deaths per 100.000 populations for opioid overdose deaths in 2014; of those 3.4 were from heroin and 1.8 from synthetic opioids (fentanyl and tramadol) which nearly doubled in one year consistent with the police reports of dramatically increased illicit fentanyl manufacturing. Thus the actual overdose deaths from prescription opioids were 4.3 per 100.000 populations in 2014. (4.3 may be an overestimation because 19% of drug overdose deaths did not include any information on the death certificate about the specific types of drugs involved).
Source CDC: Vital statistics.
Heroin addiction
Heroin addiction is a chronic disorder .It presents with by drug intoxication, craving, bingeing, withdrawal and behavior often associated with prevention of withdrawal.4 Often, this cycle culminates in an intense preoccupation with the attainment of heroin to prevent withdrawal associated symptoms.4 Animal studies have shown marked differences in chronic consumption of heroin versus cocaine.5 The attainment of prevention of or relief from withdrawal symptoms seem to be the predominant influence for chronic heroin use in mice versus seeking reward and euphoria for chronic cocaine use.5 Opiates and their receptors are crucial in pain control ,pleasure and addictive behavior.4,6 The opiate receptors(mu, delta, kappa) have a high affinity for opiates.4,6 Endorphins, enkephalines and dynorphins (morphine like substances) are produced by brain. By opening potassium and calcium channels, opiates enjoy an inhibitory influence in the central nervous system.4,6 Opiates induce acute analgesia and euphoria. Analgesia is due to opiates acting as agonists at opiate receptor subtypes primarily in the sub cortical and limbic regions. Prefrontal cortex dopaminergic activation is associated with euphoric effects.4,6
Animals learn to regulate with some accuracy the amount of morphine they require.5 The observation that the increase in self administration is not infinite and correspondence to a specific pattern. The animal self administers morphine just the amount to prevent discomfort associated with withdrawal symptoms.5 Bioengineered mice that had become dependent on a morphine like substance would still benefit from the analgesic effect without any withdrawal symptoms upon discontinuation of opiates.7 Also there is a big difference between heroin and cocaine self administration8 Rats self administering cocaine lose up to 47% of the pretesting body weight and showed profound deterioration in general health. Animals self administering heroin maintained grooming behavior pre-testing body weight and a good state of general health. After stopping regular intake of opiates morphine abstinence syndrome develops.4 Symptoms emerge in the first 24 hours gradually resolving in 7 to 10 days. Increased anxiety, restlessness, irritability, dilated pupils, goose flesh, hot flashes, vomiting, diarrhea, fever, elevated blood pressure, increased heart rate and abdominal and generalized muscle cramps are common.
Increased noradrenergic parasympathetic and glutamatergic activity and the emergence of withdrawal symptoms correlate with plasma concentration half-life and the final clearance of a morphine like substance.4 The onset of withdrawal from an opiate does not always coincide with the onset of its terminal effects. A patient may be pain-free yet show withdrawal symptoms. Withdrawal is triggered by the downward shift of the plasma concentration of the endorphin agonist whereas the analgesic effect is determined by CNS effect. Addiction to opiates is primarily driven by behavior to prevent withdrawal discomfort rather than personal pleasure and reward.4,7 The reduction of unpleasant withdrawal associated symptoms. By Long acting heroin administered by intramuscular injection has been an effective treatment for opiate addiction.9 There is minimal risk of overuse of opiates with long elimination half lives (i.e. methadone and other extended release opiates). Various endorphin agonists with long elimination half-lives or slow release preparations (long-acting IM heroin, methadone and buprenorphine) ar the most effective therapeutic agents.4
Dopamine-Endorphin relationship
Dampening influence on sub cortical and limbic regions and activation of prefrontal cortex function represent the dual influence of endorphine agonists on brain function with.4,6 Executive function, mood and joy are enhanced by endorphins .Blocking endorphine agonists in prefrontal cortex neutralizes dopamine specific joy.10 Panic attacks and depression are caused by Naltrexone a morphine antagonist.11 Highly sophisticated intellectual and emotional functions are the domain of prefrontal cortex. A minute downward shift in prefrontal cortex function may adversely effect executive dysfunction, elicit anhedonia and diminished initiative. A recent discovery of antidepressant action is restoration of normal prefrotal cortex function.12,13 An impairment in spatial delayed alternation performance nearly as severe as that caused by surgical ablation is caused by depletion of dopamine in a circumscribed area of association cortex in rhesus monkeys can be pharmacologically reversed with dopamine agonists.14 This proves that dopamine plays an important role in a specific cortical function. The dorsolateral convexity of the prefrontal cortex plays a selective role in mediating mnnemonic, attentional and spatial capacities in primates including humans in prefrontal cortex serotonin activity is relatively low with high catecholamine levels (dopamine) in prefrontal cortex.14 These observations that suggests that dopamine in the prefrontal cortex may work as a neurotransmitter independent of its precursor role and the antidepressant effects of endorphin agonists.
Endorphins and antidepressant action
Preclinical essays showed that activation of the Delta opioid receptor produces robust antidepressant like effect.15 Electroconvulsive treatment of depressed patients is associated with elevations of plasma beta endorphin level and clinical improvement.16,17 Ten depressed patients improve by Cyclazocine a mixed opiate agonist antagonist.18 Ten patients with refractory depression who had previously failed to respond to traditional treatments had a positive response to buprenorphine.19 Three depressed patients unresponsive to electroconvulsive treatment had a robust response to buprenorphine and oxycodone.20 Antidepressant effects of methadone21 and buprenorphine22 have been shown. Also historically opiates have shown antidepressant and therapeutic benefits.23 Discontinuation of stable opiate treatment following practice closures have been associated with strikingly high suicide rates.24‒26 High mortality among patients with heroin addiction who discontinued buprenorphine treatment has been reported.27 The largest US epidemiological study of mood, anxiety and substance use disorders had a special warning by the authors: suicides may occur discontinuation of opiates in stable patient populations.28 These observations suggest endorphin specific neuroprotection for some vulnerable subgroups (Table 2).29
Brains of suicide victims are endorphin depleted.42 |
Endorphin agonists are crucial for treating pain addiction and treatment refractory depression.4 |
20% death rate in one year among heroin addicts who discontinued buprenorphine.27 |
Alarmingly high suicide rates among patients with discontinued opiate treatment following practice closures.24‒26 |
Table 2 Endorphin (opiates): Neurobiology
Pain depression and addiction share common pathways
Evidence of abnormal endogenous opioid neurotransmission in people with impulsiveness30 evidences of dysregulation of endogenous endorphins in major depression and women31 a high comorbidity between addiction and depression28 and also between pain and depression32 and suicide33 have been shown. Methadone, buprenorphine and heroine intramuscular are endorphin agonists to treat addictive disorders. The observations that opiates are effective to treat pain and addiction, high comorbidity of pain and depression, and of addiction and depression suggest common pathways in the genesis of pain addiction and depression. Endorphin function is involved in responses to diverse input such as exercise, pain, music and cocaine. Music and exercise seem to promote prefrontal cortex function.10,34 Naltrexone a morphine antagonist can block the effects induced by music10 and morphine like substances dampen pain.8 The opposite is true for pain and cocaine. Neuroimaging Atrophy with chronic pain35,36 and neurotoxicity with cocaine4 have been shown by neuroimaging studies. In summary endorphin agonists have mediating influence on prefrontal cortex function.
CDC’s scientific misrepresentations wrongly attribute an epidemic of overdose deaths to prescription pain medications. CDC without any scientific evidence wrongly broadcasts an epidemic of steadily rising overdose deaths to prescription pain medications. This is an egregious scientific misrepresentation. Association is not causation. Both the number of prescription medication overdose deaths and prescription pain medication overdose deaths increased at the same rate. From 2011 to 2013 the percentage of prescription pain medication deaths versus overall overdose deaths decreased. CDC wrongly and unscientifically attributed heroin addiction to prescription pain medications based upon a flawed study of people with heroin addiction and their past exposure to pain medications. According to the Institute of Medicine Report there are 110 million Americans with chronic pain. This large number may reflect multiple social medical realities industrial and traffic accidents, wars and longer longevity with cancer and other disorders-and has greatly increased the number of people who may benefit from prescription pain medications. Centers for Disease Control and Prevention (CDC) have published numerous warnings of a deadly epidemic of deaths from prescription painkiller overdoses. On November 4, 2015 DEA acting administrator Chuck Rosenberg warned the public and stated, “guns are safer than prescription drugs”. He declared that in 2013 more people died from a drug overdose then guns and more than half of those were prescription painkillers and heroin.
Is it possible that the chaos theory, the butterfly effect and the sensitive dependence of complex systems on initial error37 (Table 4) may explain the US heroin epidemic? Is it possible that man-made interventions interfering with efficient and optimal delivery of prescription opiates for a large population of people with chronic pain addiction and treatment refractory depression has been a crucial catalyst in triggering the heroine epidemic? There is no evidence of a causal link between the increasing overdose death rates and prescription pain medications. The CDC warning of an opiate prescription overdose epidemic destroying America citing 48.000 deaths or 9 deaths per 100.000 populations in 2014 is misleading.1 The actual number for prescription opiates is 4.3 per100.000 population because the CDC figures include illicit drugs (fentanyl and heroin) (Figure 1) (Figure 2). The observed increase in overdose deaths seems to be of multifactorial origin and may reflect recording errors, the increased numbers of people with chronic pain and mental illness, the larger number of over the counter pain medications etc.
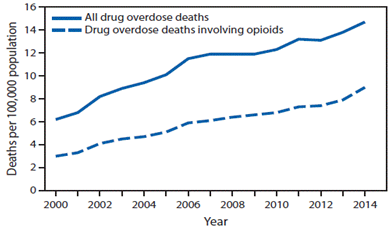
Figure 1 Age-adjusted rate* of drug overdose deaths† and drug overdose deaths involving opioids§,¶-United States, 2000–2014.
Source National vital statistics system, mortality file.

Figure 2 Drug overdose deaths* involving opioids†,§ by type of opioid¶-United States, 2000–2014.
Source National vital statistics system, mortality file.
From 2000 to 2014 heroin deaths jumped from 0.7 per 100.000 populations to 3.4, almost a fivefold increase. During the same period, deaths from opiate prescriptions rose from 3 to 4.3. Of significance the percentage of deaths from prescription opiates relative to the total overdose deaths dropped. This is consistent with the effects of regulatory measures to contain prescription opiates. The CDC warnings of a causal association between prescription pain medications and an epidemic of overdose deaths seem to lack scientific validity for no evidence has been offered to indicate that the association is causative. The highly publicized association between the use of prescription pain medications and heroin addiction is based upon flawed data: the study subjects were not patients taking prescription opiates prescribed by their physicians for a specific psychiatric condition or chronic pain (Figure 4A & B). CDC claim that use of prescription pain medications may lead to heroin addiction is flawed and based upon a scientific misrepresentation of an inconsequential association as causation (Table 4). Public statements by CDC and DEA officials scapegoating paying doctors or prescribing prescription pain medications have created an extremely hostile environment for Americans in need of prescription pain medications.
Inadequate or less than optimal opiate treatment for large number of people with addiction, chronic pain and treatment refractory depression from 2000 to 2014 include the following: 9000 physicians who prescribed opiates were rendered inactive37‒41 at a time when The Institute of medicine declared that inadequate treatment was a major challenge for 110 million Americans with chronic pain (Table 3). Medically unnecessary preconditions seem to interfere with efficient and optimal delivery of crucial therapeutic medications for chronic pain and addiction. For instance in the US methadone maintenance requires daily medical visits and travel restrictions. The number of physicians certified to prescribe buprenorphine is restricted.42,43 And slow acting i.m. heroin is unavailable the United States. An independent observation consistent with an association between regulatory restrictions on prescription opiates and the heroin epidemic seems to be the statistically significant correlation coefficient r=0.9 between the suicide and heroin epidemics from 2000 to 2014 (Table 4). Pharmacologically prescription opiates are the shared independent variable (Figure 4A & B). Thus the regulatory influences governing prescription opiates seem to be crucial for both epidemics.
People in need of pain treatment: 110 million |
Physicians treating pain: 6000 |
Physicians under investigation every year: 600 |
Pain physicians delicensed: 9000 |
Table 3 Pain treatment (2000 to 2014)*
*DEA does not provide specific data of the annual and total number of physicians investigated or prosecuted. The above numbers are the best educated estimates based upon available information from diverse sources.
Complex system: US health care. |
Initial condition: measures to curb prescription opiates. |
Sensitive dependence on a crucial variable: prescription opiates. |
Final state: Heroin epidemic. |
Table 4 The butterfly effect and the heroin epidemic*
*The idea, that small causes may have large effects in general and in weather specifically, was used from Henri Poincare to Norbert Wiener. In chaos theory, the butterfly effect is the sensitive dependence on initial conditions in which a small change in one state of a complex system can result in large differences in a later state. The butterfly effect coined by Ed Lorenz is derived from the metaphorical example of a hurricane being influenced by minor perturbations such as the flapping of the wings of a distant butterfly several weeks earlier.
An independent observation consistent with an association between regulatory restrictions on prescription opiates and the heroin epidemic seems to be the statistically significant correlation coefficient r=0.9 between the suicide and heroin epidemics from 2000 to 2014 (Table 5). Pharmacologically prescription opiates are the shared independent variable. Man-made interventions which resulted in reduction of access to treatment with opiates-might have contributed to the US heroin epidemic.
Year |
Heroine |
Suicide |
2000 |
0.7 |
10.5 |
2005 |
0.7 |
11 |
2008 |
0.9 |
11.6 |
2010 |
1 |
12.1 |
2011 |
1.3 |
12.3 |
2014 |
3.4 |
13 |
Table 5 2009–2014–US Deaths from Suicide and Heroine per 100.000 populations
r=0.9
None.
The author declares that there is no conflict of interest.

©2018 Salerian. This is an open access article distributed under the terms of the, which permits unrestricted use, distribution, and build upon your work non-commercially.